Tuesday Poster Session
Category: General Endoscopy
P5156 - Massive Gastric Distension: A Rare Life-Threatening Emergency
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Hira Khan, MD (she/her/hers)
University of Connecticut Health Center
Farmington, CT
Presenting Author(s)
Hira Khan, MD1, Karim Al Annan, MD2, Sarah Canavan, MD3
1University of Connecticut Health Center, Farmington, CT; 2University of Connecticut Health Center, Hartford, CT; 3Hartford HealthCare, New London, CT
Introduction: Massive gastric distension and catastrophic gastric perforation have been reported in individuals with disability, presenting challenges in diagnosis and management. We present a case of massive gastric distention with unique endoscopic findings.
Case Description/
Methods: A 68-year-old non-verbal female with severe developmental delay and a history of small bowel obstruction presented from a skilled nursing facility (SNF) with abdominal distension and decreased oral intake. Vitals showed fever (101.1°F), hypertension (155/107 mmHg), and tachycardia (108 bpm). Physical exam revealed abdominal distension without peritoneal signs. Labs showed lactic acidosis (6.3 mg/dL), leukocytosis (23.0 x10³/μL), and elevated lipase (828 U/L). Abdominal CT with IV contrast showed a massively dilated stomach full of contents (Fig 1), ascites, and a non-inflamed pancreas. Volvulus and obstruction were not present.
Nasogastric decompression was attempted, but unsuccessful due to patient distress and tube coiling. Sedation for endoscopy to aspirate gastric contents and place an NGT was too high risk for aspiration given the tremendous gastric distension. After a multi-disciplinary discussion, an emergent percutaneous gastrostomy tube was placed by IR, and 1300cc of material was drained. The patient was resuscitated with IV fluids, and stabilized. Eventual upper endoscopy revealed a congested, ulcerated, hemorrhagic-appearing mucosa in the cardia, fundus, and body of the stomach (Fig 2). Biopsy showed moderate chronic inflammation and regenerative changes favoring reactive gastropathy. The scope easily traversed the pylorus, and there was no obstructive lesion in the examined upper GI tract. The gastrostomy tube was later converted to a gastro-jejunostomy tube, yet dilation remained on subsequent imaging.
Discussion: Massive gastric distension can be a life threatening emergency in disabled adults, progressing to ischemia, perforation, sepsis, or compressive cardiovascular collapse. The etiology is unknown but may be related to non-volitional air swallowing and motility differences in these patients, compounded by communication barriers. Early recognition and intervention is crucial in this patient population.

Figure: Figure 1. CT Abdomen & Pelvis showing massive gastric distension.
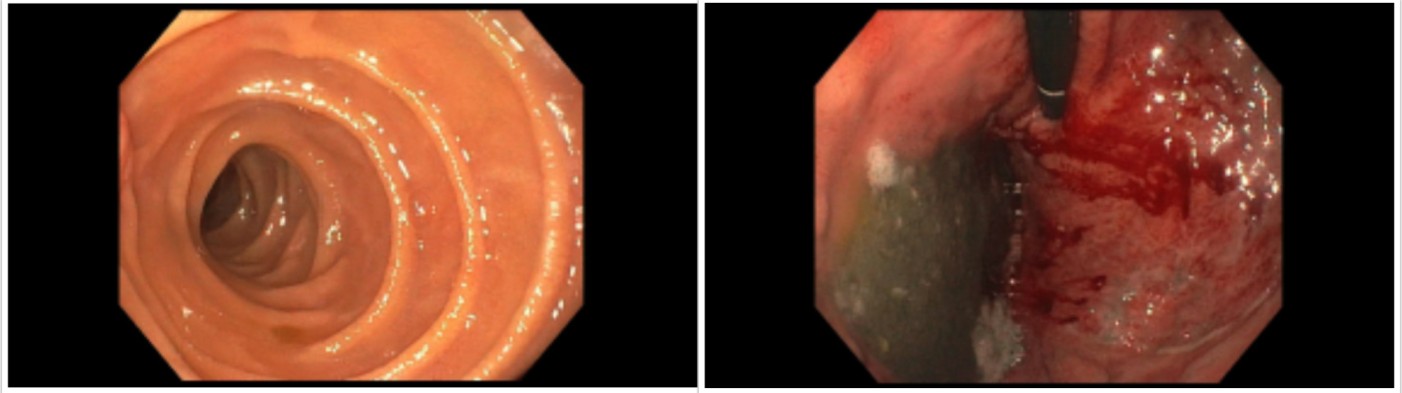
Figure: Figure 2. Endoscopy findings congested and hemorrhagic-appearing mucosa in the stomach.
Disclosures:
Hira Khan indicated no relevant financial relationships.
Karim Al Annan indicated no relevant financial relationships.
Sarah Canavan indicated no relevant financial relationships.
