Tuesday Poster Session
Category: GI Bleeding
P5206 - Tumor-Related Upper GI Bleeding in the Era of Hemostatic Sprays: Progress or Plateau?
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Rand Alkalbani, MD (she/her/hers)
INOVA Fairfax Hospital, VA
Presenting Author(s)
Rand Alkalbani, MD1, Farhan Azad, DO1, Kelly M. Vo, DO2, Amolika Gupta, MD3, Martin Banks, MD4, Adaobi Ahanotu, MD5, Marwan S. Abougergi, MD6
1INOVA Fairfax Hospital, Fairfax, VA; 2Walter Reed National Military Medical Center, Bethesda, MD; 3Inova Fairfax Medical Campus, Vienna, VA; 4Bayhealth Medical Center - - Dover, DE, Dover, DE; 5University of Maryland Medical Center, Hyattsville, MD; 6INOVA Fairfax Hospital, Falls Church, VA
Introduction: Gastrointestinal (GI) bleeding is one of the serious and potentially life-threatening complications of upper GI tumors. Traditional endoscopic hemostatic methods have a low success rate in this setting. Hemostatic powder became available in 2018 and was seen by many as a game changer. However, longitudinal data on hemostatic powder real-world treatment outcome in this setting is limited. We aim to bridge this gap using the National Inpatient Sample database.
Methods: Adult patients with a principal diagnosis of hemorrhage from an esophageal, gastric or small intestinal tumor were identified yearly from 2016 to 2022. Elective admissions were excluded. The primary outcome was age and sex adjusted in-hospital mortality. Secondary outcomes were 1-treatment modalities: endoscopic therapy, interventional radiology-guided embolization of a vessel (IR Embolization) and extracorporeal radiation therapy, 2-resource utilization: length of stay (LOS), and total hospitalization costs, and charges. Charges and costs were adjusted for inflation using the consumer price index.
