Tuesday Poster Session
Category: GI Bleeding
P5208 - Yield of Inpatient Colonoscopy in the Presentation of Lower Gastrointestinal Bleeding
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- DA
Dinkar Ahuja, MD (he/him/his)
Loyola University Medical Center
Chicago, IL
Presenting Author(s)
Dinkar Ahuja, MD1, Dejan Micic, MD2, Mohammed Abourahma, MD3
1Loyola University Medical Center, Chicago, IL; 2Loyola University Medical Center, Maywood, IL; 3Loyola University Medical Center, Willowbrook, IL
Introduction: Lower gastrointestinal bleeding (LGIB) is a common cause of hospital admission, often prompting endoscopic evaluation. Diverticular bleeding is the leading etiology, accounting for an estimated 26–64% of LGIB cases. The diagnostic yield and therapeutic impact of colonoscopy remain uncertain. Current ACG guidelines suggest colonoscopy may be deferred in patients with self-limited LGIB if a high-quality colonoscopy within 12 months demonstrated diverticulosis. Our study aims to evaluate the diagnostic yield and rate of intervention during colonoscopy for diverticular bleeding.
Methods: In this retrospective cohort study, we included patients aged >18 years admitted between 1/2014 and 12/2024 for hematochezia or melena who underwent colonoscopy demonstrating diverticulosis. Patients with diverticulitis, IBD, colorectal cancer, radiation proctitis, or cirrhosis were excluded. The primary outcome was detection of new advanced colonic neoplasia (ACN), defined as adenomas ≥1 cm or with ≥25% villous features and histologically confirmed colorectal cancer (CRC). The secondary outcome was stigmata of bleeding requiring endoscopic therapy, defined as active bleeding, visible vessel, adherent clot, or presumptive bleeding treated endoscopically. Pairwise comparisons were made using Fisher’s exact test.
Results: A total of 333 charts were reviewed, 182 met inclusion criteria. Median age was 74 years (IQR: 65.0–81.0), and 50.5% were male. One quarter had a colonoscopy in the past year, while 56 (30.8%) had no prior colonoscopy. Median time to colonoscopy was 45.0 hours (IQR: 30.0–65.2) (Table 1). ACN was identified in 0 patients (0%) with a colonoscopy in the past year, 1 (5.0%) at 1–2 years, 0 (0%) at 2–5 years, 1 (3.0%) if a colonoscopy was performed over 5 years ago. Eight (14.3%) had ACN with no prior colonoscopy. Only one patient (1.8%) without a prior colonoscopy was diagnosed with CRC. The ACN detection rate for those with a colonoscopy in the past year was less than those without a prior colonoscopy (p=0.034) (Table 2). Stigmata of bleeding requiring intervention were found in 7 patients (3.8%), all treated with hemostatic clips.
Discussion: In this cohort, ACN detection rates were reduced in those with a recent prior colonoscopy and the rate of intervention was < 5%. These findings support the ACG guidelines and suggest that inpatient colonoscopy may be of limited value in diverticular bleeding with a high-quality colonoscopy within 1 year and potentially longer given the low rate of ACN.
