Tuesday Poster Session
Category: Esophagus
P5056 - Atypical Presentation of Killian-Jamieson Diverticulum: A Case Report
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Kelly M. Vo, DO (she/her/hers)
Walter Reed National Military Medical Center
Bethesda, MD
Presenting Author(s)
Kelly M. Vo, DO, Andrew Kim, MD, John McCarthy, MD
Walter Reed National Military Medical Center, Bethesda, MD
Introduction: Esophageal diverticula are rare, affecting 0.06%–4% of the population. Usually identified in the elderly, symptoms include dysphagia, regurgitation, halitosis, cough, and chest pain. Zenker’s diverticulum (ZD) is the most common esophageal diverticulum (0.01%–0.11%) and typically occurs in men, arising from the midline posterior pharyngoesophageal segment. Killian-Jamieson diverticulum (KJD), found more commonly in women in about 0.025% of people, originates from the anterolateral proximal cervical esophagus. We present a case of a man with KJD, highlighting its uncommon features and management challenges.
Case Description/
Methods: A 53-year-old man never-smoker with a medical history of obstructive sleep apnea, prediabetes, and environmental allergies, presented with chronic solid-food dysphagia associated with weekly coughing and halitosis. He denied red-flag symptoms such as unintentional weight loss or a family history of esophageal cancer. Baseline laboratory tests were reassuring, including no evidence of anemia. Physical examination was unremarkable. Esophagogastroduodenoscopy was aborted upon encountering food debris within the inlet to the esophagus (Figure 1). Due to an iodine allergy, a non-contrast computed tomography scan was performed, revealing a 3.6 x 3.5 x 4.9 cm left lateral esophageal outpouching at the T2 level (Figure 2A–C). A barium esophagogram confirmed a large left anterolateral diverticulum consistent with Killian-Jamieson diverticulum (Figure 2D). Nasolaryngoscopy by Otolaryngology was unable to visualize diverticulum due to the atypical and more distal location.
