Tuesday Poster Session
Category: Functional Bowel Disease
P5073 - Motility Matters: Is Dyssynergia in Cancer Patients Being Ignored?
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Pooja Prasad, MD
Baylor College of Medicine
Houston, TX
Presenting Author(s)
Award: ACG Presidential Poster Award
Pooja Prasad, MD1, Lavanya Viswanathan, MD, MS, FACG2
1Baylor College of Medicine, Houston, TX; 2UT MD Anderson Cancer Center, Houston, TX
Introduction: Anorectal manometry (ARM) in cancer patients has focused on those with rectal and prostate cancer after low anterior resection or chemoradiation. No studies have compared motility findings between pelvic and non-pelvic cancers. We retrospectively analyzed cancer patients referred for ARM, hypothesizing that pelvic cancers and treatments would correlate with higher rates of dyssynergia and rectal hypersensitivity.
Methods: We analyzed adult patients referred for ARM for bowel complaints at UT MD Anderson Cancer Center (2019-2024), stratified by age, sex, cancer type, treatment history, and ARM findings. Multivariable logistic regression assessed associations between cancer type and ARM findings, using non-pelvic cancers as the reference. Models adjusted for age, sex, and treatment. Odds ratios (ORs) and 95% confidence intervals (CIs) were reported (p< 0.05 is significant).
Results: Among 115 patients (77% female, mean age 63), cancers included breast (25%), GI (23%), hematologic (16%), prostate (11%), and GU (10%). 65% were referred for ARM due to constipation and 35% for fecal incontinence, as defined by ICD diagnosis. Mean time from cancer diagnosis to ARM was 7.2 years. Dyssynergia was present in 41%, predominantly type 1 (Table 1). As hypothesized, compared to non-pelvic floor cancers, rectal