Tuesday Poster Session
Category: Functional Bowel Disease
P5105 - May-Thurner Meets the Gut-Brain Axis: Multilevel Dysfunction in Hypermobile Ehler-Danlos Sydnrome
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Chloe K. Tom, MD
Medical University of South Carolina
Mount Pleasant, SC
Presenting Author(s)
Chloe K.. Tom, MD1, Amol Sharma, MD, MSc, FACG2
1Medical University of South Carolina, Mount Pleasant, SC; 2Medical University of South Carolina, Charleston, SC
Introduction: Constipation in hypermobile Ehler-Danlos syndrome (hEDS)/Hypermobility spectrum disorders (HSDs) is multifactorial, stemming from GI dysmotility, autonomic dysfunction, pelvic floor abnormalities, and medication effects. May-Thurner syndrome (MTS), characterized by extrinsic venous compression by the arterial system, most commonly resulting from compression of the left common iliac vein (LCIV) by the right common iliac artery, can lead to pelvic venous hypertension and collateralization. We present a rare case of severe constipation in a patient with hEDS, complicated by MTS and tethered cord syndrome (TCS) – a spinal cord malformation in which pathological attachments limit cord mobility, resulting in neurological dysfunction and exacerbation of bowel dysfunction.
Case Description/
Methods: An 18-year-old female with hEDS, postural orthostatic tachycardia syndrome, mast cell activation syndrome, prior lower extremity DVT on anticoagulation, and PEG tube dependence presented for evaluation of abdominal pain, nausea, vomiting, and failure to thrive (BMI 16). Notably, she reported no bowel movement in six weeks, with a lifelong bowel pattern consistent with one, occasionally bloody, Bristol Stool Scale one bowel movement every two weeks with severe straining. Prior colonoscopy revealed internal hemorrhoids. Cross-sectional imaging was unrevealing, however, venography demonstrated classic MTS with LCIV compression with extensive pelvic and spinal venous collaterals (Fig. 1). She underwent successful iliac vein bypass surgery. Her constipation persisted post-operatively. A medication review revealed chronic use of tramadol and dicyclomine. Her management included counseling to reduce straining, minimizing constipating medications, initiating a secretagogue, instituting elemental nutrition, and anorectal function testing.
Discussion: This case illustrates the diagnostic and therapeutic challenges of severe constipation in patients with hEDS. Long-standing bowel dysfunction may be a consequence and contributor to multi-system pathology through mechanisms like low-grade inflammation, intestinal hyperpermeability, and autonomic dysregulation. Pelvic venous outflow obstruction (e.g. MTS) and neurological impairments (e.g. TCS) may coexist and potentiate gut dysfunction, particularly in connective tissue disorders. A high index of suspicion and a multidisciplinary approach are essential for identifying and managing overlapping anatomic and functional contributors to intractable constipation in hEDS.
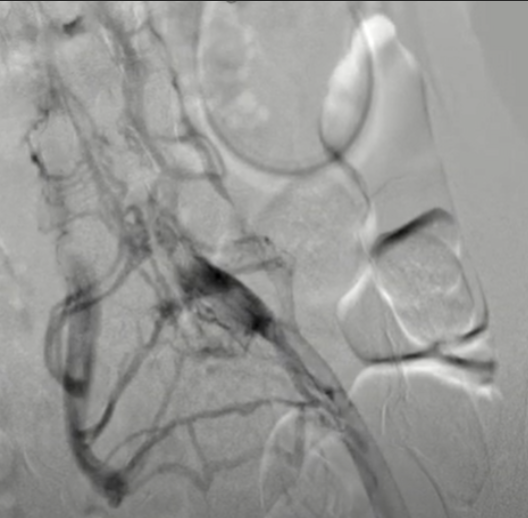
Figure: The right common iliac artery compresses the left common iliac vein against the vertebra with venous collaterals into the spinal veins.
Disclosures:
Chloe Tom indicated no relevant financial relationships.
Amol Sharma indicated no relevant financial relationships.
