Tuesday Poster Session
Category: General Endoscopy
P5138 - Closing In: A Comparative Analysis of the Safety and Effectiveness of Defect Closure Techniques in Colon Polyp Resection
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Olivia Reszczynski, MD (she/her/hers)
University of Virginia Medical Center
Charlottesville, VA
Presenting Author(s)
Award: ACG Presidential Poster Award
Olivia Reszczynski, MD1, Himesh Zaver, MD2, Jason Erno, MD1, Owen Battel, MD1, Aditya Singh, BS2, Gianna Stoleru, MD3, Tanya Wanchek, JD, PhD3, Wendy M. Novicoff, PhD4, Ross Buerlein, MD1, Andrew Copland, MD1
1University of Virginia Medical Center, Charlottesville, VA; 2University of Virginia Health, Charlottesville, VA; 3University of Virginia, Charlottesville, VA; 4University of Virginia School of Medicine, Charlottesville, VA
Introduction: Endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) are minimally invasive techniques for removing large polyps unsuitable for standard polypectomy. Delayed post-polypectomy bleeding occurs in 4–10% of cases but can be reduced with effective mucosal defect closure. This study aimed to assess the safety and efficacy of various defect closure techniques following large colon polyp resection.
Methods: This retrospective, single-center cohort study examined adult patients who underwent conventional (hot) EMR, underwater EMR, or ESD for colon polyps ≥ 20 mm. Defect closure techniques included through-the-scope clips (TTSC), through-the-scope suturing (TTSS), peptide-based hemostatic agent (HA), or combinations of these techniques.
Results: A total of 241 patients were included in this study (mean age 65.9 years, 48.1% female) (Table 1). Most patients (69.5%) were not on anticoagulation or antiplatelet therapy and the average ASA classification was 2.21 (1–4, SD 0.79). Polyps were mainly located in the right colon (75.8%), with an average polyp size of 33.72 mm (20–70, SD 11.9). Hot EMR was the most common technique (55.1%). Piecemeal resection was performed in 81.1% of cases, with complete polyp resection achieved in 91.0% of cases. Complete defect closure was successful in 97.5% of patients, with similar success rates across cohorts, except for the HA group (89.3%). Adverse events related to defect closure techniques were minimal, with 