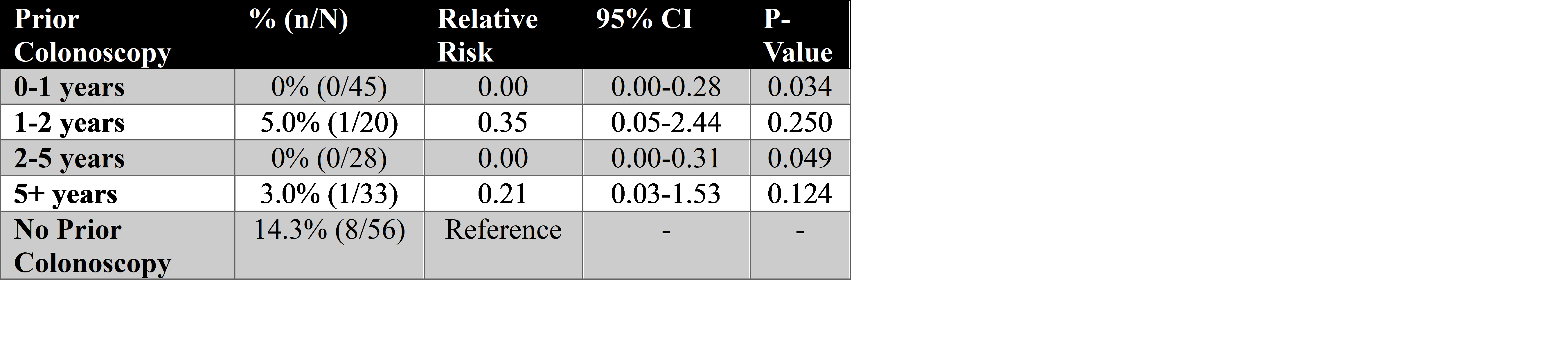
Figure: Table 1: Demographics, colonoscopy characteristics, findings and interventions
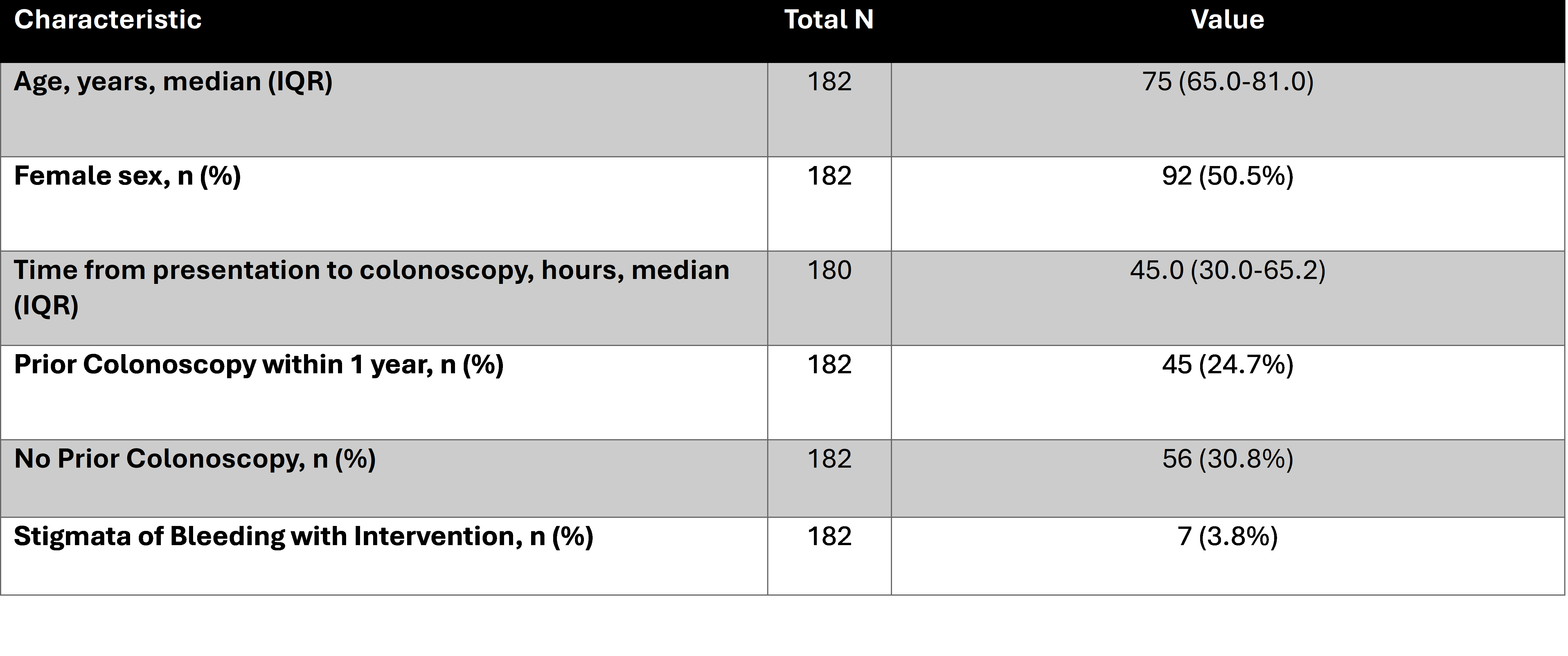
Figure: Table 2: Rate of advanced colonic neoplasia by duration since preceding colonoscopy
Disclosures:
Dinkar Ahuja indicated no relevant financial relationships.
Dejan Micic indicated no relevant financial relationships.
Mohammed Abourahma indicated no relevant financial relationships.
