Tuesday Poster Session
Category: Esophagus
P5016 - Esophageal Cast After Balloon Dilation in a Patient With Esophageal Stricture From Epidermolysis Bullosa Acquisita
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Kwabena Asafo-Agyei, MD
Medical College of Georgia at Augusta University
Evans, GA
Presenting Author(s)
Award: ACG Presidential Poster Award
Kwabena Asafo-Agyei, MD1, Sajid Ali, MD2, Anam Herekar, MD3, Amit Hudgi, MD4, Karansher Singh Randhawa, MBBS3, Leonard Little, MD5, Bianca Afonso, MD6, Suhas Sharma, MD6, Subbaramiah Sridhar, MD4
1Medical College of Georgia at Augusta University, Evans, GA; 2Aiken Regional Medical Center, Aiken, SC; 3Medical College of Georgia at Augusta University, Augusta, GA; 4Augusta University, Augusta, GA; 5VA AUGUSTA, Augusta, GA; 6VA Augusta, Augusta, GA
Introduction: Epidermolysis bullosa acquisita (EBA) is a rare, chronic autoimmune blistering disorder characterized by autoantibodies targeting type VII collagen, a key component of anchoring fibrils in the basement membrane. While primarily affecting the skin (non-inflammatory type), the mucosal involvement (inflammatory type) is possible. Esophageal involvement is particularly rare & may lead to serious complications such as dysphagia & strictures.
Case Description/
Methods:
A 42-year-old African American female with a known diagnosis of EBA presented with progressive dysphagia to both solids & liquids, choking episodes & occasional inability to tolerate secretions for the past 6 months. Her diet was reduced to pureed soups & nutritional shakes. An initial endoscopy (EGD) revealed a severe esophageal stricture at 25 cm from the incisors, characterized by sloughing mucosa & inability to advance even a pediatric scope (Figure 1). She was treated with intermittent prednisone, which provided partial symptomatic relief & was started on dupilumab by dermatology. The patient noted a reduction in blistering of the skin, but dysphagia persisted. She subsequently underwent a second EGD & at 25cm from the incisor, there was a circumferential stricture with a residual diameter of 5 mm. Using a guidewire, a through-the-scope balloon was advanced & the stricture was carefully dilated to 10mm. The inflated balloon was used as a guide & the endoscope was carefully advanced to the stomach. After deflating the balloon, we found a tubular cast of the esophageal lumen, which was carefully retrieved with a biopsy forceps & submitted for histology (Figure 2). The histology revealed features of EBA involving the esophagus. The patient was started on a proton pump inhibitor twice daily & oral budesonide. She subsequently had severe odynophagia after the procedure, which improved after the third repeat dilation to 15mm the following week.
Discussion: Our first-ever case highlights a rare but significant complication of EBA: esophageal involvement leading to dysphagia. EBA-associated strictures may mimic other causes of esophageal narrowing and are often diagnosed only after extensive evaluation. Treatment typically includes immunosuppressants such as corticosteroids, azathioprine, or biologic agents. Gastroenterologists need to recognize the rare complication of esophageal cast during dilations for strictures in patients with EBA to decrease post-procedural complications and improve outcomes.
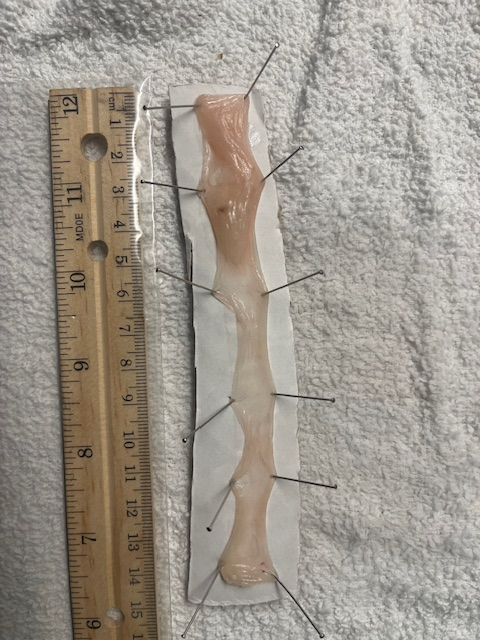
Figure: STRICTURE AND SLOUGHING OF THE MIDDLE ESOPHAGUS
