Tuesday Poster Session
Category: Esophagus
P5027 - Endoscopic Vacuum Therapy for Postoperative Esophageal Perforation: A Minimally Invasive Salvage Approach With Complete Healing
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mujtaba Moazzam, MD
Corewell Health William Beaumont University Hospital
Royal Oak, MI
Presenting Author(s)
Usenko Olexandr Yu, MD, DSCi1, Marko Kozyk, MD2, Ivan S. Tereshkevych, MD, PhD1, Ivan V. Babii, MD1, Oleksandr M. Sanzharov, MD1, Oleksandra Kozyk, 3, Olena Strubchevska, 4, Sushrut Ingawale, MD, DNB, MBBS5, Mujtaba Moazzam, MD2, Usman Bin Hameed, MD2, Kateryna Strubchevska, MD2
1Shalimov National Scientific Center of Surgery and Transplantology, Kyiv, Kyyiv, Ukraine; 2Corewell Health William Beaumont University Hospital, Royal Oak, MI; 3Williamette Univeristy, Salem, OR; 4Jagiellonian University Medical College, Krakow, Malopolskie, Poland; 5Quinnipiac University - Frank H Netter MD School of Medicine, Bridgeport, CT
Introduction: Esophageal perforation remains a life-threatening complication with significant morbidity. Traditional management includes surgical repair or esophageal stenting, but each approach carries limitations—ranging from procedural morbidity to incomplete defect sealing and stent migration. Endoscopic vacuum therapy (EVT), a minimally invasive technique that applies negative pressure to a polyurethane sponge placed endoscopically, has emerged as a promising alternative. EVT promotes wound granulation, controls infection through continuous drainage, and enables real-time monitoring.
Case Description/
Methods: A 27-year-old woman with achalasia underwent laparoscopic Heller myotomy with Dor fundoplication. Postoperatively, she developed gastric content leakage through her drain. Imaging and EGD revealed a large distal esophageal defect with exposed intra-abdominal drains. She underwent relaparoscopy with drainage and jejunostomy, followed by an interdisciplinary decision to initiate EVT. A custom Endovac system was constructed using a duodenal tube and polypropylene sponge, exchanged every 3–5 days. Over 27 days, seven EVT sessions were performed. Endoscopic reassessment showed progressive healing: initial wound edge debridement and granulation by session 1, near-complete defect closure with small residual fistulas by session 4, and full epithelialization with cicatricial remodeling by session 6. The patient resumed oral intake, was discharged in stable condition, and had a normal follow-up EGD at 2.5 months.
Discussion: This case illustrates EVT’s value as a first-line salvage therapy for transmural esophageal defects. Compared to stents—which seal but do not drain—EVT achieves superior outcomes by simultaneously closing the defect and evacuating septic fluid. Recent meta-analyses cite EVT closure rates of 85–90%, exceeding the 70–78% success seen with esophageal stents. EVT is also associated with fewer adverse events and reduced mortality. Though it necessitates multiple endoscopic sessions and inpatient care, it has a favorable safety profile with low rates of strictures and bleeding. Early initiation correlates with higher success. Our patient’s complete healing without surgical revision underscores EVT’s potential to preserve esophageal integrity and avoid more invasive interventions. For gastroenterologists, especially those managing post-surgical leaks, EVT represents a paradigm shift in perforation care—minimally invasive, dynamic, and organ-sparing.