and prostate cancers showed higher odds of dyssynergia, with rectal cancer approaching statistical significance (OR 6.93, [0.88, 7.97] p= 0.098). GU and rectal cancers also showed increased odds of rectal hypersensitivity, though not statistically significant. No significant associations were found with age, sex, or treatment history (i.e. surgery, radiation, chemotherapy).
Discussion: Rectal and prostate cancers were associated with higher dyssynergia rates, regardless of treatment. Type 1 dyssynergia was the most common subtype, and women had higher rates in cancers affecting both sexes – consistent with literature. Overall, the study is limited by sample size, with only 115 patients referred for lower motility testing over 5 years. This reflects the broader underuse of motility testing in cancer patients and need for increased screening and awareness by patients’ primary team. The 7.2-year average delay from cancer diagnosis to ARM highlights the barriers to motility evaluation even at a tertiary care center. This novel study reveals a care gap in addressing motility issues among cancer patients and underscores the need for to screen for GI symptoms, particularly in those with pelvic cancers.
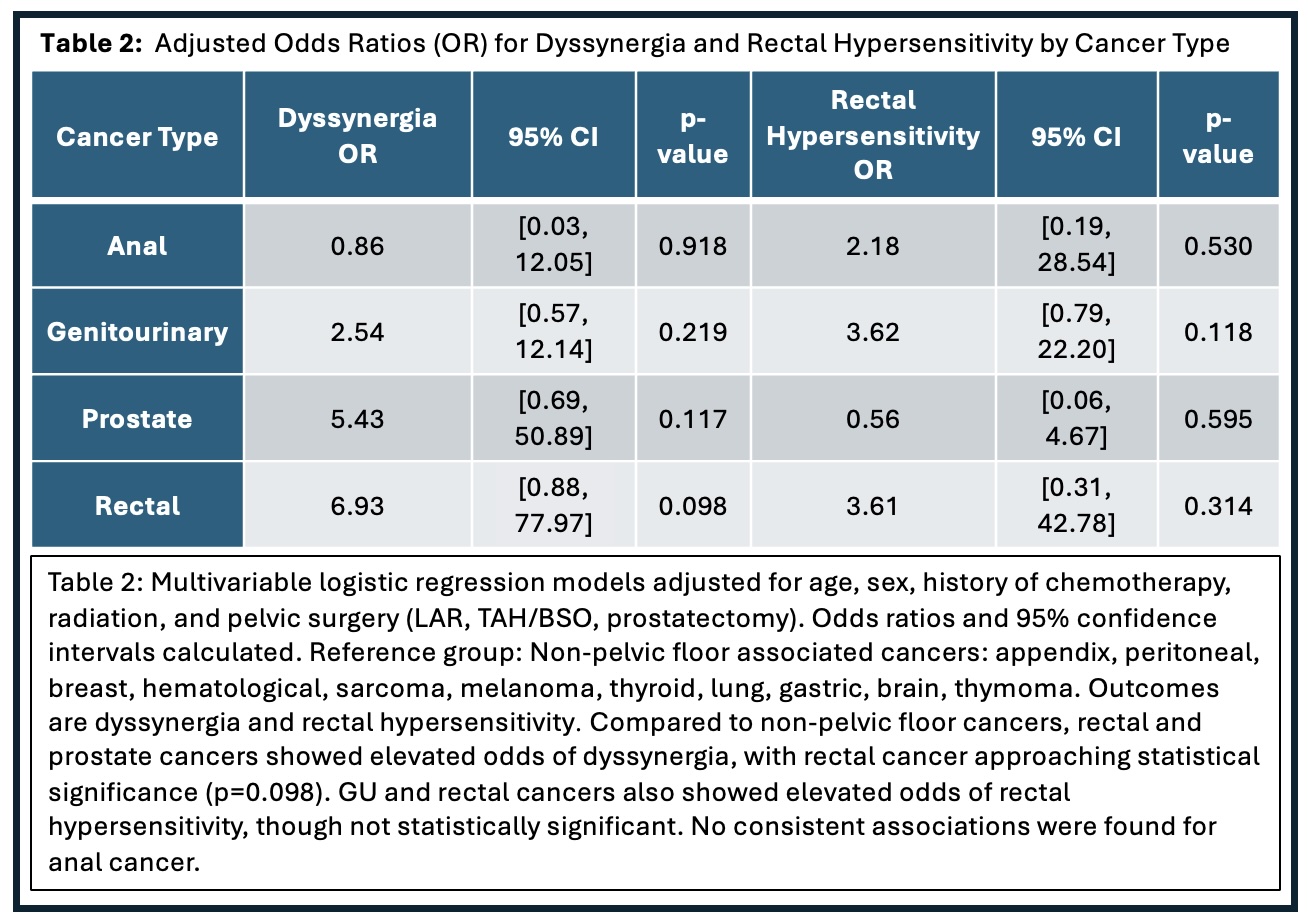
Figure: Table 1
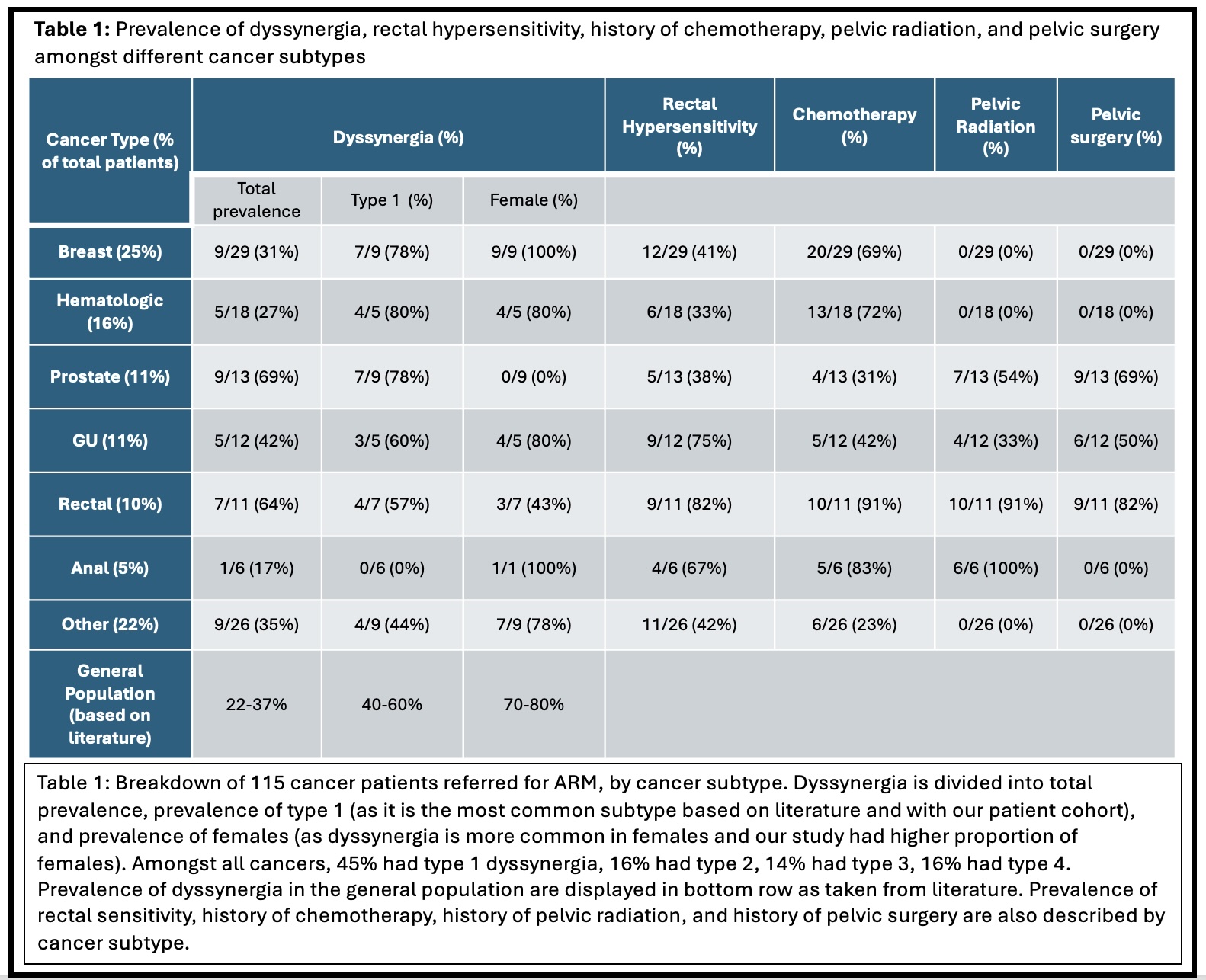
Figure: Table 2
Disclosures:
Pooja Prasad indicated no relevant financial relationships.
Lavanya Viswanathan: Ardelyx, Inc. – Advisor or Review Panel Member, The above are unpaid., Speakers Bureau.
Pooja Prasad, MD1, Lavanya Viswanathan, MD, MS, FACG2. P5073 - Motility Matters: Is Dyssynergia in Cancer Patients Being Ignored?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Pooja Prasad, MD1, Lavanya Viswanathan, MD, MS, FACG2