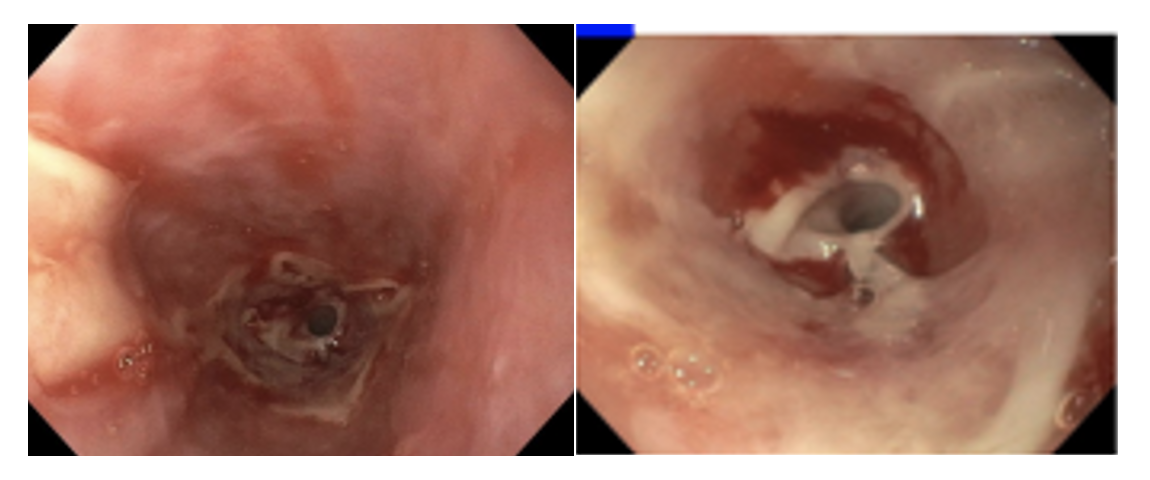
Figure: ESOPHAGEAL CAST
Disclosures:
Kwabena Asafo-Agyei indicated no relevant financial relationships.
Sajid Ali indicated no relevant financial relationships.
Anam Herekar indicated no relevant financial relationships.
Amit Hudgi indicated no relevant financial relationships.
Karansher Singh Randhawa indicated no relevant financial relationships.
Leonard Little indicated no relevant financial relationships.
Bianca Afonso indicated no relevant financial relationships.
Suhas Sharma indicated no relevant financial relationships.
Subbaramiah Sridhar indicated no relevant financial relationships.
Kwabena Asafo-Agyei, MD1, Sajid Ali, MD2, Anam Herekar, MD3, Amit Hudgi, MD4, Karansher Singh Randhawa, MBBS3, Leonard Little, MD5, Bianca Afonso, MD6, Suhas Sharma, MD6, Subbaramiah Sridhar, MD4. P5016 - Esophageal Cast After Balloon Dilation in a Patient With Esophageal Stricture From Epidermolysis Bullosa Acquisita, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Kwabena Asafo-Agyei, MD1, Sajid Ali, MD2, Anam Herekar, MD3, Amit Hudgi, MD4, Karansher Singh Randhawa, MBBS3, Leonard Little, MD5, Bianca Afonso, MD6, Suhas Sharma, MD6, Subbaramiah Sridhar, MD4
1Medical College of Georgia at Augusta University, Evans, GA; 2Aiken Regional Medical Center, Aiken, SC; 3Medical College of Georgia at Augusta University, Augusta, GA; 4Augusta University, Augusta, GA; 5VA AUGUSTA, Augusta, GA; 6VA Augusta, Augusta, GA
Introduction: Epidermolysis bullosa acquisita (EBA) is a rare, chronic autoimmune blistering disorder characterized by autoantibodies targeting type VII collagen, a key component of anchoring fibrils in the basement membrane. While primarily affecting the skin (non-inflammatory type), the mucosal involvement (inflammatory type) is possible. Esophageal involvement is particularly rare & may lead to serious complications such as dysphagia & strictures.
Case Description/
Methods:
A 42-year-old African American female with a known diagnosis of EBA presented with progressive dysphagia to both solids & liquids, choking episodes & occasional inability to tolerate secretions for the past 6 months. Her diet was reduced to pureed soups & nutritional shakes. An initial endoscopy (EGD) revealed a severe esophageal stricture at 25 cm from the incisors, characterized by sloughing mucosa & inability to advance even a pediatric scope (Figure 1). She was treated with intermittent prednisone, which provided partial symptomatic relief & was started on dupilumab by dermatology. The patient noted a reduction in blistering of the skin, but dysphagia persisted. She subsequently underwent a second EGD & at 25cm from the incisor, there was a circumferential stricture with a residual diameter of 5 mm. Using a guidewire, a through-the-scope balloon was advanced & the stricture was carefully dilated to 10mm. The inflated balloon was used as a guide & the endoscope was carefully advanced to the stomach. After deflating the balloon, we found a tubular cast of the esophageal lumen, which was carefully retrieved with a biopsy forceps & submitted for histology (Figure 2). The histology revealed features of EBA involving the esophagus. The patient was started on a proton pump inhibitor twice daily & oral budesonide. She subsequently had severe odynophagia after the procedure, which improved after the third repeat dilation to 15mm the following week.