Discussion: KJD and ZD differ in location and demographics, with the former often smaller and asymptomatic. Diagnosis is usually confirmed by esophagogram or upper endoscopy. Treatment is indicated for symptomatic diverticula and may involve surgical or endoscopic intervention. KJD is thought to originate from functional outflow obstruction. About 50% of KJD cases ultimately require surgical intervention. However, endoscopic approaches carry a risk of recurrence and potential injury to the recurrent laryngeal nerve. In this case, given the diverticulum’s uncommon location and complexity, and after multidisciplinary consultation and shared decision-making, the patient opted for continued observation rather than surgical or endoscopic intervention. This case highlights the importance of a multidisciplinary approach in managing complex and rare esophageal conditions.
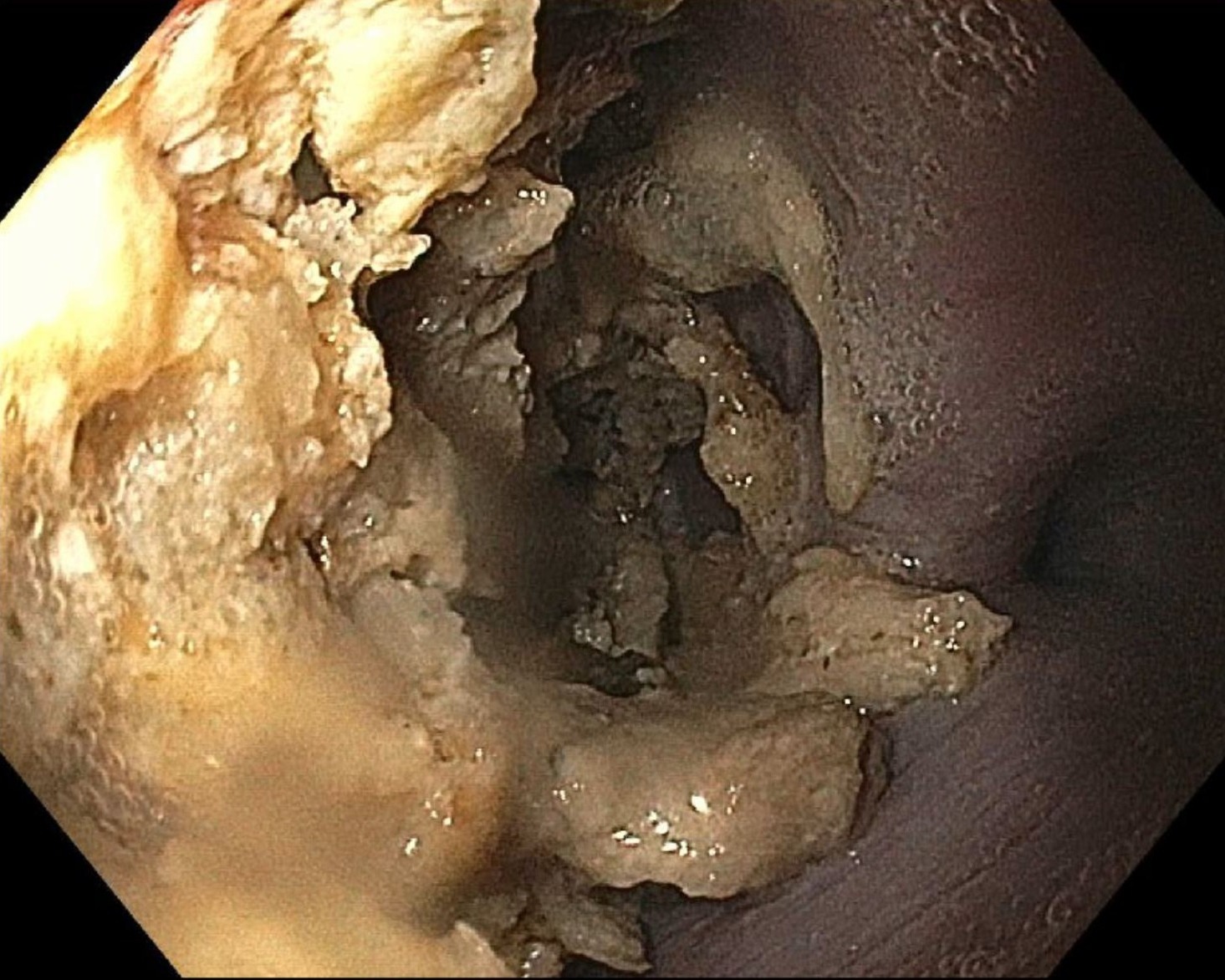
Figure: Figure 1. Endoscopy image. Esophagogastroduodenoscopy showing food debris immediately within the esophageal inlet.
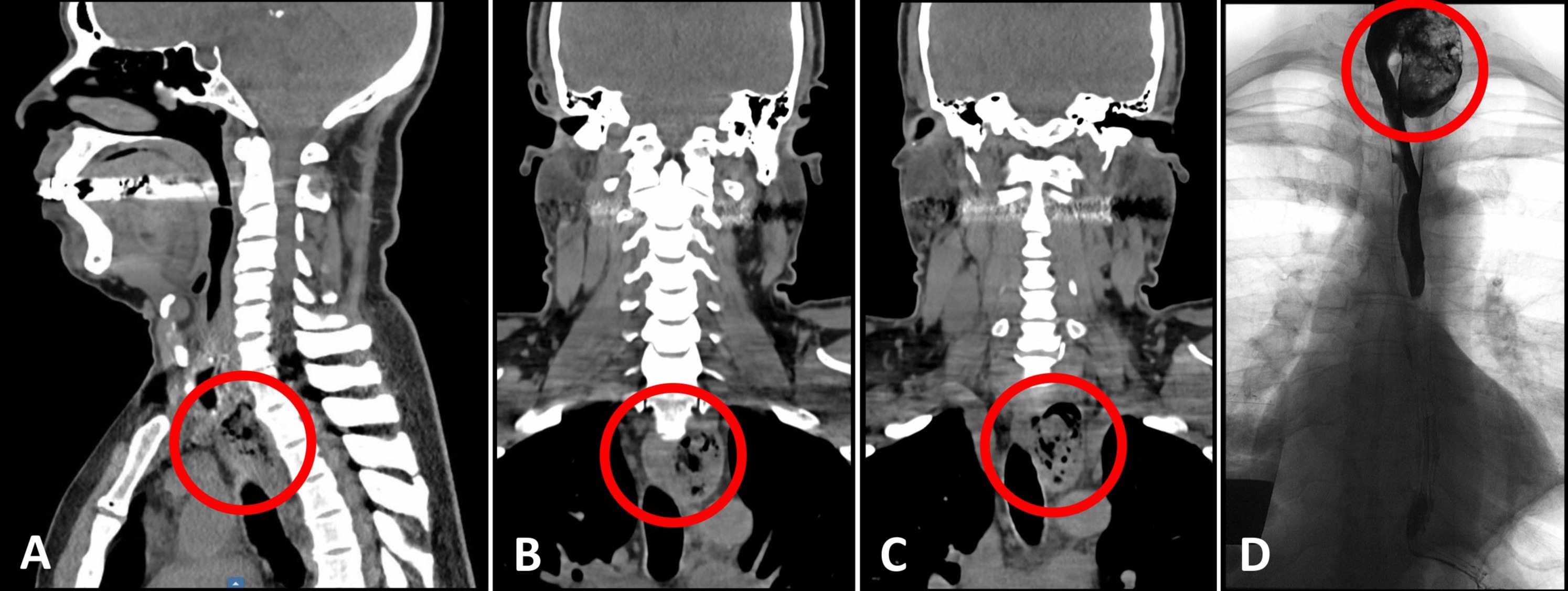
Figure: Figure 2: Radiological images. A-C) Non-contrast computed tomography scan showing a 3.6 x 3.5 x 4.9 cm left lateral esophageal outpouching at the T2 level. D) Barium esophagogram showing a large left anterolateral diverticulum consistent with Killian-Jamieson diverticulum.
Disclosures:
Kelly Vo indicated no relevant financial relationships.
Andrew Kim indicated no relevant financial relationships.
John McCarthy indicated no relevant financial relationships.
