Tuesday Poster Session
Category: Esophagus
P5053 - From Varices to Viral Infiltrate: Diagnosing CMV Gastritis in a Cirrhotic, Immunocompromised Host
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mina Awadallah, MD, MSc
University of Utah
Salt Lake City, UT
Presenting Author(s)
Mina Awadallah, MD, MSc1, Viveksandeep Thoguluva Chandrasekar, MBBS2, Jolanta Jedrzkiewicz, MD1, Rebecca G. Kim, MD, MAS3, John Erikson Yap, MD, MBA, FACG3
1University of Utah, Salt Lake City, UT; 2Medical College of Georgia at Augusta University, Augusta, GA; 3University of Utah Health, Salt Lake City, UT
Introduction: Cytomegalovirus (CMV) gastritis is a rare but important cause of upper gastrointestinal pathology, most often identified in immunocompromised individuals. In patients with cirrhosis and overlapping immunosuppressive conditions, CMV involvement of the upper GI tract may be overlooked, as symptoms are frequently attributed to portal gastropathy. We present a case of biopsy-proven CMV gastritis in a patient with metabolic-associated steatohepatitis (MASH) cirrhosis and chronic B-cell depletion from long-term rituximab therapy.
Case Description/
Methods: A 68-year-old woman with compensated MASH cirrhosis, morbid obesity, rheumatoid arthritis (on rituximab for 9 years), interstitial lung disease (on fluticasone furoate/umeclidinium/vilanterol), atrial fibrillation on anticoagulation, prediabetes, hypothyroidism, and depression underwent upper endoscopy for variceal screening. She was found to have large esophageal varices, which were successfully banded. In addition, mucosal erythema was noted in the gastric body. The appearance was not consistent with typical portal hypertensive gastropathy, prompting biopsy for further evaluation.