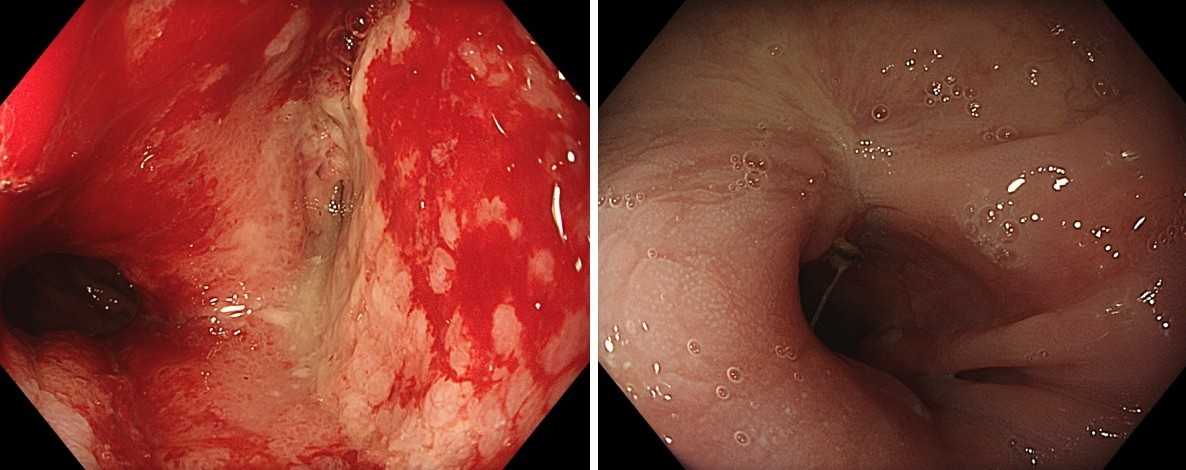
Figure: Left - After 1 EVT session; Right - After 4 EVT sessions
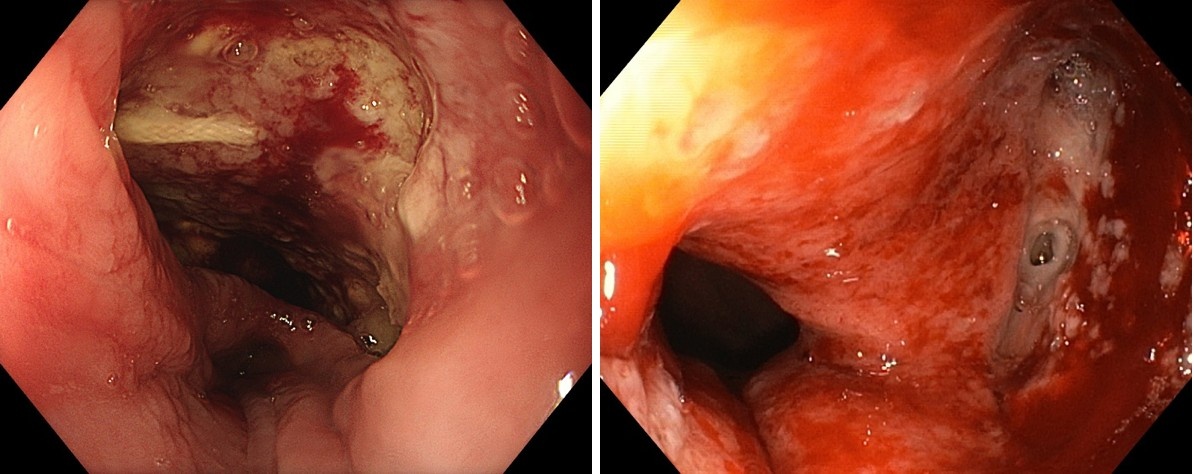
Figure: Left - After 6 EVT sessions; Right - 2 months after discharge
Disclosures:
Usenko Olexandr Yu indicated no relevant financial relationships.
Marko Kozyk indicated no relevant financial relationships.
Ivan S. Tereshkevych indicated no relevant financial relationships.
Ivan V. Babii indicated no relevant financial relationships.
Oleksandr M. Sanzharov indicated no relevant financial relationships.
Oleksandra Kozyk indicated no relevant financial relationships.
Olena Strubchevska indicated no relevant financial relationships.
Sushrut Ingawale indicated no relevant financial relationships.
Mujtaba Moazzam indicated no relevant financial relationships.
Usman Bin Hameed indicated no relevant financial relationships.
Kateryna Strubchevska indicated no relevant financial relationships.