94.2% of cases (227 patients) experiencing no complications. Intraprocedural bleeding due to defect closure technique occurred in 5.8% of cases (14 patients), and was successfully managed by the end of each respective procedure. No perforations were observed across any technique cohort. The overall incidence of delayed bleeding was 2.9% (7 patients) and similar across cohorts (Table 2). The average time to delayed bleeding was 4.1 days (1–10, SD 3.54), with supportive care (3 cases) and colonoscopy (4 cases) as the primary management strategies.
Discussion: All closure techniques achieved similar complete closure success rates, with no significant difference between single-modality and combination closure techniques in terms of technical success or adverse events. These findings support the continued use of TTSC for defect closure while highlighting the potential for alternative techniques guided by provider expertise and polyp characteristics.
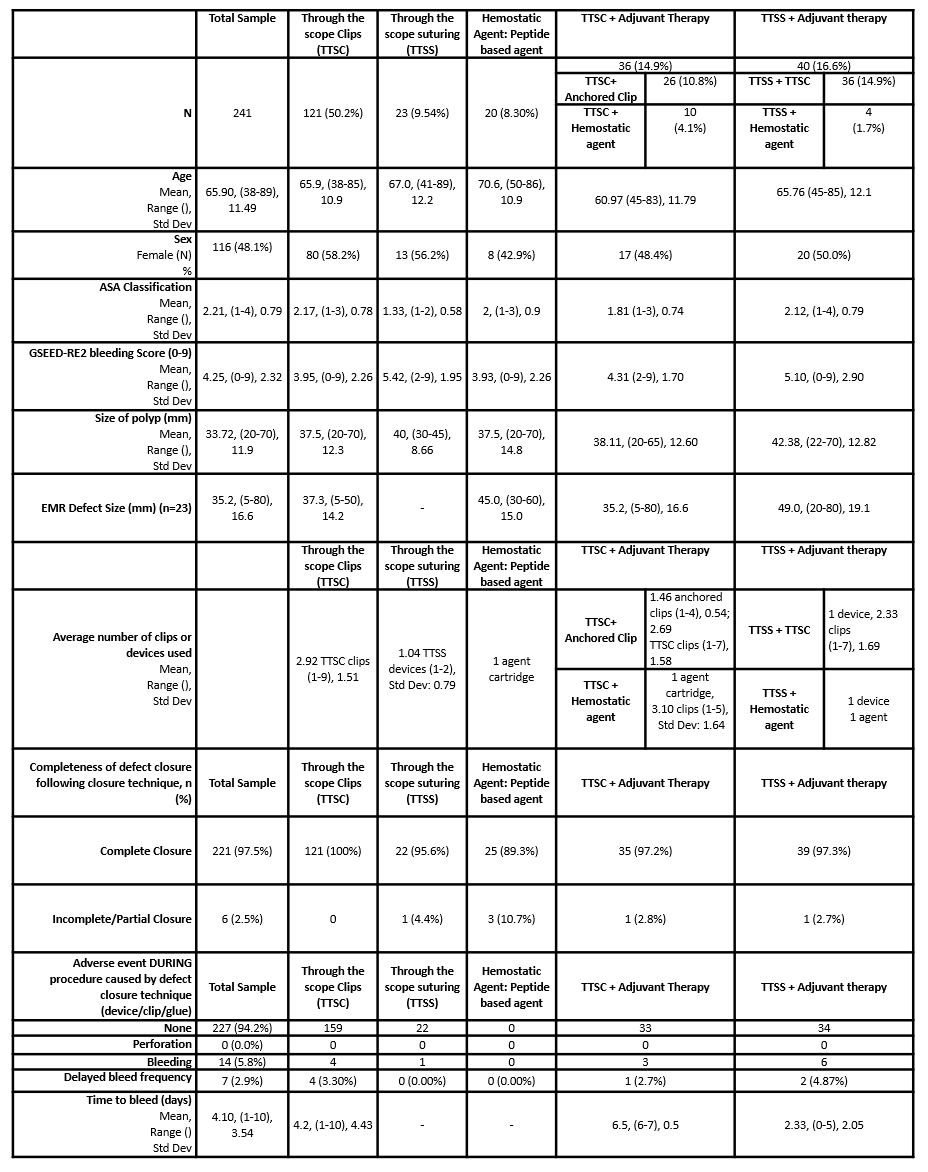
Figure: Table 1 Study Cohort Summary
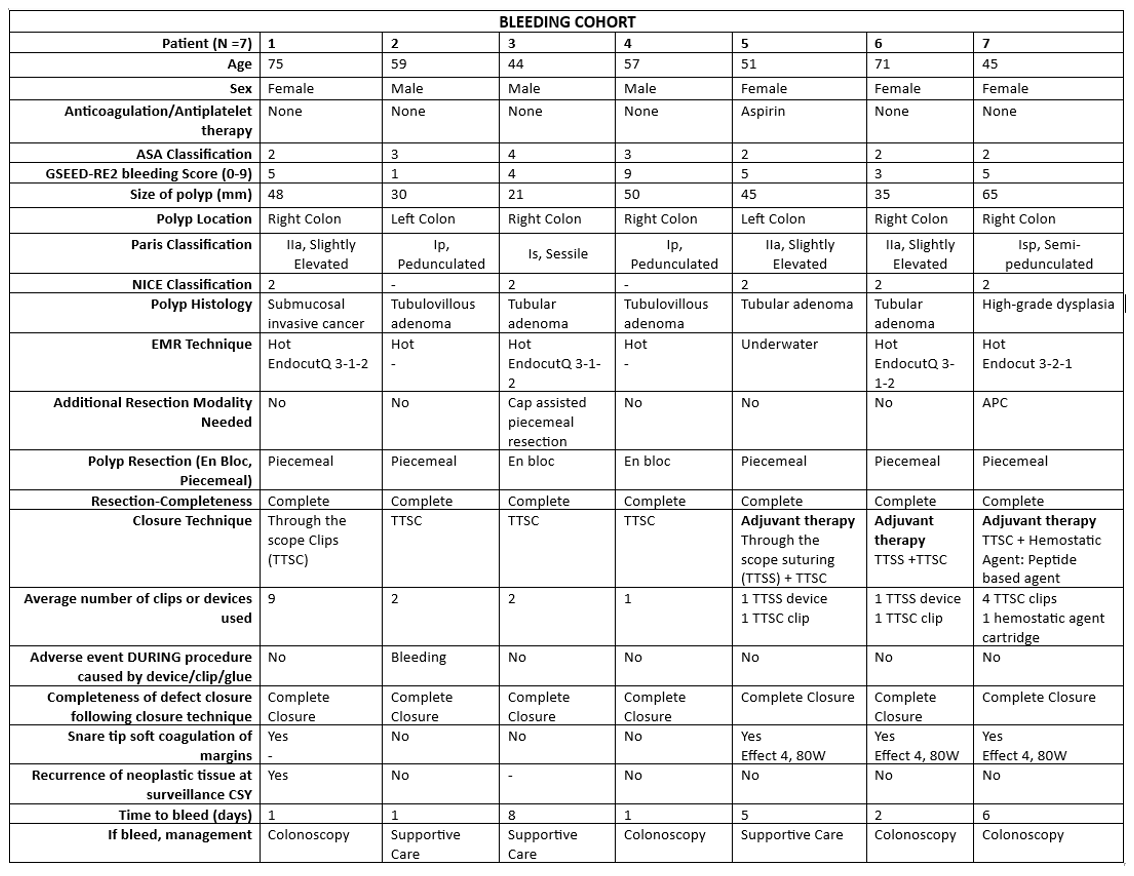
Figure: Table 2 Bleeding Cohort Summary
Disclosures:
Olivia Reszczynski indicated no relevant financial relationships.
Himesh Zaver indicated no relevant financial relationships.
Jason Erno indicated no relevant financial relationships.
Owen Battel indicated no relevant financial relationships.
Aditya Singh indicated no relevant financial relationships.
Gianna Stoleru indicated no relevant financial relationships.
Tanya Wanchek indicated no relevant financial relationships.
Wendy Novicoff indicated no relevant financial relationships.
Ross Buerlein indicated no relevant financial relationships.
Andrew Copland indicated no relevant financial relationships.
Olivia Reszczynski, MD1, Himesh Zaver, MD2, Jason Erno, MD1, Owen Battel, MD1, Aditya Singh, BS2, Gianna Stoleru, MD3, Tanya Wanchek, JD, PhD3, Wendy M. Novicoff, PhD4, Ross Buerlein, MD1, Andrew Copland, MD1. P5138 - Closing In: A Comparative Analysis of the Safety and Effectiveness of Defect Closure Techniques in Colon Polyp Resection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Olivia Reszczynski, MD1, Himesh Zaver, MD2, Jason Erno, MD1, Owen Battel, MD1, Aditya Singh, BS2, Gianna Stoleru, MD3, Tanya Wanchek, JD, PhD3, Wendy M. Novicoff, PhD4, Ross Buerlein, MD1, Andrew Copland, MD1