Gastric biopsies demonstrated mildly active chronic gastritis with viral cytopathic changes consistent with CMV, confirmed by positive immunohistochemical staining. H. pylori was negative. The inflammatory infiltrate included eosinophils and CD68-positive histiocytes. Special stains for fungi, acid-fast bacilli, and spirochetes were negative. Concurrent plasma CMV DNA by NAAT was elevated at 5,530 IU/mL.
Given her immunocompromised status, close coordination with the infectious disease team was undertaken, and the patient was initiated on intravenous ganciclovir therapy.
Discussion: This case highlights the importance of maintaining a broad differential diagnosis when evaluating gastric mucosal changes in immunosuppressed patients with cirrhosis. While erythema is commonly attributed to portal hypertensive gastropathy (PHG), PHG often has characteristic endoscopic findings such as a mosaic pattern, red spots, or diffuse congestion. When mucosal changes are atypical or deviate from these patterns, clinicians should have a lower threshold to obtain biopsies. Histologic evaluation remains essential, especially in those with immune dysfunction, where clinical and visual findings may be nonspecific. Early recognition and multidisciplinary coordination enabled timely initiation of appropriate antiviral therapy.
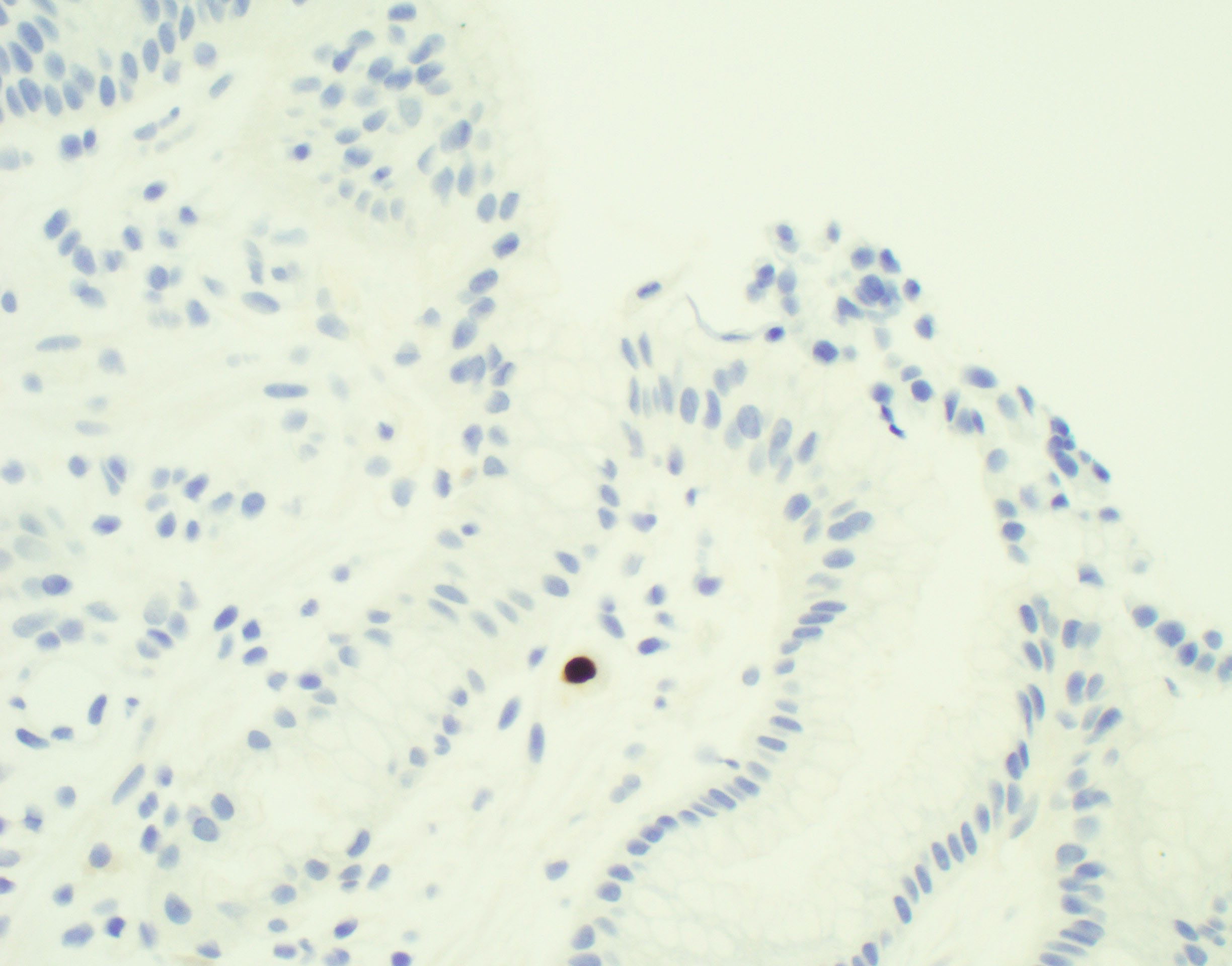
Figure: CMV immunohistochemical stain highlighting staining in rare CMV inclusions
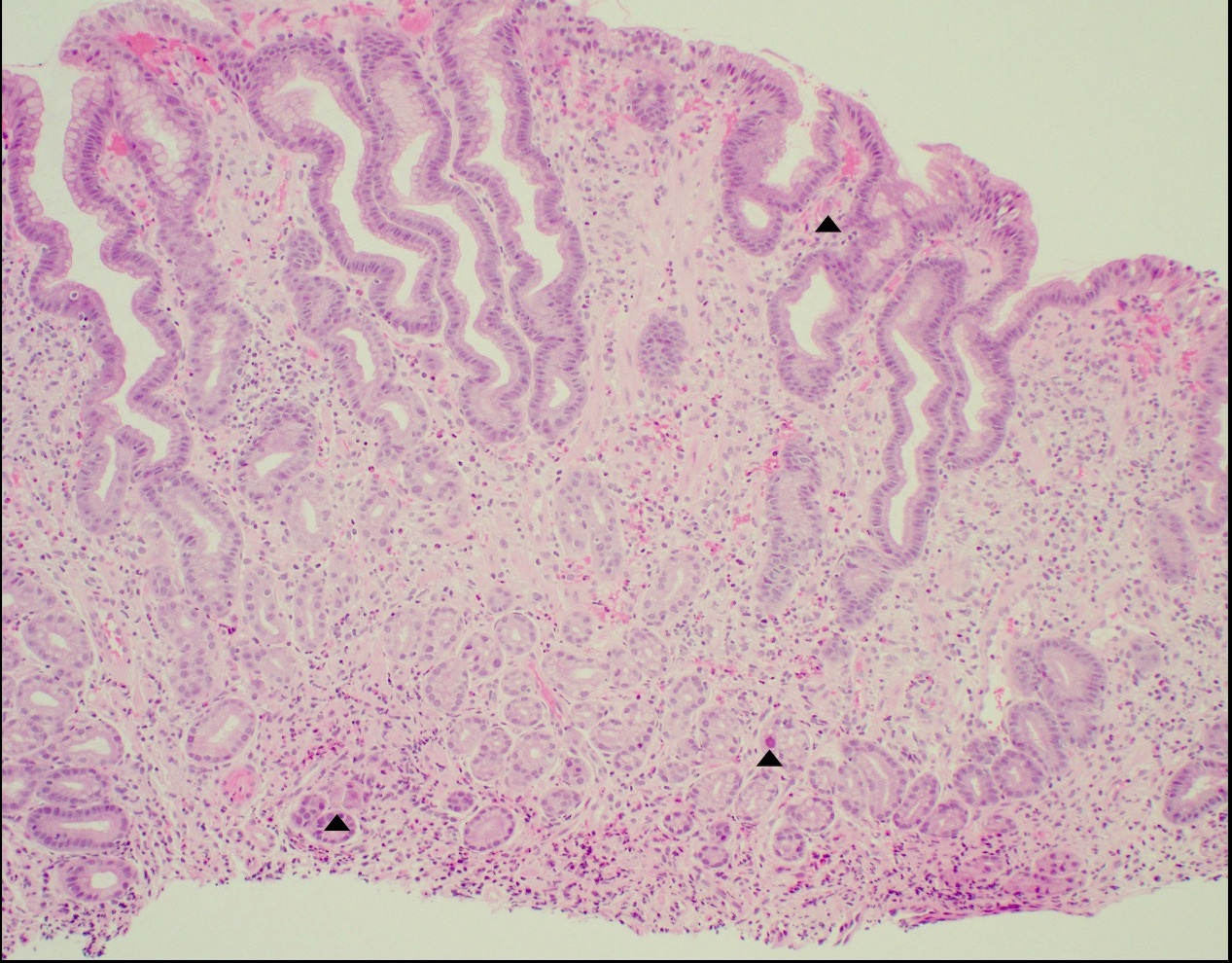
Figure: Chronic active gastritis with CMV inclusions
Disclosures:
Mina Awadallah indicated no relevant financial relationships.
Viveksandeep Thoguluva Chandrasekar indicated no relevant financial relationships.
Jolanta Jedrzkiewicz indicated no relevant financial relationships.
Rebecca Kim indicated no relevant financial relationships.
John Erikson Yap: Phathom Pharmaceutical – Speakers Bureau. Steris – Consultant.
Mina Awadallah, MD, MSc1, Viveksandeep Thoguluva Chandrasekar, MBBS2, Jolanta Jedrzkiewicz, MD1, Rebecca G. Kim, MD, MAS3, John Erikson Yap, MD, MBA, FACG3. P5053 - From Varices to Viral Infiltrate: Diagnosing CMV Gastritis in a Cirrhotic, Immunocompromised Host, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Utah, Salt Lake City, UT; 2Medical College of Georgia at Augusta University, Augusta, GA; 3University of Utah Health, Salt Lake City, UT