1Baylor College of Medicine, Houston, TX; 2UT MD Anderson Cancer Center, Houston, TX
Introduction: Anorectal manometry (ARM) in cancer patients has focused on those with rectal and prostate cancer after low anterior resection or chemoradiation. No studies have compared motility findings between pelvic and non-pelvic cancers. We retrospectively analyzed cancer patients referred for ARM, hypothesizing that pelvic cancers and treatments would correlate with higher rates of dyssynergia and rectal hypersensitivity.
Methods: We analyzed adult patients referred for ARM for bowel complaints at UT MD Anderson Cancer Center (2019-2024), stratified by age, sex, cancer type, treatment history, and ARM findings. Multivariable logistic regression assessed associations between cancer type and ARM findings, using non-pelvic cancers as the reference. Models adjusted for age, sex, and treatment. Odds ratios (ORs) and 95% confidence intervals (CIs) were reported (p< 0.05 is significant).
Results: Among 115 patients (77% female, mean age 63), cancers included breast (25%), GI (23%), hematologic (16%), prostate (11%), and GU (10%). 65% were referred for ARM due to constipation and 35% for fecal incontinence, as defined by ICD diagnosis. Mean time from cancer diagnosis to ARM was 7.2 years. Dyssynergia was present in 41%, predominantly type 1 (Table 1). As hypothesized, compared to non-pelvic floor cancers, rectal and prostate cancers showed higher odds of dyssynergia, with rectal cancer approaching statistical significance (OR 6.93, [0.88, 7.97] p= 0.098). GU and rectal cancers also showed increased odds of rectal hypersensitivity, though not statistically significant. No significant associations were found with age, sex, or treatment history (i.e. surgery, radiation, chemotherapy).
