Tuesday Poster Session
Category: Esophagus
P5028 - An Uncommon Cause of Dysphagia: Bullous Pemphigoid with Esophageal Manifestations
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mujtaba Moazzam, MD
Corewell Health William Beaumont University Hospital
Royal Oak, MI
Presenting Author(s)
Mujtaba Moazzam, MD1, Usman Bin Hameed, MD1, Aleena Sharif, MBBS2, Nishant Aggarwal, MD1
1Corewell Health William Beaumont University Hospital, Royal Oak, MI; 2Sheikh Zayed Medical College Raheem Yar Khan, Bahawalpur, Punjab, Pakistan
Introduction: Bullous pemphigoid (BP) is an autoimmune blistering disorder commonly affecting elderly individuals, characterized by subepidermal bullae due to IgG autoantibody deposition at the basement membrane. While mucosal involvement is uncommon, esophageal manifestations occur in approximately 4% of cases and may mimic gastroesophageal reflux disease (GERD) or esophageal strictures.
Case Description/
Methods: An 83-year-old woman with GERD and a history of esophageal stricture status post multiple dilations (most recently 4 years ago with a 58F Maloney dilator) presented with tense, pruritic, and painful skin blisters. Punch biopsy of the right thigh showed subepidermal blisters with eosinophils. Direct immunofluorescence demonstrated linear IgG and C3 deposition at the dermoepidermal junction, confirming bullous pemphigoid.
During hospitalization, she developed progressive dysphagia and odynophagia. Given her esophageal history, concern was raised for mucosal BP involvement. Esophagogastroduodenoscopy (EGD) revealed concentric rings and mildly abnormal mucosa in the distal esophagus. The upper esophagus appeared normal. Biopsies from the proximal and distal esophagus showed squamous epithelium with mild reactive changes and no eosinophils, ruling out eosinophilic esophagitis. Immunofluorescence confirmed linear IgG and C3 at the dermoepidermal junction in the esophageal mucosa.
She was started on oral prednisone 40 mg daily, topical betamethasone dipropionate, and loratadine. Proton pump inhibitors and a mechanical soft diet improved her dysphagia. She was discharged with outpatient gastroenterology and dermatology follow-up.
Discussion: This case underscores the importance of considering bullous pemphigoid in atypical esophageal symptoms. Esophageal BP presents variably—from asymptomatic bullae to dysphagia, webs, strictures, bleeding, or sloughing esophagitis—and may mimic eosinophilic esophagitis, as in our case. Endoscopic biopsy with immunofluorescence is essential for diagnosis. Management typically involves systemic corticosteroids; immunosuppressants like mycophenolate or rituximab may be used for refractory cases. Adjunctive therapies include acid suppression, diet modification, and cautious endoscopic dilation if strictures develop. Early recognition is key to preventing complications, and interdisciplinary care between dermatology and gastroenterology ensures optimal outcomes.
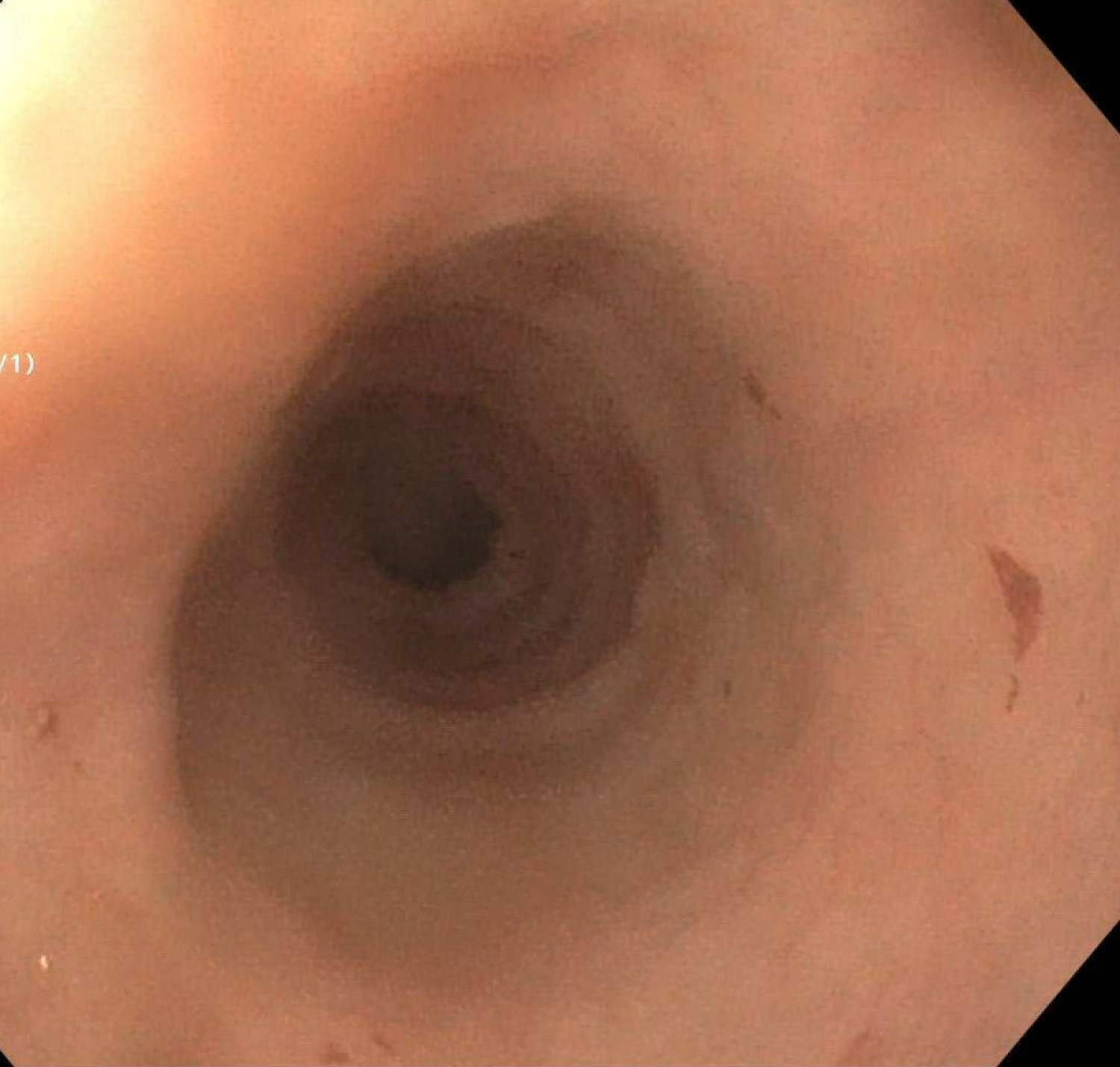
Figure: Endoscopy demonstrating concentric rings
Disclosures:
Mujtaba Moazzam indicated no relevant financial relationships.
Usman Bin Hameed indicated no relevant financial relationships.
Aleena Sharif indicated no relevant financial relationships.
Nishant Aggarwal indicated no relevant financial relationships.
Mujtaba Moazzam, MD1, Usman Bin Hameed, MD1, Aleena Sharif, MBBS2, Nishant Aggarwal, MD1. P5028 - An Uncommon Cause of Dysphagia: Bullous Pemphigoid with Esophageal Manifestations, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Corewell Health William Beaumont University Hospital, Royal Oak, MI; 2Sheikh Zayed Medical College Raheem Yar Khan, Bahawalpur, Punjab, Pakistan
Introduction: Bullous pemphigoid (BP) is an autoimmune blistering disorder commonly affecting elderly individuals, characterized by subepidermal bullae due to IgG autoantibody deposition at the basement membrane. While mucosal involvement is uncommon, esophageal manifestations occur in approximately 4% of cases and may mimic gastroesophageal reflux disease (GERD) or esophageal strictures.
Case Description/
Methods: An 83-year-old woman with GERD and a history of esophageal stricture status post multiple dilations (most recently 4 years ago with a 58F Maloney dilator) presented with tense, pruritic, and painful skin blisters. Punch biopsy of the right thigh showed subepidermal blisters with eosinophils. Direct immunofluorescence demonstrated linear IgG and C3 deposition at the dermoepidermal junction, confirming bullous pemphigoid.
During hospitalization, she developed progressive dysphagia and odynophagia. Given her esophageal history, concern was raised for mucosal BP involvement. Esophagogastroduodenoscopy (EGD) revealed concentric rings and mildly abnormal mucosa in the distal esophagus. The upper esophagus appeared normal. Biopsies from the proximal and distal esophagus showed squamous epithelium with mild reactive changes and no eosinophils, ruling out eosinophilic esophagitis. Immunofluorescence confirmed linear IgG and C3 at the dermoepidermal junction in the esophageal mucosa.
She was started on oral prednisone 40 mg daily, topical betamethasone dipropionate, and loratadine. Proton pump inhibitors and a mechanical soft diet improved her dysphagia. She was discharged with outpatient gastroenterology and dermatology follow-up.
Discussion: This case underscores the importance of considering bullous pemphigoid in atypical esophageal symptoms. Esophageal BP presents variably—from asymptomatic bullae to dysphagia, webs, strictures, bleeding, or sloughing esophagitis—and may mimic eosinophilic esophagitis, as in our case. Endoscopic biopsy with immunofluorescence is essential for diagnosis. Management typically involves systemic corticosteroids; immunosuppressants like mycophenolate or rituximab may be used for refractory cases. Adjunctive therapies include acid suppression, diet modification, and cautious endoscopic dilation if strictures develop. Early recognition is key to preventing complications, and interdisciplinary care between dermatology and gastroenterology ensures optimal outcomes.