Results: 375,440 patients were included in the study. Table 1 summarizes the patient’s characteristics. The mean age was 67 years. The majority of patients were Caucasian males of lower income, insured by Medicare and treated at large urban teaching hospitals.
The study outcomes are presented in Table 2. From 2016 to 2022, the in-hospital mortality rate increased by 25%. The proportion of patients who received an inpatient EGD was constant and low (17%–19%). The same was found for early EGD (within 24 hours of admission). The rate of endoscopic therapy increased by 75% from 2016 to 2022. Extracorporeal radiation therapy rates were low and further decreased over the study period. IR embolization rate were also low but constant. The mean LOS increased by 9% over the study period, while the mean total hospitalization costs and charges increased by 14% and 18%, respectively.
Discussion: From 2016 to 2022, the use of endoscopic therapy including hemostatic powder for upper GI tumor hemorrhage increased significantly. However, this rise did not yield any measurable reduction in in-hospital mortality, which trended upward over the study period. The higher rates of endoscopic intervention were associated with increased resource utilization and healthcare costs. These findings highlight the need for more effective and evidence-based modalities to achieve hemostasis in patients with tumor-related upper GI bleeding.
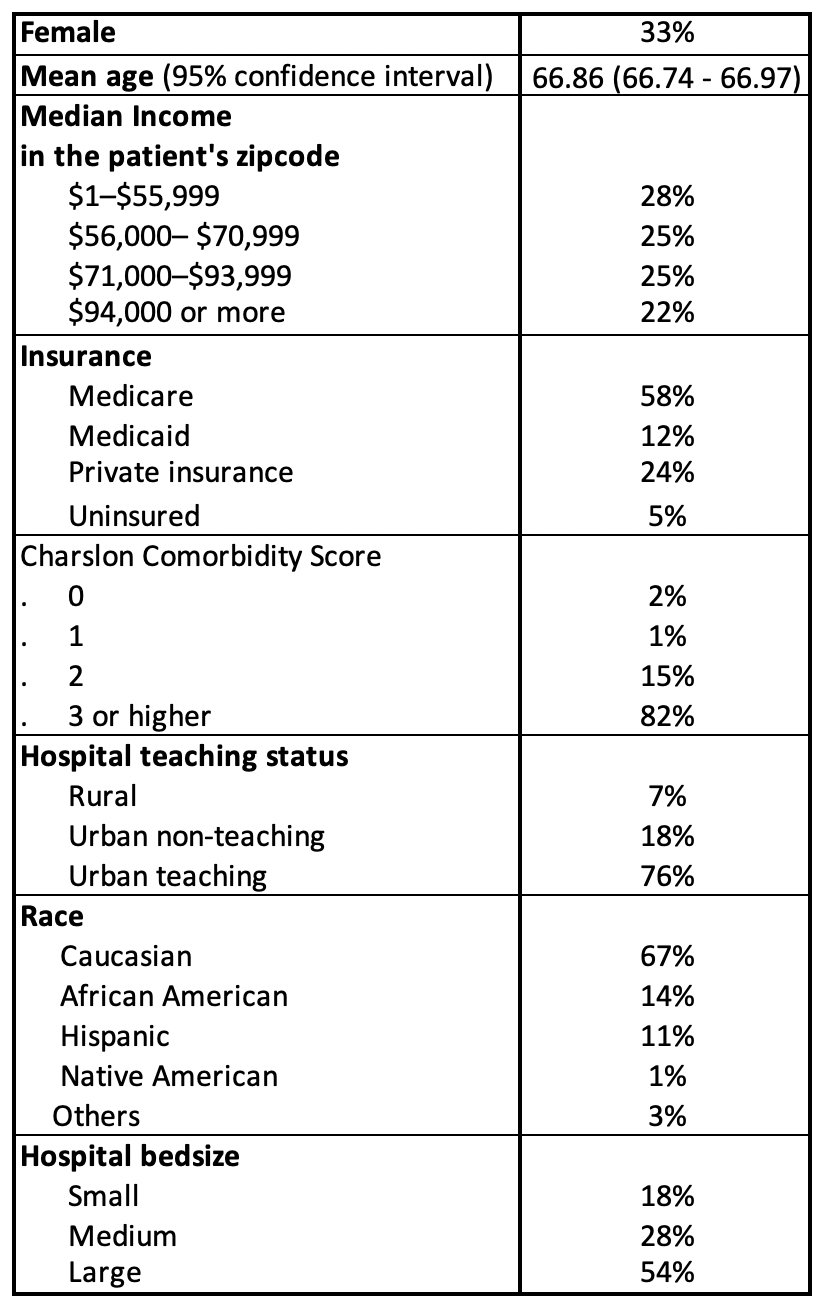
Figure: Table 1: Patients' Characteristics
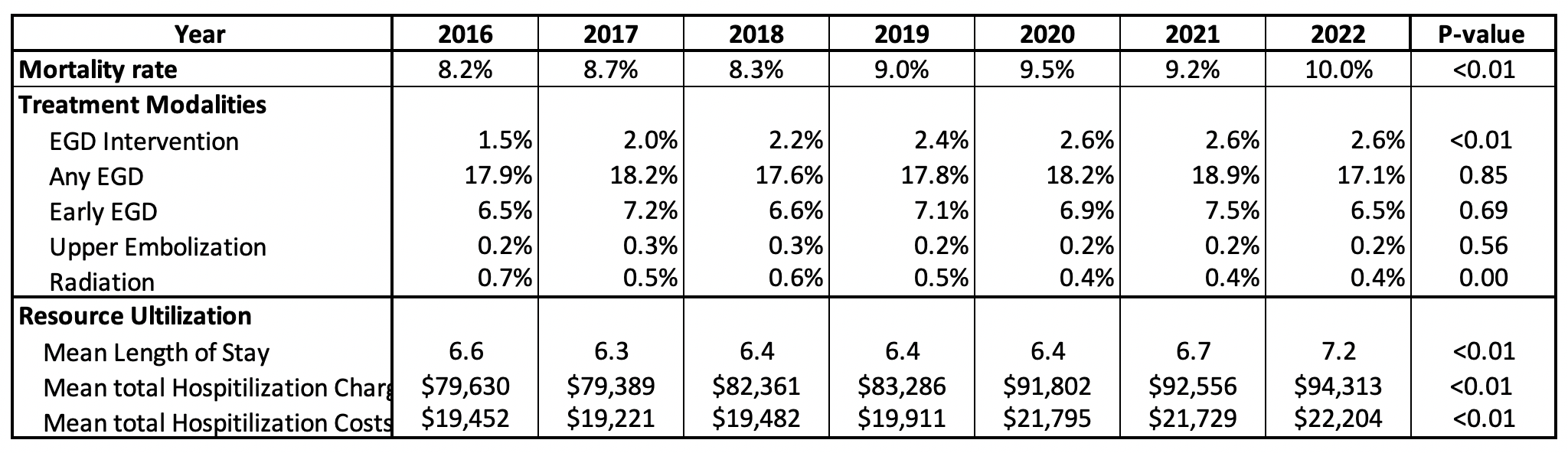
Figure: Table 2: Study Outcomes from 2016 to 2022
Disclosures:
Rand Alkalbani indicated no relevant financial relationships.
Farhan Azad indicated no relevant financial relationships.
Kelly Vo indicated no relevant financial relationships.
Amolika Gupta indicated no relevant financial relationships.
Martin Banks indicated no relevant financial relationships.
Adaobi Ahanotu indicated no relevant financial relationships.
Marwan Abougergi indicated no relevant financial relationships.