Usenko Olexandr Yu, MD, DSCi1, Marko Kozyk, MD2, Ivan S. Tereshkevych, MD, PhD1, Ivan V. Babii, MD1, Oleksandr M. Sanzharov, MD1, Oleksandra Kozyk, 3, Olena Strubchevska, 4, Sushrut Ingawale, MD, DNB, MBBS5, Mujtaba Moazzam, MD2, Usman Bin Hameed, MD2, Kateryna Strubchevska, MD2. P5027 - Endoscopic Vacuum Therapy for Postoperative Esophageal Perforation: A Minimally Invasive Salvage Approach With Complete Healing, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Shalimov National Scientific Center of Surgery and Transplantology, Kyiv, Kyyiv, Ukraine; 2Corewell Health William Beaumont University Hospital, Royal Oak, MI; 3Williamette Univeristy, Salem, OR; 4Jagiellonian University Medical College, Krakow, Malopolskie, Poland; 5Quinnipiac University - Frank H Netter MD School of Medicine, Bridgeport, CT
Introduction: Esophageal perforation remains a life-threatening complication with significant morbidity. Traditional management includes surgical repair or esophageal stenting, but each approach carries limitations—ranging from procedural morbidity to incomplete defect sealing and stent migration. Endoscopic vacuum therapy (EVT), a minimally invasive technique that applies negative pressure to a polyurethane sponge placed endoscopically, has emerged as a promising alternative. EVT promotes wound granulation, controls infection through continuous drainage, and enables real-time monitoring.
Case Description/
Methods: A 27-year-old woman with achalasia underwent laparoscopic Heller myotomy with Dor fundoplication. Postoperatively, she developed gastric content leakage through her drain. Imaging and EGD revealed a large distal esophageal defect with exposed intra-abdominal drains. She underwent relaparoscopy with drainage and jejunostomy, followed by an interdisciplinary decision to initiate EVT. A custom Endovac system was constructed using a duodenal tube and polypropylene sponge, exchanged every 3–5 days. Over 27 days, seven EVT sessions were performed. Endoscopic reassessment showed progressive healing: initial wound edge debridement and granulation by session 1, near-complete defect closure with small residual fistulas by session 4, and full epithelialization with cicatricial remodeling by session 6. The patient resumed oral intake, was discharged in stable condition, and had a normal follow-up EGD at 2.5 months.
Discussion: This case illustrates EVT’s value as a first-line salvage therapy for transmural esophageal defects. Compared to stents—which seal but do not drain—EVT achieves superior outcomes by simultaneously closing the defect and evacuating septic fluid. Recent meta-analyses cite EVT closure rates of 85–90%, exceeding the 70–78% success seen with esophageal stents. EVT is also associated with fewer adverse events and reduced mortality. Though it necessitates multiple endoscopic sessions and inpatient care, it has a favorable safety profile with low rates of strictures and bleeding. Early initiation correlates with higher success. Our patient’s complete healing without surgical revision underscores EVT’s potential to preserve esophageal integrity and avoid more invasive interventions. For gastroenterologists, especially those managing post-surgical leaks, EVT represents a paradigm shift in perforation care—minimally invasive, dynamic, and organ-sparing.