Kelly M. Vo, DO, Andrew Kim, MD, John McCarthy, MD. P5056 - Atypical Presentation of Killian-Jamieson Diverticulum: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Walter Reed National Military Medical Center, Bethesda, MD
Introduction: Esophageal diverticula are rare, affecting 0.06%–4% of the population. Usually identified in the elderly, symptoms include dysphagia, regurgitation, halitosis, cough, and chest pain. Zenker’s diverticulum (ZD) is the most common esophageal diverticulum (0.01%–0.11%) and typically occurs in men, arising from the midline posterior pharyngoesophageal segment. Killian-Jamieson diverticulum (KJD), found more commonly in women in about 0.025% of people, originates from the anterolateral proximal cervical esophagus. We present a case of a man with KJD, highlighting its uncommon features and management challenges.
Case Description/
Methods: A 53-year-old man never-smoker with a medical history of obstructive sleep apnea, prediabetes, and environmental allergies, presented with chronic solid-food dysphagia associated with weekly coughing and halitosis. He denied red-flag symptoms such as unintentional weight loss or a family history of esophageal cancer. Baseline laboratory tests were reassuring, including no evidence of anemia. Physical examination was unremarkable. Esophagogastroduodenoscopy was aborted upon encountering food debris within the inlet to the esophagus (Figure 1). Due to an iodine allergy, a non-contrast computed tomography scan was performed, revealing a 3.6 x 3.5 x 4.9 cm left lateral esophageal outpouching at the T2 level (Figure 2A–C). A barium esophagogram confirmed a large left anterolateral diverticulum consistent with Killian-Jamieson diverticulum (Figure 2D). Nasolaryngoscopy by Otolaryngology was unable to visualize diverticulum due to the atypical and more distal location.