Introduction: Cytomegalovirus (CMV) gastritis is a rare but important cause of upper gastrointestinal pathology, most often identified in immunocompromised individuals. In patients with cirrhosis and overlapping immunosuppressive conditions, CMV involvement of the upper GI tract may be overlooked, as symptoms are frequently attributed to portal gastropathy. We present a case of biopsy-proven CMV gastritis in a patient with metabolic-associated steatohepatitis (MASH) cirrhosis and chronic B-cell depletion from long-term rituximab therapy.
Case Description/
Methods: A 68-year-old woman with compensated MASH cirrhosis, morbid obesity, rheumatoid arthritis (on rituximab for 9 years), interstitial lung disease (on fluticasone furoate/umeclidinium/vilanterol), atrial fibrillation on anticoagulation, prediabetes, hypothyroidism, and depression underwent upper endoscopy for variceal screening. She was found to have large esophageal varices, which were successfully banded. In addition, mucosal erythema was noted in the gastric body. The appearance was not consistent with typical portal hypertensive gastropathy, prompting biopsy for further evaluation.
Gastric biopsies demonstrated mildly active chronic gastritis with viral cytopathic changes consistent with CMV, confirmed by positive immunohistochemical staining. H. pylori was negative. The inflammatory infiltrate included eosinophils and CD68-positive histiocytes. Special stains for fungi, acid-fast bacilli, and spirochetes were negative. Concurrent plasma CMV DNA by NAAT was elevated at 5,530 IU/mL.
Given her immunocompromised status, close coordination with the infectious disease team was undertaken, and the patient was initiated on intravenous ganciclovir therapy.