Rand Alkalbani, MD1, Farhan Azad, DO1, Kelly M. Vo, DO2, Amolika Gupta, MD3, Martin Banks, MD4, Adaobi Ahanotu, MD5, Marwan S. Abougergi, MD6. P5206 - Tumor-Related Upper GI Bleeding in the Era of Hemostatic Sprays: Progress or Plateau?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1INOVA Fairfax Hospital, Fairfax, VA; 2Walter Reed National Military Medical Center, Bethesda, MD; 3Inova Fairfax Medical Campus, Vienna, VA; 4Bayhealth Medical Center - - Dover, DE, Dover, DE; 5University of Maryland Medical Center, Hyattsville, MD; 6INOVA Fairfax Hospital, Falls Church, VA
Introduction: Gastrointestinal (GI) bleeding is one of the serious and potentially life-threatening complications of upper GI tumors. Traditional endoscopic hemostatic methods have a low success rate in this setting. Hemostatic powder became available in 2018 and was seen by many as a game changer. However, longitudinal data on hemostatic powder real-world treatment outcome in this setting is limited. We aim to bridge this gap using the National Inpatient Sample database.
Methods: Adult patients with a principal diagnosis of hemorrhage from an esophageal, gastric or small intestinal tumor were identified yearly from 2016 to 2022. Elective admissions were excluded. The primary outcome was age and sex adjusted in-hospital mortality. Secondary outcomes were 1-treatment modalities: endoscopic therapy, interventional radiology-guided embolization of a vessel (IR Embolization) and extracorporeal radiation therapy, 2-resource utilization: length of stay (LOS), and total hospitalization costs, and charges. Charges and costs were adjusted for inflation using the consumer price index.
Results: 375,440 patients were included in the study. Table 1 summarizes the patient’s characteristics. The mean age was 67 years. The majority of patients were Caucasian males of lower income, insured by Medicare and treated at large urban teaching hospitals.