Hira Khan, MD1, Karim Al Annan, MD2, Sarah Canavan, MD3. P5156 - Massive Gastric Distension: A Rare Life-Threatening Emergency, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Connecticut Health Center, Farmington, CT; 2University of Connecticut Health Center, Hartford, CT; 3Hartford HealthCare, New London, CT
Introduction: Massive gastric distension and catastrophic gastric perforation have been reported in individuals with disability, presenting challenges in diagnosis and management. We present a case of massive gastric distention with unique endoscopic findings.
Case Description/
Methods: A 68-year-old non-verbal female with severe developmental delay and a history of small bowel obstruction presented from a skilled nursing facility (SNF) with abdominal distension and decreased oral intake. Vitals showed fever (101.1°F), hypertension (155/107 mmHg), and tachycardia (108 bpm). Physical exam revealed abdominal distension without peritoneal signs. Labs showed lactic acidosis (6.3 mg/dL), leukocytosis (23.0 x10³/μL), and elevated lipase (828 U/L). Abdominal CT with IV contrast showed a massively dilated stomach full of contents (Fig 1), ascites, and a non-inflamed pancreas. Volvulus and obstruction were not present.
Nasogastric decompression was attempted, but unsuccessful due to patient distress and tube coiling. Sedation for endoscopy to aspirate gastric contents and place an NGT was too high risk for aspiration given the tremendous gastric distension. After a multi-disciplinary discussion, an emergent percutaneous gastrostomy tube was placed by IR, and 1300cc of material was drained. The patient was resuscitated with IV fluids, and stabilized. Eventual upper endoscopy revealed a congested, ulcerated, hemorrhagic-appearing mucosa in the cardia, fundus, and body of the stomach (Fig 2). Biopsy showed moderate chronic inflammation and regenerative changes favoring reactive gastropathy. The scope easily traversed the pylorus, and there was no obstructive lesion in the examined upper GI tract. The gastrostomy tube was later converted to a gastro-jejunostomy tube, yet dilation remained on subsequent imaging.
Discussion: Massive gastric distension can be a life threatening emergency in disabled adults, progressing to ischemia, perforation, sepsis, or compressive cardiovascular collapse. The etiology is unknown but may be related to non-volitional air swallowing and motility differences in these patients, compounded by communication barriers. Early recognition and intervention is crucial in this patient population.

Figure: Figure 1. CT Abdomen & Pelvis showing massive gastric distension.
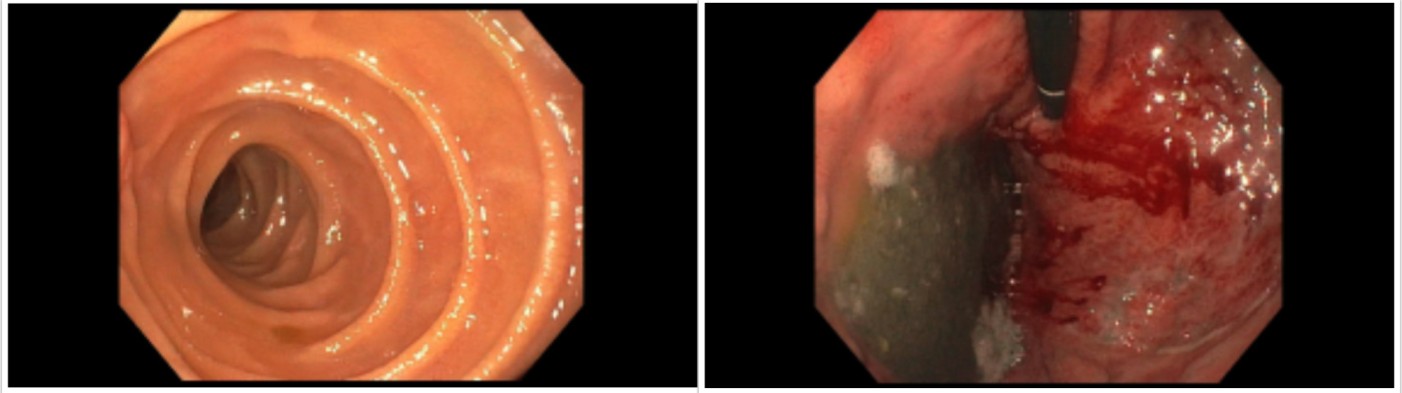
Figure: Figure 2. Endoscopy findings congested and hemorrhagic-appearing mucosa in the stomach.
Disclosures:
Hira Khan indicated no relevant financial relationships.
Karim Al Annan indicated no relevant financial relationships.
Sarah Canavan indicated no relevant financial relationships.
Hira Khan, MD1, Karim Al Annan, MD2, Sarah Canavan, MD3. P5156 - Massive Gastric Distension: A Rare Life-Threatening Emergency, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