Discussion: This case highlights the importance of maintaining a broad differential diagnosis when evaluating gastric mucosal changes in immunosuppressed patients with cirrhosis. While erythema is commonly attributed to portal hypertensive gastropathy (PHG), PHG often has characteristic endoscopic findings such as a mosaic pattern, red spots, or diffuse congestion. When mucosal changes are atypical or deviate from these patterns, clinicians should have a lower threshold to obtain biopsies. Histologic evaluation remains essential, especially in those with immune dysfunction, where clinical and visual findings may be nonspecific. Early recognition and multidisciplinary coordination enabled timely initiation of appropriate antiviral therapy.
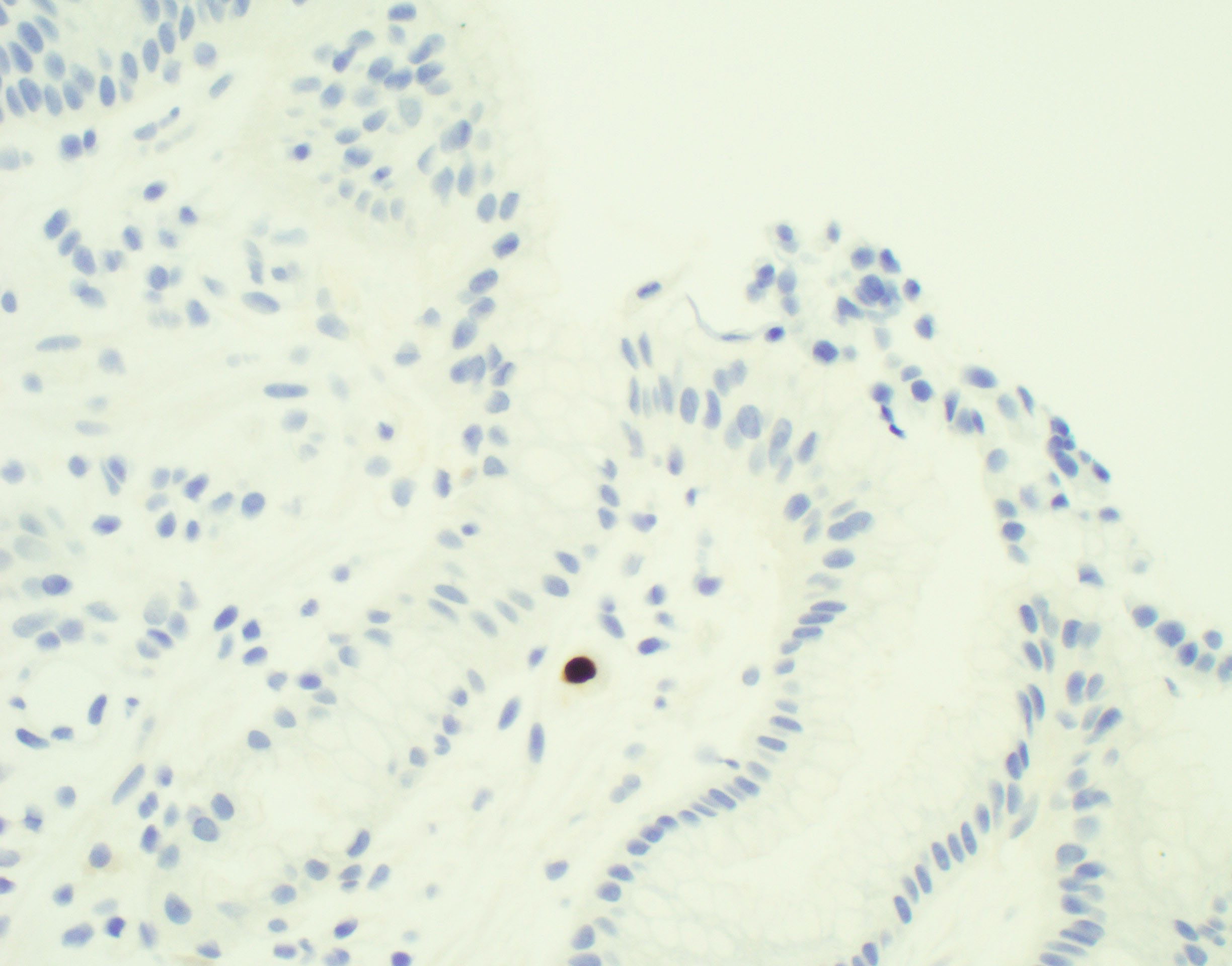