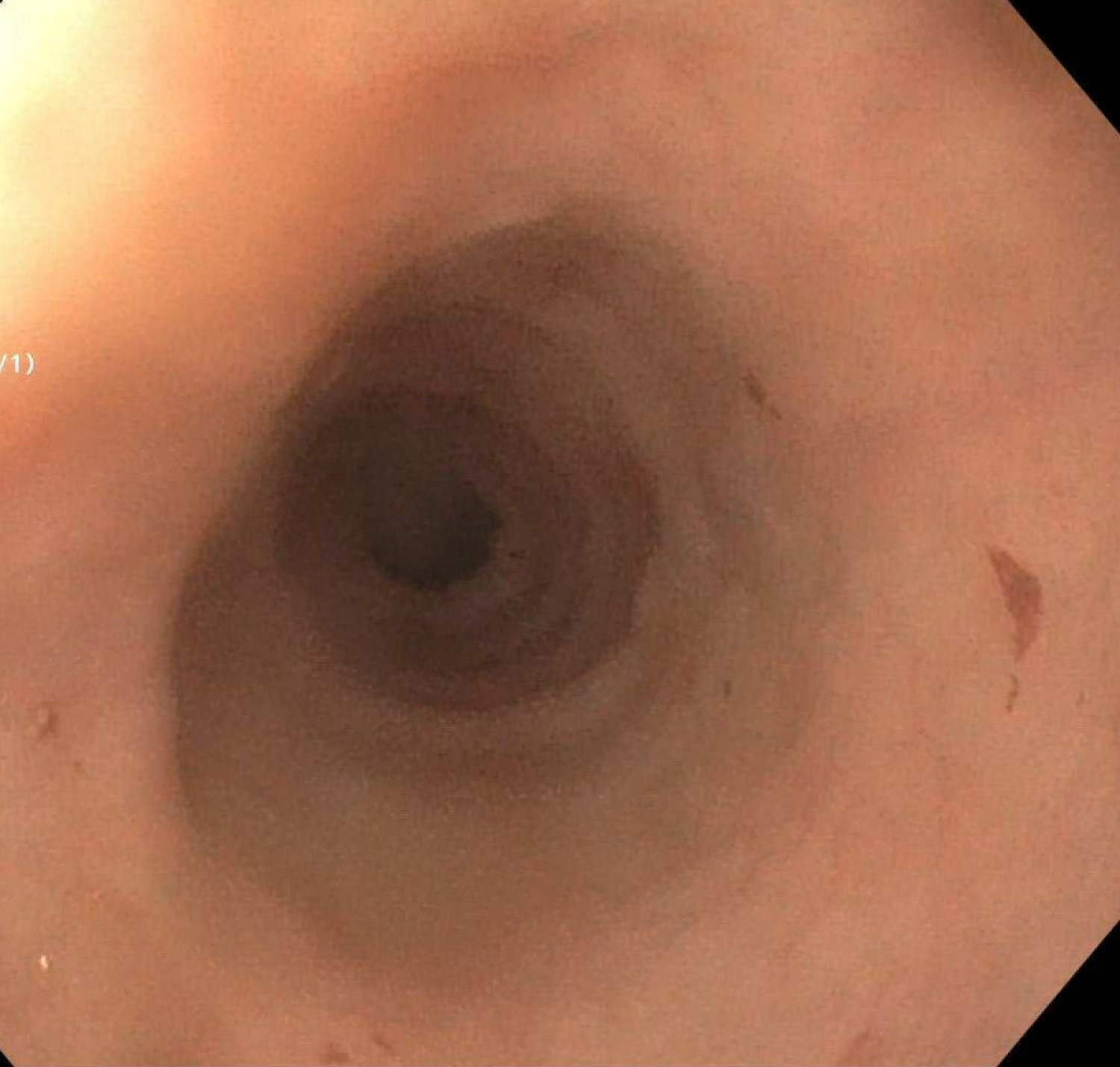
Figure: Endoscopy demonstrating concentric rings
Disclosures:
Mujtaba Moazzam indicated no relevant financial relationships.
Usman Bin Hameed indicated no relevant financial relationships.
Aleena Sharif indicated no relevant financial relationships.
Nishant Aggarwal indicated no relevant financial relationships.
Mujtaba Moazzam, MD1, Usman Bin Hameed, MD1, Aleena Sharif, MBBS2, Nishant Aggarwal, MD1. P5028 - An Uncommon Cause of Dysphagia: Bullous Pemphigoid with Esophageal Manifestations, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

