Tuesday Poster Session
Category: Functional Bowel Disease
P5099 - Digitally Delivered Diaphragmatic Breathing Improves Core IBS Symptoms: A Multivariable Regression Analysis of Over 38,000 Users
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Mauricio F. Jin, MD
Mayo Clinic
Rochester, MN
Presenting Author(s)
Mauricio F. Jin, MD1, Xiao Jing Wang, MD1, Claire Hall, 2
1Mayo Clinic, Rochester, MN; 2Mindset Health, Boston, MA
Introduction: Diaphragmatic breathing (DB), a gut-directed behavioral therapy, may help modulate gut-brain axis activity in patients with irritable bowel syndrome (IBS) for whom limited options for symptom relief are available. While often combined with other interventions, data on its independent effect is lacking. The present study evaluates the impact of DB exercises delivered via a digital program, Nerva, on symptom improvement in abdominal bloating, abdominal pain, and passage of wind over a 6-week period.
Methods: Data were retrospectively analyzed from Nerva users, providing IBS symptom tracking and digital diaphragmatic breathing intervention. Symptom severity was measured using IBS-visual analog scale (IBS-VAS) at baseline and at week 6. Changes in score from baseline to week 6 were modeled using multivariable linear regression models, adjusted for baseline symptom severity, age, sex, IBS classification, and supplemental intervention use (including hypnotherapy, supplements). To minimize long-tail influence, breathing session count was capped at 40, capturing >95% of users. Outliers and influential observations were excluded using standardized residuals and Cook’s distance.
Results: Data were retrospectively analyzed from 38,454 Nerva users. Patient demographics are included on table 1. Final models for abdominal bloating, abdominal pain, and passage of wind included 18,242, 13,330, and 17,846 participants respectively. Breathing sessions were completed by a subset of users (table 2). Across all models, higher engagement with DB was significantly associated with greater symptom improvement. Within our truncated range of up to 40 sessions, linear regression demonstrated modest but statistically significant associations between number of diaphragmatic breathing sessions and symptom improvement across all three core symptom domains. Each additional breathing exercise was associated with a 0.27 improvement in bloating score (β = -0.27, 95% CI: -0.32 to -0.21, p < 0.001), a 0.27 reduction in abdominal pain, (β = -0.27, 95% CI: -0.32 to -0.22, p < 0.001), and a 0.25 reduction in passage of wind (β = -0.25, 95% CI: -0.30 to -0.20, p < 0.001).
Discussion: In our real-world IBS cohort, diaphragmatic breathing was independently associated with modest, yet consistent symptom improvements across abdominal bloating, pain, and gas-related discomfort. These findings support the role of diaphragmatic breathing as an accessible and effective part of treatment for self-guided IBS management.
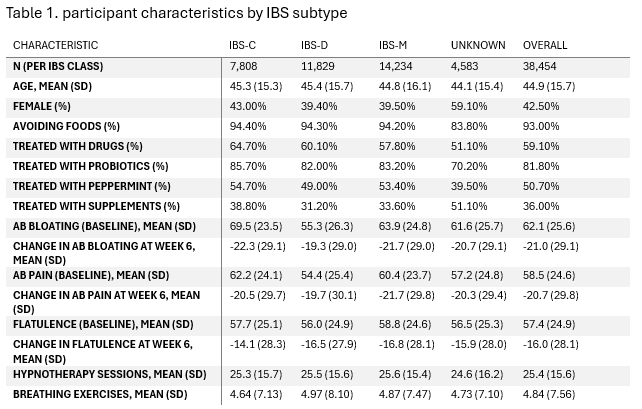
Figure: Table 1. Patient demographics
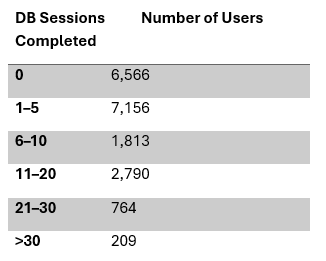
Figure: Table 2. Distribution of users by number of diaphragmatic breathing sessions completed
Disclosures:
Mauricio Jin indicated no relevant financial relationships.
Xiao Jing Wang indicated no relevant financial relationships.
Claire Hall: Mindset Health – Employee.