Figure: CMV immunohistochemical stain highlighting staining in rare CMV inclusions
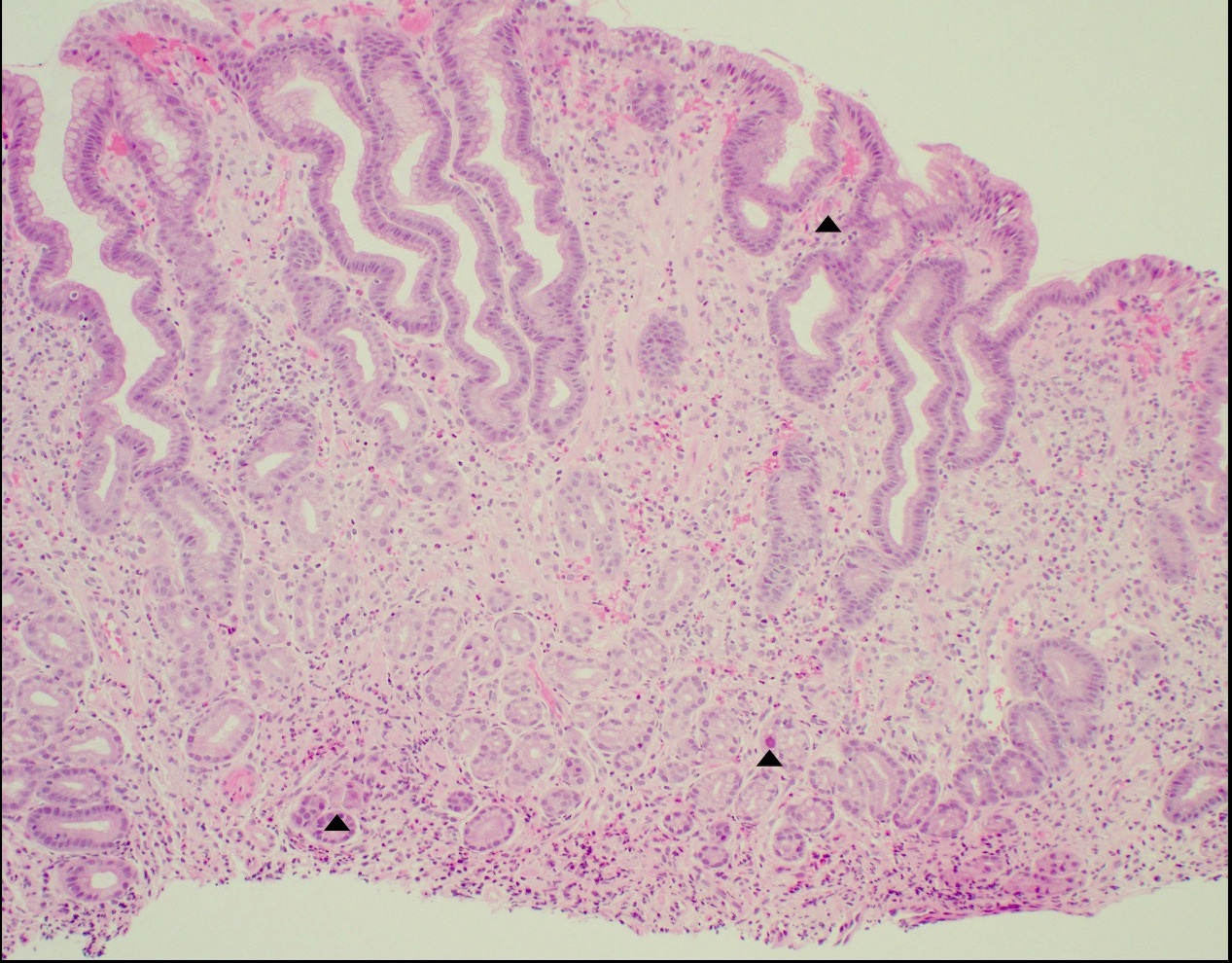
Figure: Chronic active gastritis with CMV inclusions
Disclosures:
Mina Awadallah indicated no relevant financial relationships.
Viveksandeep Thoguluva Chandrasekar indicated no relevant financial relationships.
Jolanta Jedrzkiewicz indicated no relevant financial relationships.
Rebecca Kim indicated no relevant financial relationships.
John Erikson Yap: Phathom Pharmaceutical – Speakers Bureau. Steris – Consultant.
Mina Awadallah, MD, MSc1, Viveksandeep Thoguluva Chandrasekar, MBBS2, Jolanta Jedrzkiewicz, MD1, Rebecca G. Kim, MD, MAS3, John Erikson Yap, MD, MBA, FACG3. P5053 - From Varices to Viral Infiltrate: Diagnosing CMV Gastritis in a Cirrhotic, Immunocompromised Host, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