Discussion: KJD and ZD differ in location and demographics, with the former often smaller and asymptomatic. Diagnosis is usually confirmed by esophagogram or upper endoscopy. Treatment is indicated for symptomatic diverticula and may involve surgical or endoscopic intervention. KJD is thought to originate from functional outflow obstruction. About 50% of KJD cases ultimately require surgical intervention. However, endoscopic approaches carry a risk of recurrence and potential injury to the recurrent laryngeal nerve. In this case, given the diverticulum’s uncommon location and complexity, and after multidisciplinary consultation and shared decision-making, the patient opted for continued observation rather than surgical or endoscopic intervention. This case highlights the importance of a multidisciplinary approach in managing complex and rare esophageal conditions.
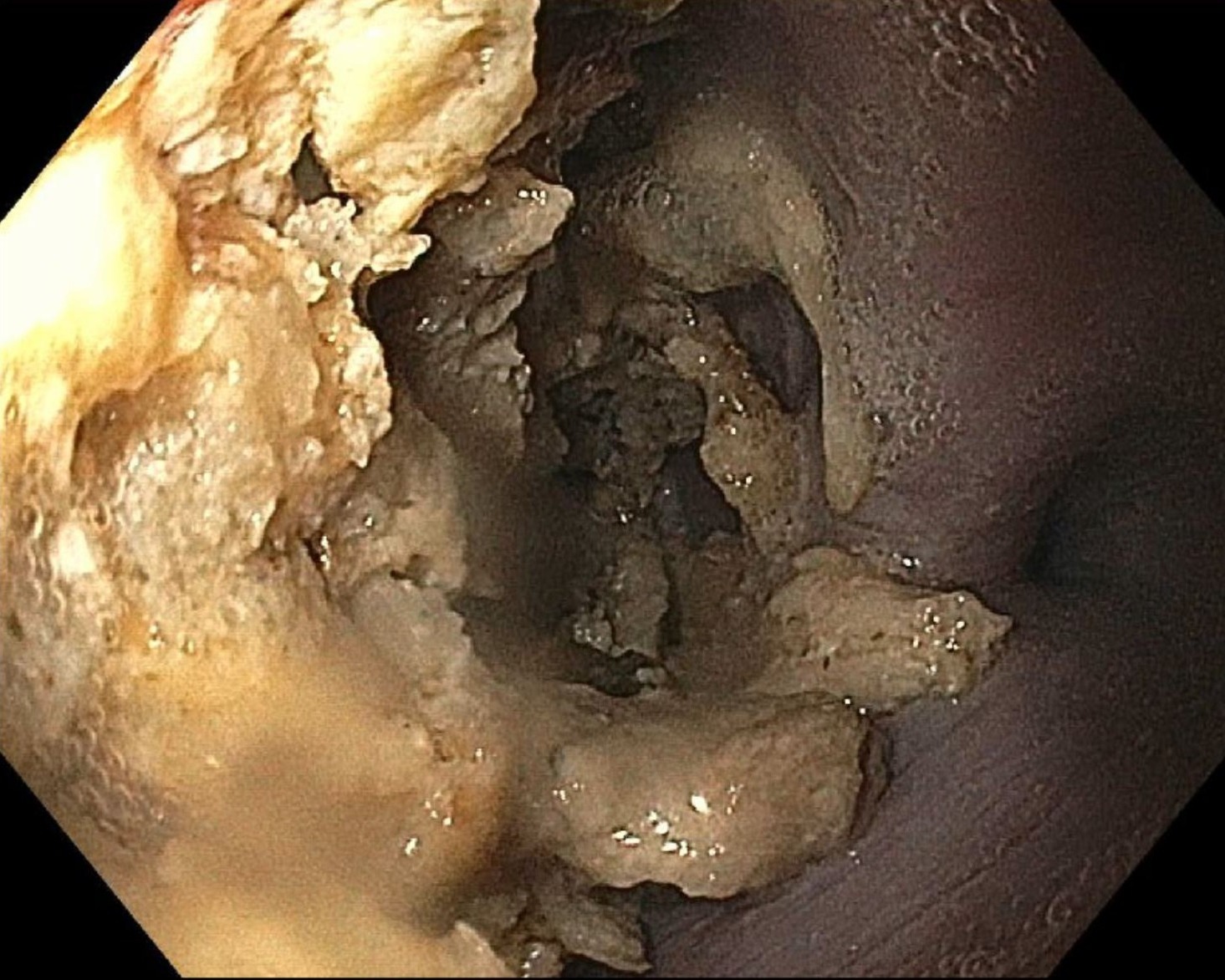
Figure: Figure 1. Endoscopy image. Esophagogastroduodenoscopy showing food debris immediately within the esophageal inlet.