Mauricio F. Jin, MD1, Xiao Jing Wang, MD1, Claire Hall, 2. P5099 - Digitally Delivered Diaphragmatic Breathing Improves Core IBS Symptoms: A Multivariable Regression Analysis of Over 38,000 Users, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mayo Clinic, Rochester, MN; 2Mindset Health, Boston, MA
Introduction: Diaphragmatic breathing (DB), a gut-directed behavioral therapy, may help modulate gut-brain axis activity in patients with irritable bowel syndrome (IBS) for whom limited options for symptom relief are available. While often combined with other interventions, data on its independent effect is lacking. The present study evaluates the impact of DB exercises delivered via a digital program, Nerva, on symptom improvement in abdominal bloating, abdominal pain, and passage of wind over a 6-week period.
Methods: Data were retrospectively analyzed from Nerva users, providing IBS symptom tracking and digital diaphragmatic breathing intervention. Symptom severity was measured using IBS-visual analog scale (IBS-VAS) at baseline and at week 6. Changes in score from baseline to week 6 were modeled using multivariable linear regression models, adjusted for baseline symptom severity, age, sex, IBS classification, and supplemental intervention use (including hypnotherapy, supplements). To minimize long-tail influence, breathing session count was capped at 40, capturing >95% of users. Outliers and influential observations were excluded using standardized residuals and Cook’s distance.
Results: Data were retrospectively analyzed from 38,454 Nerva users. Patient demographics are included on table 1. Final models for abdominal bloating, abdominal pain, and passage of wind included 18,242, 13,330, and 17,846 participants respectively. Breathing sessions were completed by a subset of users (table 2). Across all models, higher engagement with DB was significantly associated with greater symptom improvement. Within our truncated range of up to 40 sessions, linear regression demonstrated modest but statistically significant associations between number of diaphragmatic breathing sessions and symptom improvement across all three core symptom domains. Each additional breathing exercise was associated with a 0.27 improvement in bloating score (β = -0.27, 95% CI: -0.32 to -0.21, p < 0.001), a 0.27 reduction in abdominal pain, (β = -0.27, 95% CI: -0.32 to -0.22, p < 0.001), and a 0.25 reduction in passage of wind (β = -0.25, 95% CI: -0.30 to -0.20, p < 0.001).
Discussion: In our real-world IBS cohort, diaphragmatic breathing was independently associated with modest, yet consistent symptom improvements across abdominal bloating, pain, and gas-related discomfort. These findings support the role of diaphragmatic breathing as an accessible and effective part of treatment for self-guided IBS management.
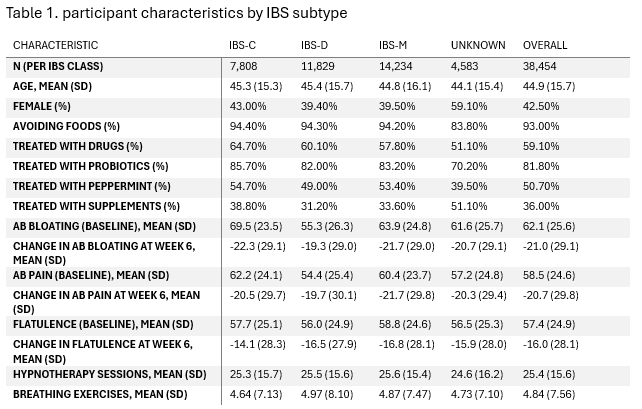
Figure: Table 1. Patient demographics
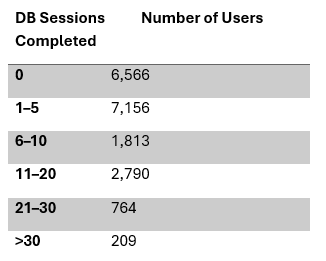
Figure: Table 2. Distribution of users by number of diaphragmatic breathing sessions completed
Disclosures:
Mauricio Jin indicated no relevant financial relationships.
Xiao Jing Wang indicated no relevant financial relationships.
Claire Hall: Mindset Health – Employee.
Mauricio F. Jin, MD1, Xiao Jing Wang, MD1, Claire Hall, 2. P5099 - Digitally Delivered Diaphragmatic Breathing Improves Core IBS Symptoms: A Multivariable Regression Analysis of Over 38,000 Users, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