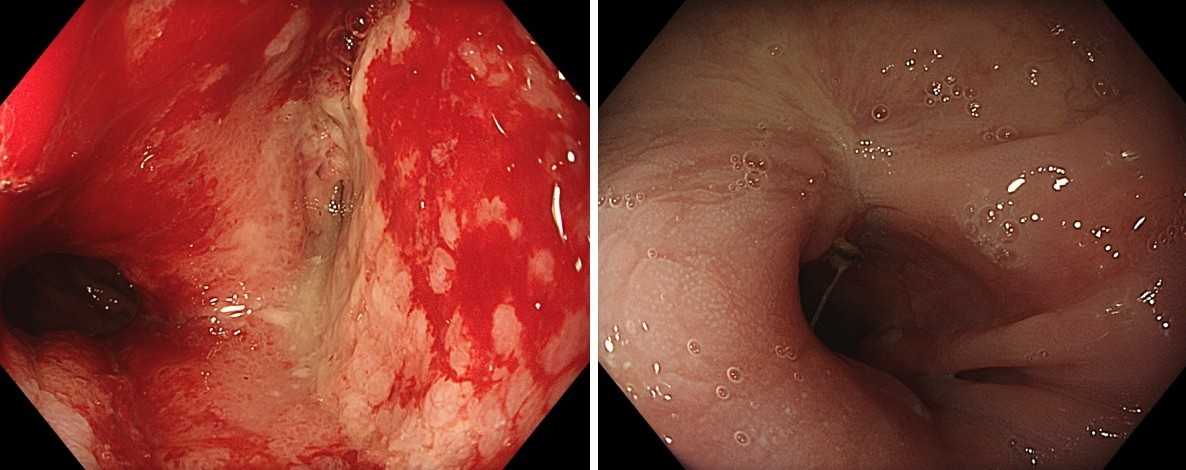
Figure: Left - After 1 EVT session; Right - After 4 EVT sessions
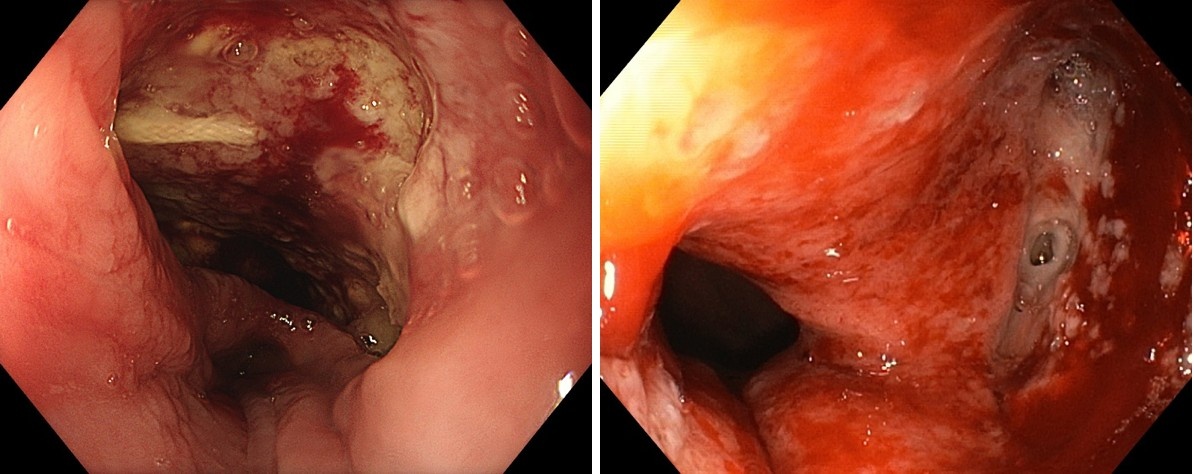
Figure: Left - After 6 EVT sessions; Right - 2 months after discharge
Disclosures:
Usenko Olexandr Yu indicated no relevant financial relationships.
Marko Kozyk indicated no relevant financial relationships.
Ivan S. Tereshkevych indicated no relevant financial relationships.
Ivan V. Babii indicated no relevant financial relationships.
Oleksandr M. Sanzharov indicated no relevant financial relationships.
Oleksandra Kozyk indicated no relevant financial relationships.
Olena Strubchevska indicated no relevant financial relationships.
Sushrut Ingawale indicated no relevant financial relationships.
Mujtaba Moazzam indicated no relevant financial relationships.
Usman Bin Hameed indicated no relevant financial relationships.
Kateryna Strubchevska indicated no relevant financial relationships.
Usenko Olexandr Yu, MD, DSCi1, Marko Kozyk, MD2, Ivan S. Tereshkevych, MD, PhD1, Ivan V. Babii, MD1, Oleksandr M. Sanzharov, MD1, Oleksandra Kozyk, 3, Olena Strubchevska, 4, Sushrut Ingawale, MD, DNB, MBBS5, Mujtaba Moazzam, MD2, Usman Bin Hameed, MD2, Kateryna Strubchevska, MD2. P5027 - Endoscopic Vacuum Therapy for Postoperative Esophageal Perforation: A Minimally Invasive Salvage Approach With Complete Healing, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