The study outcomes are presented in Table 2. From 2016 to 2022, the in-hospital mortality rate increased by 25%. The proportion of patients who received an inpatient EGD was constant and low (17%–19%). The same was found for early EGD (within 24 hours of admission). The rate of endoscopic therapy increased by 75% from 2016 to 2022. Extracorporeal radiation therapy rates were low and further decreased over the study period. IR embolization rate were also low but constant. The mean LOS increased by 9% over the study period, while the mean total hospitalization costs and charges increased by 14% and 18%, respectively.
Discussion: From 2016 to 2022, the use of endoscopic therapy including hemostatic powder for upper GI tumor hemorrhage increased significantly. However, this rise did not yield any measurable reduction in in-hospital mortality, which trended upward over the study period. The higher rates of endoscopic intervention were associated with increased resource utilization and healthcare costs. These findings highlight the need for more effective and evidence-based modalities to achieve hemostasis in patients with tumor-related upper GI bleeding.
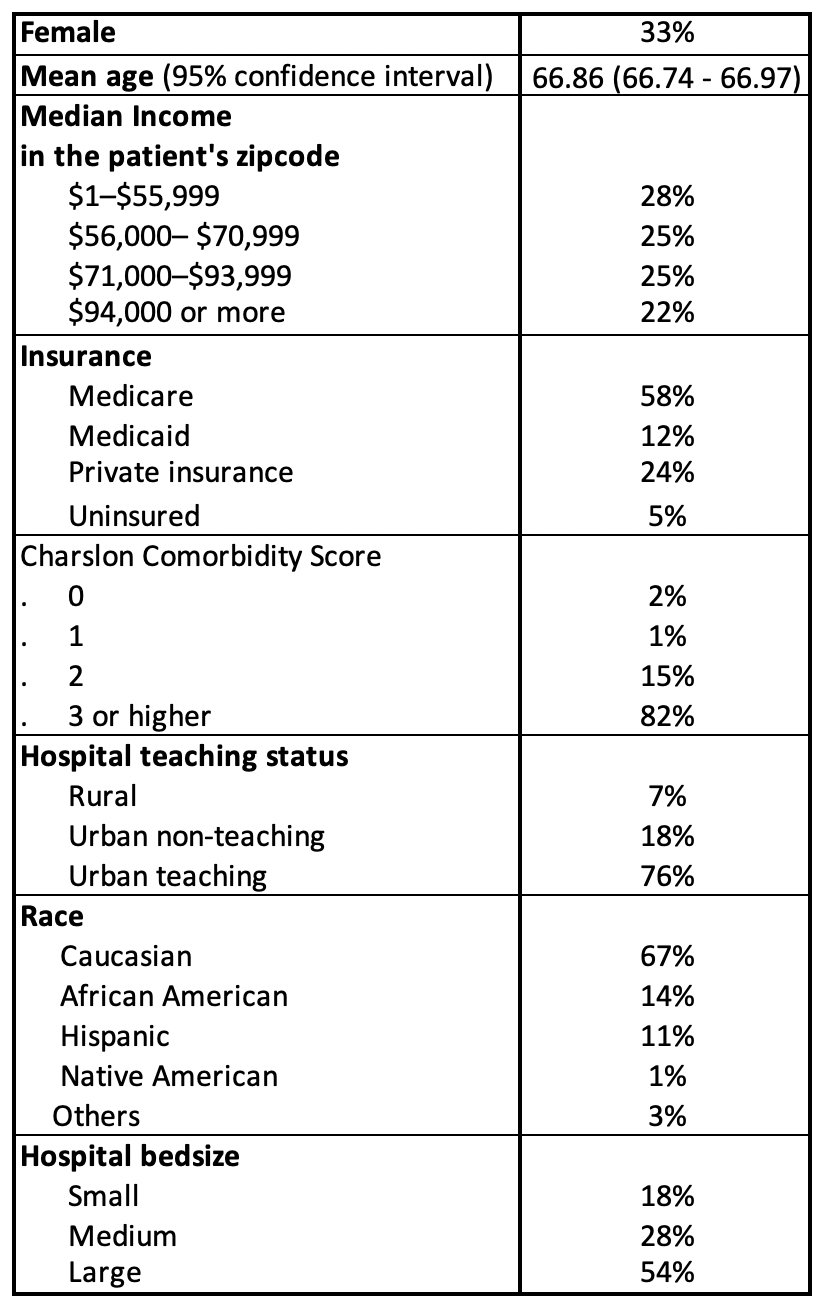
Figure: Table 1: Patients' Characteristics
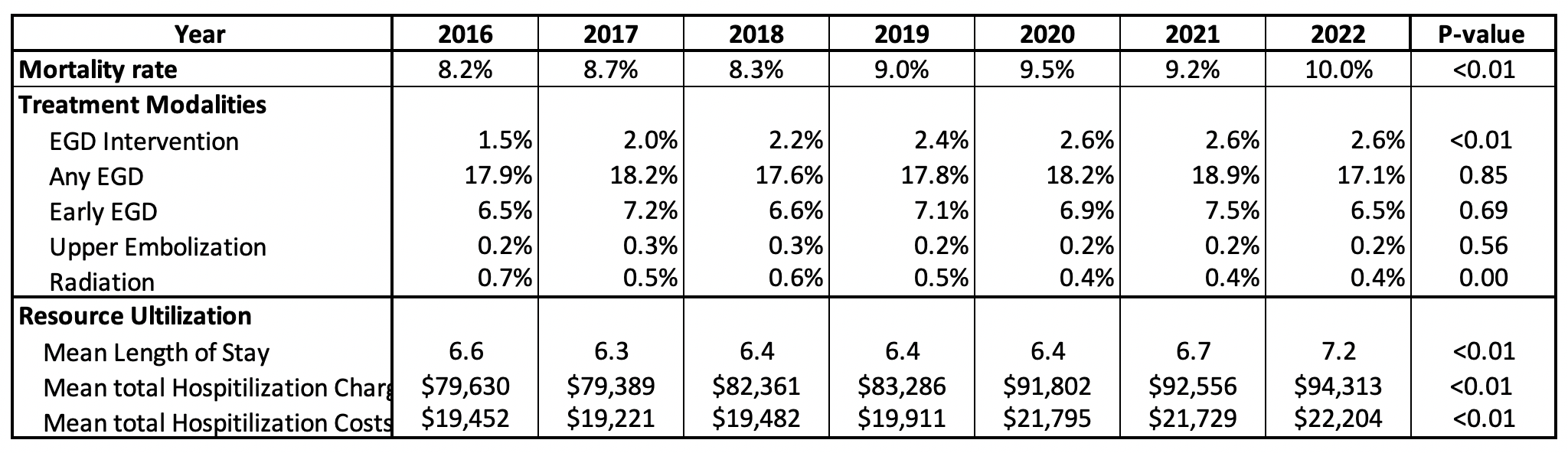
Figure: Table 2: Study Outcomes from 2016 to 2022
Disclosures:
Rand Alkalbani indicated no relevant financial relationships.
Farhan Azad indicated no relevant financial relationships.
Kelly Vo indicated no relevant financial relationships.
Amolika Gupta indicated no relevant financial relationships.
Martin Banks indicated no relevant financial relationships.
Adaobi Ahanotu indicated no relevant financial relationships.
Marwan Abougergi indicated no relevant financial relationships.
Rand Alkalbani, MD1, Farhan Azad, DO1, Kelly M. Vo, DO2, Amolika Gupta, MD3, Martin Banks, MD4, Adaobi Ahanotu, MD5, Marwan S. Abougergi, MD6. P5206 - Tumor-Related Upper GI Bleeding in the Era of Hemostatic Sprays: Progress or Plateau?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