Discussion: Rectal and prostate cancers were associated with higher dyssynergia rates, regardless of treatment. Type 1 dyssynergia was the most common subtype, and women had higher rates in cancers affecting both sexes – consistent with literature. Overall, the study is limited by sample size, with only 115 patients referred for lower motility testing over 5 years. This reflects the broader underuse of motility testing in cancer patients and need for increased screening and awareness by patients’ primary team. The 7.2-year average delay from cancer diagnosis to ARM highlights the barriers to motility evaluation even at a tertiary care center. This novel study reveals a care gap in addressing motility issues among cancer patients and underscores the need for to screen for GI symptoms, particularly in those with pelvic cancers.
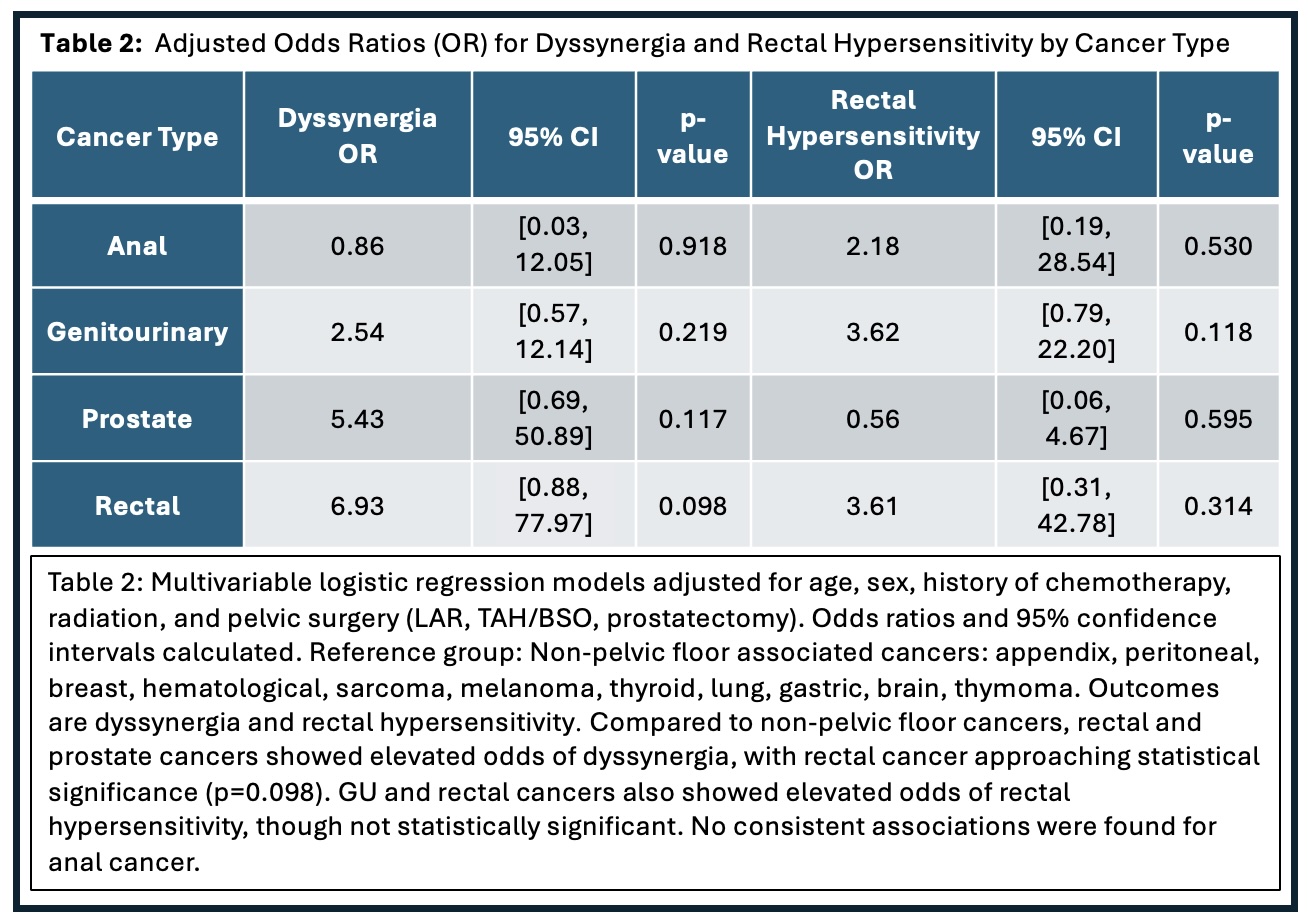
Figure: Table 1
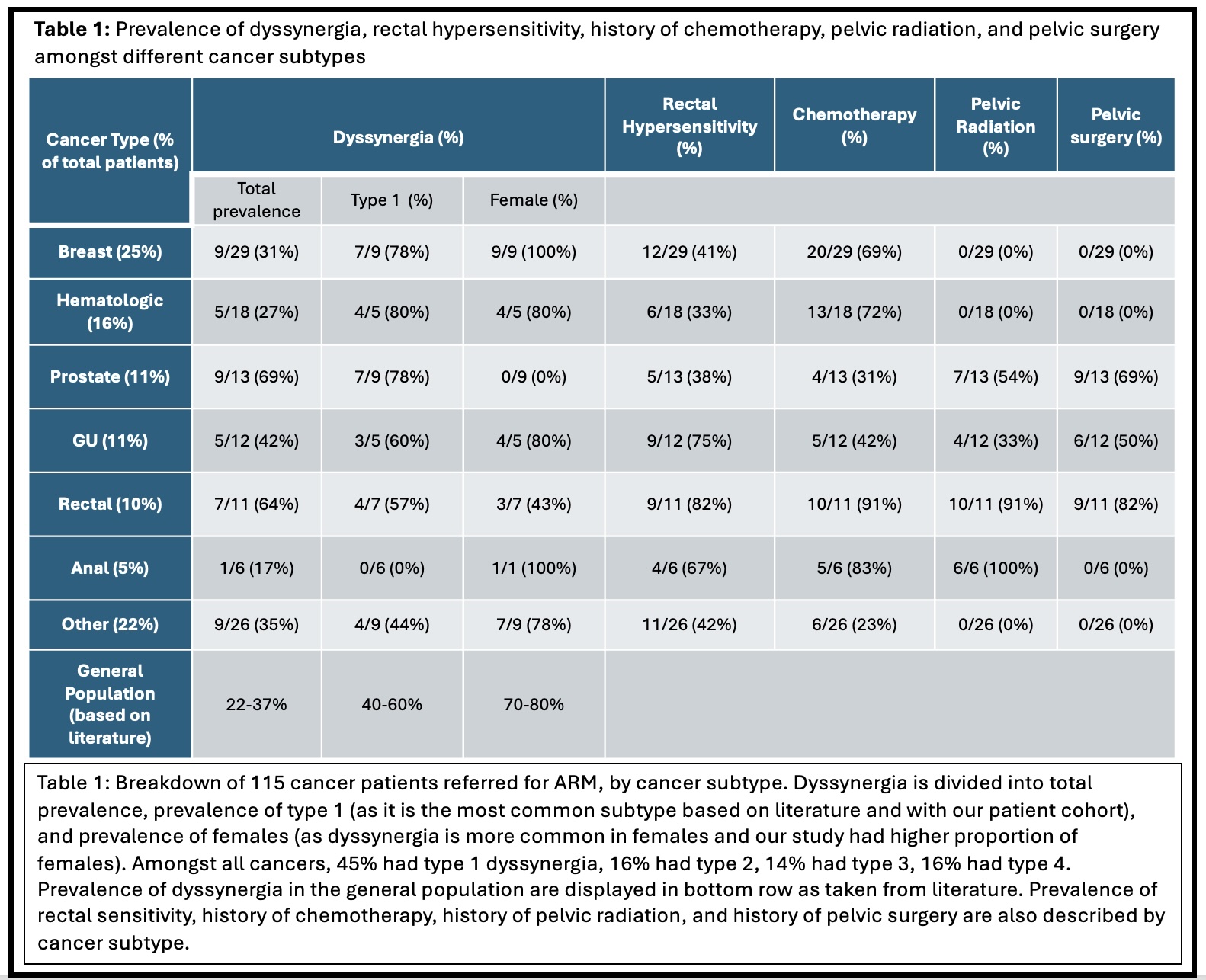
Figure: Table 2
Disclosures:
Pooja Prasad indicated no relevant financial relationships.
Lavanya Viswanathan: Ardelyx, Inc. – Advisor or Review Panel Member, The above are unpaid., Speakers Bureau.
Pooja Prasad, MD1, Lavanya Viswanathan, MD, MS, FACG2. P5073 - Motility Matters: Is Dyssynergia in Cancer Patients Being Ignored?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