1University of Virginia Medical Center, Charlottesville, VA; 2University of Virginia Health, Charlottesville, VA; 3University of Virginia, Charlottesville, VA; 4University of Virginia School of Medicine, Charlottesville, VA
Introduction: Endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) are minimally invasive techniques for removing large polyps unsuitable for standard polypectomy. Delayed post-polypectomy bleeding occurs in 4–10% of cases but can be reduced with effective mucosal defect closure. This study aimed to assess the safety and efficacy of various defect closure techniques following large colon polyp resection.
Methods: This retrospective, single-center cohort study examined adult patients who underwent conventional (hot) EMR, underwater EMR, or ESD for colon polyps ≥ 20 mm. Defect closure techniques included through-the-scope clips (TTSC), through-the-scope suturing (TTSS), peptide-based hemostatic agent (HA), or combinations of these techniques.
Results: A total of 241 patients were included in this study (mean age 65.9 years, 48.1% female) (Table 1). Most patients (69.5%) were not on anticoagulation or antiplatelet therapy and the average ASA classification was 2.21 (1–4, SD 0.79). Polyps were mainly located in the right colon (75.8%), with an average polyp size of 33.72 mm (20–70, SD 11.9). Hot EMR was the most common technique (55.1%). Piecemeal resection was performed in 81.1% of cases, with complete polyp resection achieved in 91.0% of cases. Complete defect closure was successful in 97.5% of patients, with similar success rates across cohorts, except for the HA group (89.3%). Adverse events related to defect closure techniques were minimal, with 94.2% of cases (227 patients) experiencing no complications. Intraprocedural bleeding due to defect closure technique occurred in 5.8% of cases (14 patients), and was successfully managed by the end of each respective procedure. No perforations were observed across any technique cohort. The overall incidence of delayed bleeding was 2.9% (7 patients) and similar across cohorts (Table 2). The average time to delayed bleeding was 4.1 days (1–10, SD 3.54), with supportive care (3 cases) and colonoscopy (4 cases) as the primary management strategies.