Dinkar Ahuja, MD1, Dejan Micic, MD2, Mohammed Abourahma, MD3. P5208 - Yield of Inpatient Colonoscopy in the Presentation of Lower Gastrointestinal Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Loyola University Medical Center, Chicago, IL; 2Loyola University Medical Center, Maywood, IL; 3Loyola University Medical Center, Willowbrook, IL
Introduction: Lower gastrointestinal bleeding (LGIB) is a common cause of hospital admission, often prompting endoscopic evaluation. Diverticular bleeding is the leading etiology, accounting for an estimated 26–64% of LGIB cases. The diagnostic yield and therapeutic impact of colonoscopy remain uncertain. Current ACG guidelines suggest colonoscopy may be deferred in patients with self-limited LGIB if a high-quality colonoscopy within 12 months demonstrated diverticulosis. Our study aims to evaluate the diagnostic yield and rate of intervention during colonoscopy for diverticular bleeding.
Methods: In this retrospective cohort study, we included patients aged >18 years admitted between 1/2014 and 12/2024 for hematochezia or melena who underwent colonoscopy demonstrating diverticulosis. Patients with diverticulitis, IBD, colorectal cancer, radiation proctitis, or cirrhosis were excluded. The primary outcome was detection of new advanced colonic neoplasia (ACN), defined as adenomas ≥1 cm or with ≥25% villous features and histologically confirmed colorectal cancer (CRC). The secondary outcome was stigmata of bleeding requiring endoscopic therapy, defined as active bleeding, visible vessel, adherent clot, or presumptive bleeding treated endoscopically. Pairwise comparisons were made using Fisher’s exact test.