Chloe K.. Tom, MD1, Amol Sharma, MD, MSc, FACG2. P5105 - May-Thurner Meets the Gut-Brain Axis: Multilevel Dysfunction in Hypermobile Ehler-Danlos Sydnrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Medical University of South Carolina, Mount Pleasant, SC; 2Medical University of South Carolina, Charleston, SC
Introduction: Constipation in hypermobile Ehler-Danlos syndrome (hEDS)/Hypermobility spectrum disorders (HSDs) is multifactorial, stemming from GI dysmotility, autonomic dysfunction, pelvic floor abnormalities, and medication effects. May-Thurner syndrome (MTS), characterized by extrinsic venous compression by the arterial system, most commonly resulting from compression of the left common iliac vein (LCIV) by the right common iliac artery, can lead to pelvic venous hypertension and collateralization. We present a rare case of severe constipation in a patient with hEDS, complicated by MTS and tethered cord syndrome (TCS) – a spinal cord malformation in which pathological attachments limit cord mobility, resulting in neurological dysfunction and exacerbation of bowel dysfunction.
Case Description/
Methods: An 18-year-old female with hEDS, postural orthostatic tachycardia syndrome, mast cell activation syndrome, prior lower extremity DVT on anticoagulation, and PEG tube dependence presented for evaluation of abdominal pain, nausea, vomiting, and failure to thrive (BMI 16). Notably, she reported no bowel movement in six weeks, with a lifelong bowel pattern consistent with one, occasionally bloody, Bristol Stool Scale one bowel movement every two weeks with severe straining. Prior colonoscopy revealed internal hemorrhoids. Cross-sectional imaging was unrevealing, however, venography demonstrated classic MTS with LCIV compression with extensive pelvic and spinal venous collaterals (Fig. 1). She underwent successful iliac vein bypass surgery. Her constipation persisted post-operatively. A medication review revealed chronic use of tramadol and dicyclomine. Her management included counseling to reduce straining, minimizing constipating medications, initiating a secretagogue, instituting elemental nutrition, and anorectal function testing.
Discussion: This case illustrates the diagnostic and therapeutic challenges of severe constipation in patients with hEDS. Long-standing bowel dysfunction may be a consequence and contributor to multi-system pathology through mechanisms like low-grade inflammation, intestinal hyperpermeability, and autonomic dysregulation. Pelvic venous outflow obstruction (e.g. MTS) and neurological impairments (e.g. TCS) may coexist and potentiate gut dysfunction, particularly in connective tissue disorders. A high index of suspicion and a multidisciplinary approach are essential for identifying and managing overlapping anatomic and functional contributors to intractable constipation in hEDS.
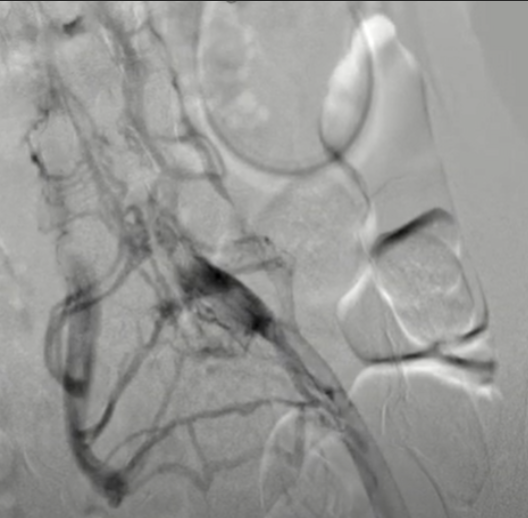
Figure: The right common iliac artery compresses the left common iliac vein against the vertebra with venous collaterals into the spinal veins.
Disclosures:
Chloe Tom indicated no relevant financial relationships.
Amol Sharma indicated no relevant financial relationships.
Chloe K.. Tom, MD1, Amol Sharma, MD, MSc, FACG2. P5105 - May-Thurner Meets the Gut-Brain Axis: Multilevel Dysfunction in Hypermobile Ehler-Danlos Sydnrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