Discussion: All closure techniques achieved similar complete closure success rates, with no significant difference between single-modality and combination closure techniques in terms of technical success or adverse events. These findings support the continued use of TTSC for defect closure while highlighting the potential for alternative techniques guided by provider expertise and polyp characteristics.
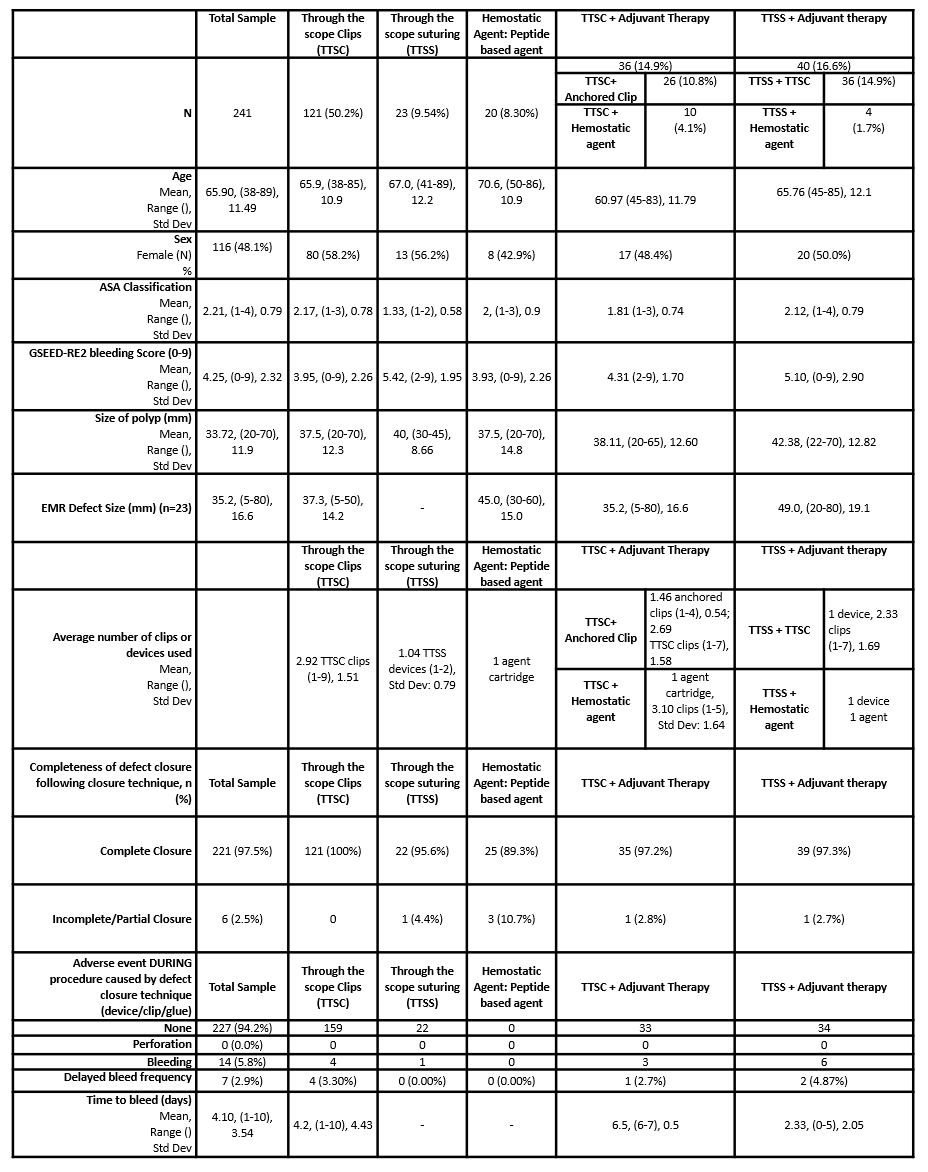
Figure: Table 1 Study Cohort Summary
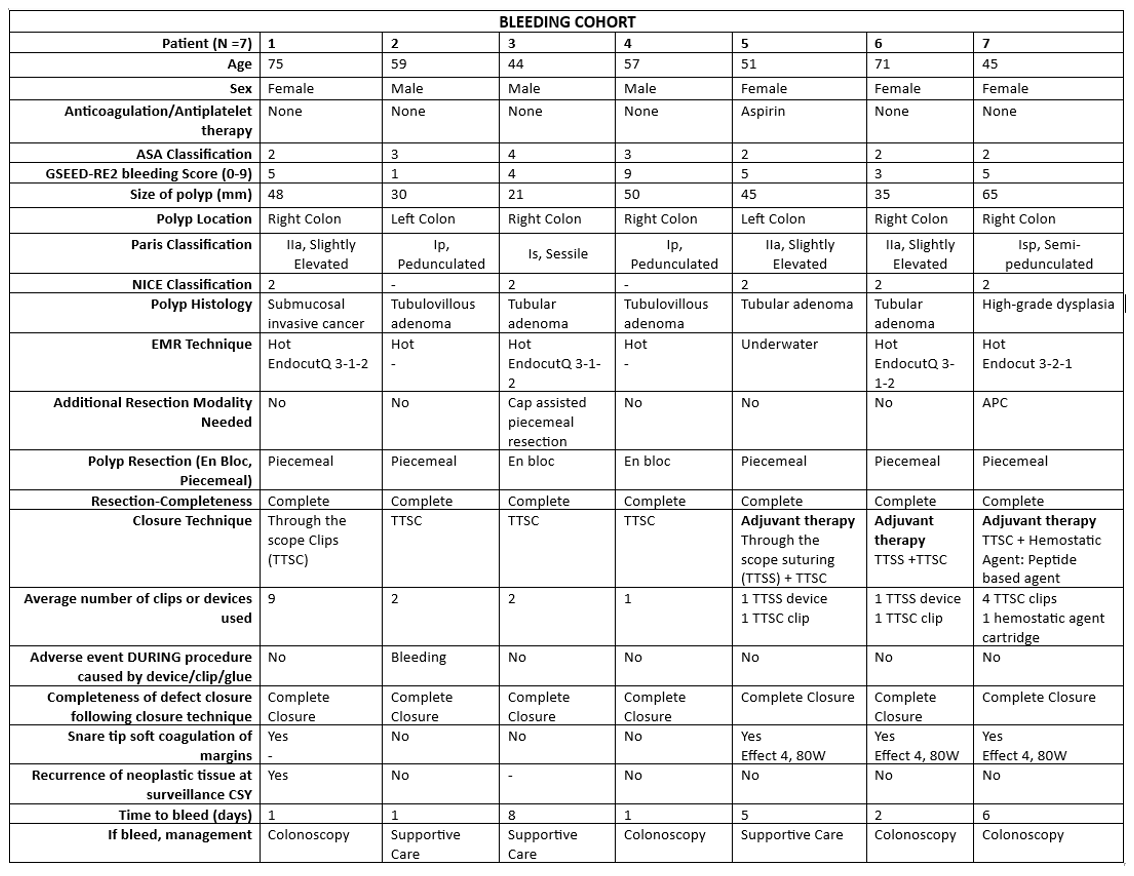
Figure: Table 2 Bleeding Cohort Summary
Disclosures:
Olivia Reszczynski indicated no relevant financial relationships.
Himesh Zaver indicated no relevant financial relationships.
Jason Erno indicated no relevant financial relationships.
Owen Battel indicated no relevant financial relationships.
Aditya Singh indicated no relevant financial relationships.
Gianna Stoleru indicated no relevant financial relationships.
Tanya Wanchek indicated no relevant financial relationships.
Wendy Novicoff indicated no relevant financial relationships.
Ross Buerlein indicated no relevant financial relationships.
Andrew Copland indicated no relevant financial relationships.
Olivia Reszczynski, MD1, Himesh Zaver, MD2, Jason Erno, MD1, Owen Battel, MD1, Aditya Singh, BS2, Gianna Stoleru, MD3, Tanya Wanchek, JD, PhD3, Wendy M. Novicoff, PhD4, Ross Buerlein, MD1, Andrew Copland, MD1. P5138 - Closing In: A Comparative Analysis of the Safety and Effectiveness of Defect Closure Techniques in Colon Polyp Resection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