Results: A total of 333 charts were reviewed, 182 met inclusion criteria. Median age was 74 years (IQR: 65.0–81.0), and 50.5% were male. One quarter had a colonoscopy in the past year, while 56 (30.8%) had no prior colonoscopy. Median time to colonoscopy was 45.0 hours (IQR: 30.0–65.2) (Table 1). ACN was identified in 0 patients (0%) with a colonoscopy in the past year, 1 (5.0%) at 1–2 years, 0 (0%) at 2–5 years, 1 (3.0%) if a colonoscopy was performed over 5 years ago. Eight (14.3%) had ACN with no prior colonoscopy. Only one patient (1.8%) without a prior colonoscopy was diagnosed with CRC. The ACN detection rate for those with a colonoscopy in the past year was less than those without a prior colonoscopy (p=0.034) (Table 2). Stigmata of bleeding requiring intervention were found in 7 patients (3.8%), all treated with hemostatic clips.
Discussion: In this cohort, ACN detection rates were reduced in those with a recent prior colonoscopy and the rate of intervention was < 5%. These findings support the ACG guidelines and suggest that inpatient colonoscopy may be of limited value in diverticular bleeding with a high-quality colonoscopy within 1 year and potentially longer given the low rate of ACN.
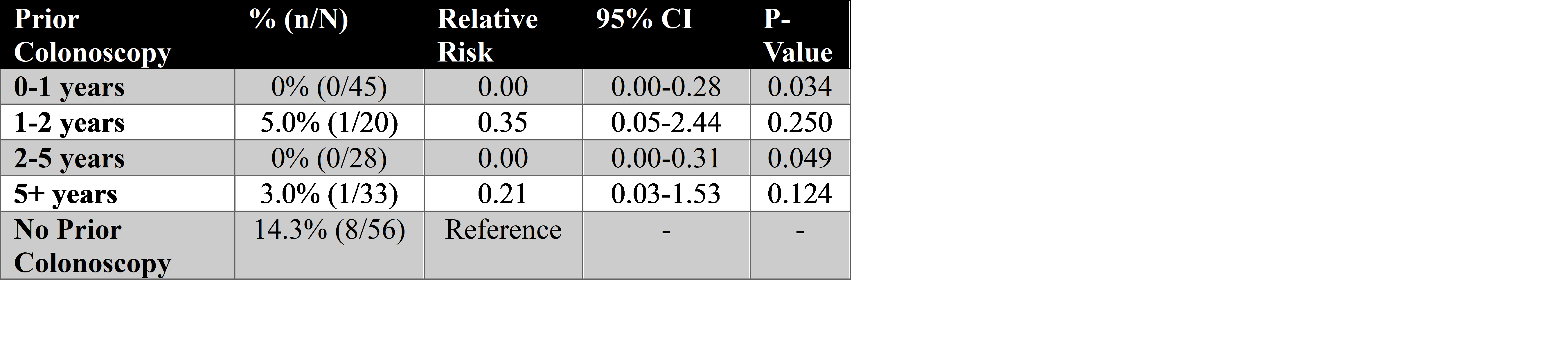
Figure: Table 1: Demographics, colonoscopy characteristics, findings and interventions
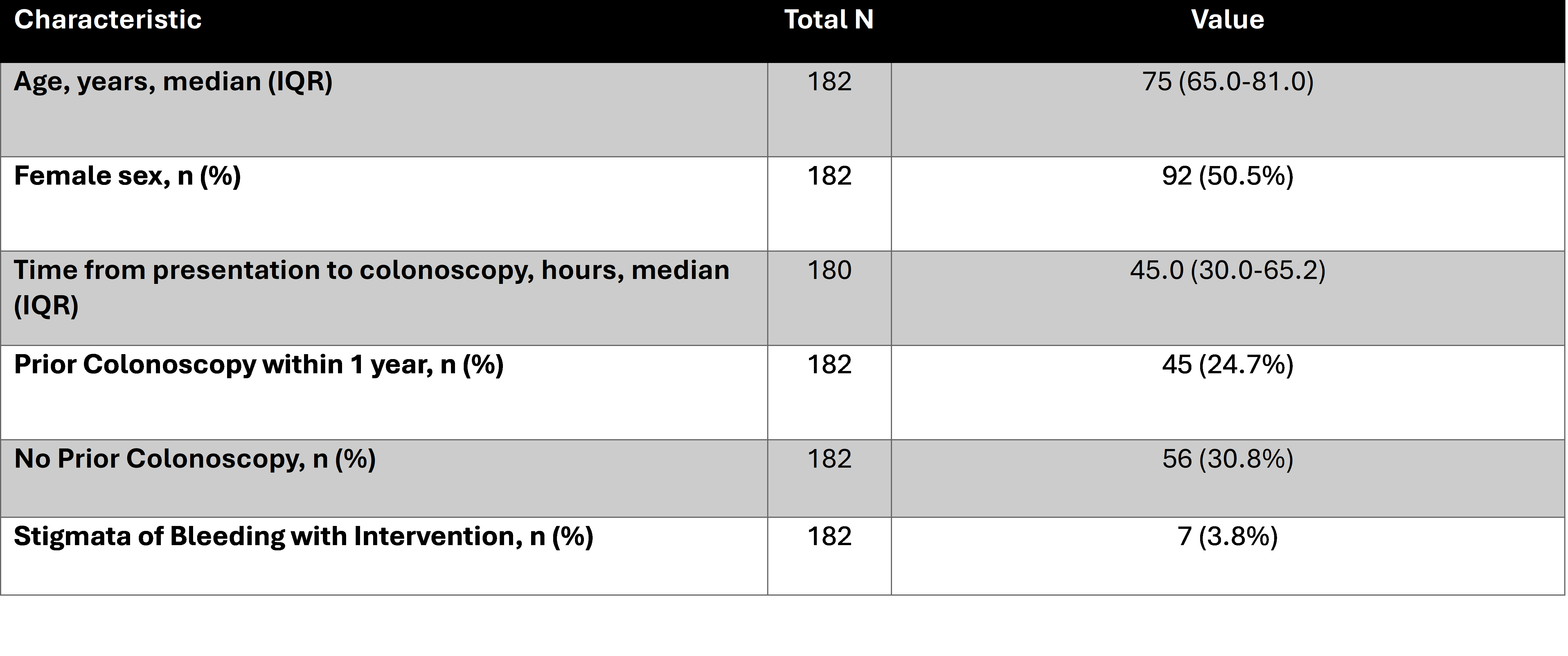
Figure: Table 2: Rate of advanced colonic neoplasia by duration since preceding colonoscopy
Disclosures:
Dinkar Ahuja indicated no relevant financial relationships.
Dejan Micic indicated no relevant financial relationships.
Mohammed Abourahma indicated no relevant financial relationships.
Dinkar Ahuja, MD1, Dejan Micic, MD2, Mohammed Abourahma, MD3. P5208 - Yield of Inpatient Colonoscopy in the Presentation of Lower Gastrointestinal Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