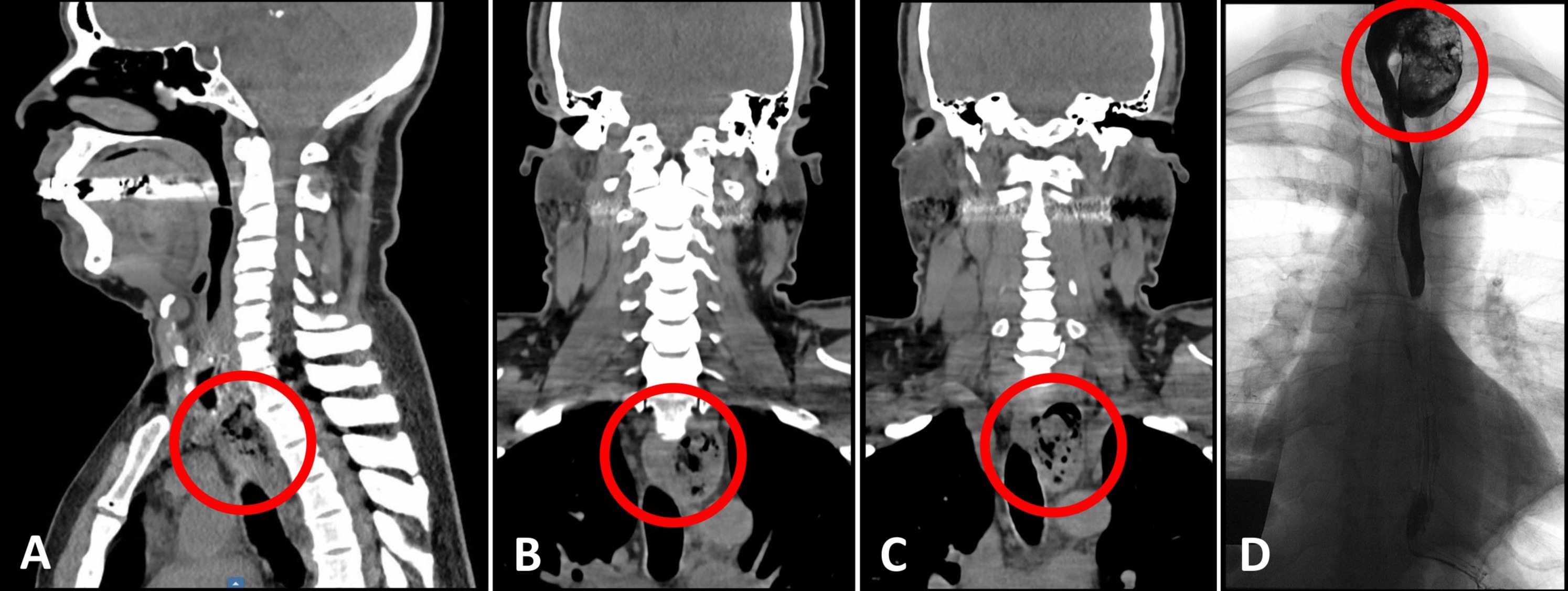
Figure: Figure 2: Radiological images. A-C) Non-contrast computed tomography scan showing a 3.6 x 3.5 x 4.9 cm left lateral esophageal outpouching at the T2 level. D) Barium esophagogram showing a large left anterolateral diverticulum consistent with Killian-Jamieson diverticulum.
Disclosures:
Kelly Vo indicated no relevant financial relationships.
Andrew Kim indicated no relevant financial relationships.
John McCarthy indicated no relevant financial relationships.
Kelly M. Vo, DO, Andrew Kim, MD, John McCarthy, MD. P5056 - Atypical Presentation of Killian-Jamieson Diverticulum: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