Discussion: Our first-ever case highlights a rare but significant complication of EBA: esophageal involvement leading to dysphagia. EBA-associated strictures may mimic other causes of esophageal narrowing and are often diagnosed only after extensive evaluation. Treatment typically includes immunosuppressants such as corticosteroids, azathioprine, or biologic agents. Gastroenterologists need to recognize the rare complication of esophageal cast during dilations for strictures in patients with EBA to decrease post-procedural complications and improve outcomes.
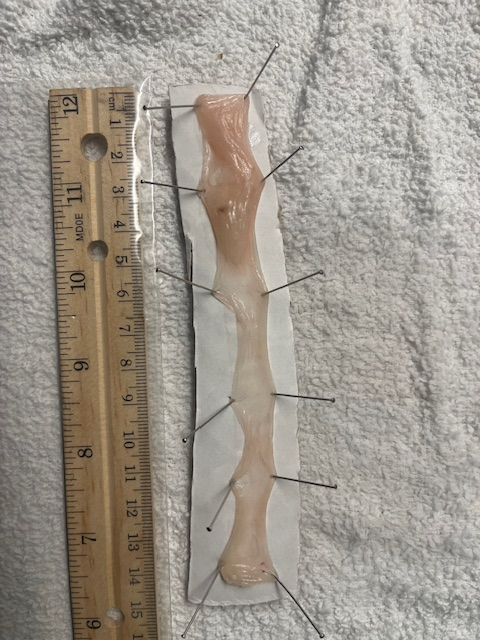
Figure: STRICTURE AND SLOUGHING OF THE MIDDLE ESOPHAGUS
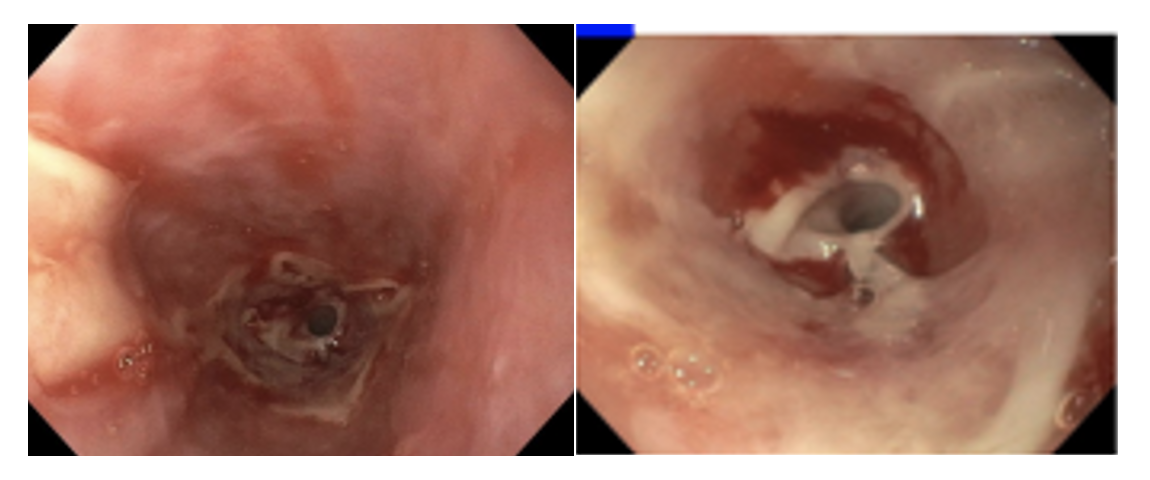
Figure: ESOPHAGEAL CAST
Disclosures:
Kwabena Asafo-Agyei indicated no relevant financial relationships.
Sajid Ali indicated no relevant financial relationships.
Anam Herekar indicated no relevant financial relationships.
Amit Hudgi indicated no relevant financial relationships.
Karansher Singh Randhawa indicated no relevant financial relationships.
Leonard Little indicated no relevant financial relationships.
Bianca Afonso indicated no relevant financial relationships.
Suhas Sharma indicated no relevant financial relationships.
Subbaramiah Sridhar indicated no relevant financial relationships.
Kwabena Asafo-Agyei, MD1, Sajid Ali, MD2, Anam Herekar, MD3, Amit Hudgi, MD4, Karansher Singh Randhawa, MBBS3, Leonard Little, MD5, Bianca Afonso, MD6, Suhas Sharma, MD6, Subbaramiah Sridhar, MD4. P5016 - Esophageal Cast After Balloon Dilation in a Patient With Esophageal Stricture From Epidermolysis Bullosa Acquisita, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

