Tuesday Poster Session
Category: Esophagus
P5015 - Swallowing the Truth: When Dysphagia Leads to a Schwannoma Surprise
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- JM
Jad Moumen, MD (he/him/his)
Albany Medical Center
Albany, NY
Presenting Author(s)
Jad Moumen, MD, Zarbakht Nisar, MBBS, Shamayel Safdar, MBBS, Mohsin Chundrigar, MBBS, Mahima Gill, MD
Albany Medical Center, Albany, NY
Introduction: Esophageal schwannoma, a relatively uncommon benign tumor arising from Schwann cells within the esophageal submucosa, comprises roughly 2% of esophageal neoplasms, with a female predilection. In fact, as of 2016 there were only 46 cases reported in the literature. While many patients remain asymptomatic, others may manifest a range of symptoms determined by tumor size and location, with dysphagia being the most prevalent. Diagnosis typically requires surgical resection or biopsy due to the nonspecific features observed on imaging studies. Here, we detail the case of a female patient presenting with dysphagia who was eventually found to have esophageal schwannoma.
Case Description/
Methods: A 59-year-old woman with a medical history of iatrogenic Cushing syndrome, diabetes, and hypothyroidism presented for evaluation of dysphagia and a globus sensation. CT imaging showed a peri-esophageal nodule measuring 1.0 × 1.0 × 1.3 cm. Esophagogastroduodenoscopy revealed a normal esophagus, and a single polyp was found in the stomach.
Endoscopic ultrasonography-guided fine-needle aspiration and histopathologic examination revealed bland spindle cells associated with a hardened vascular wall, consistent with a diagnosis of schwannoma. Since the patient’s symptoms were mild, she refused surgical evaluation and opted to repeat EUS after six months for monitoring.
Discussion: Symptoms related to esophageal schwannoma vary according to the location and size of the tumor. While most patients are asymptomatic, some can present with a variety of symptoms. Diagnosis can be established using various imaging techniques, including CT, MRI, and EUS; however, confirmation of the diagnosis requires pathologic examination after surgical resection or biopsy. EUS-FNA may be useful for both diagnosis and management of this tumor; however, diagnosis via biopsy can sometimes be challenging due to limited tissue availability and the submucosal benign tumor morphology.
The histologic features of schwannoma include spindle-shaped tumor cells arranged in a palisading pattern or with loose cellularity in a reticular array. Management depends on various factors, including symptoms, tumor size, and pathology. Resection of the tumor via surgery or endoscopy is the primary treatment, and complete excision usually suffices. Esophagectomy is reserved for cases with diffuse involvement.
Esophageal schwannoma, though rare, should be considered in submucosal esophageal masses, with treatment tailored to tumor specifics for optimal outcomes.
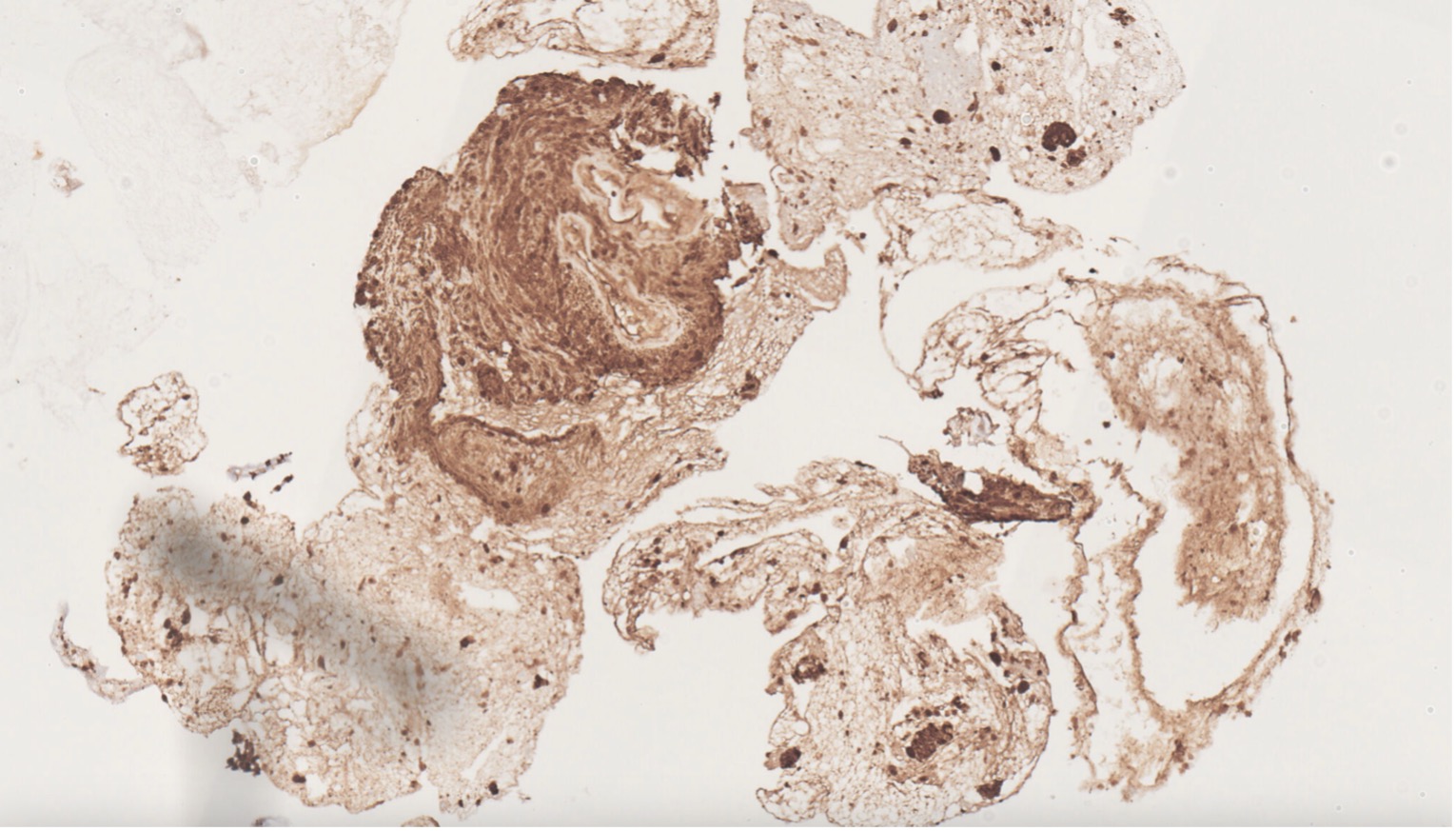
Figure: Immunohistochemical staining of a Schwannoma showing characteristic S100 positivity.
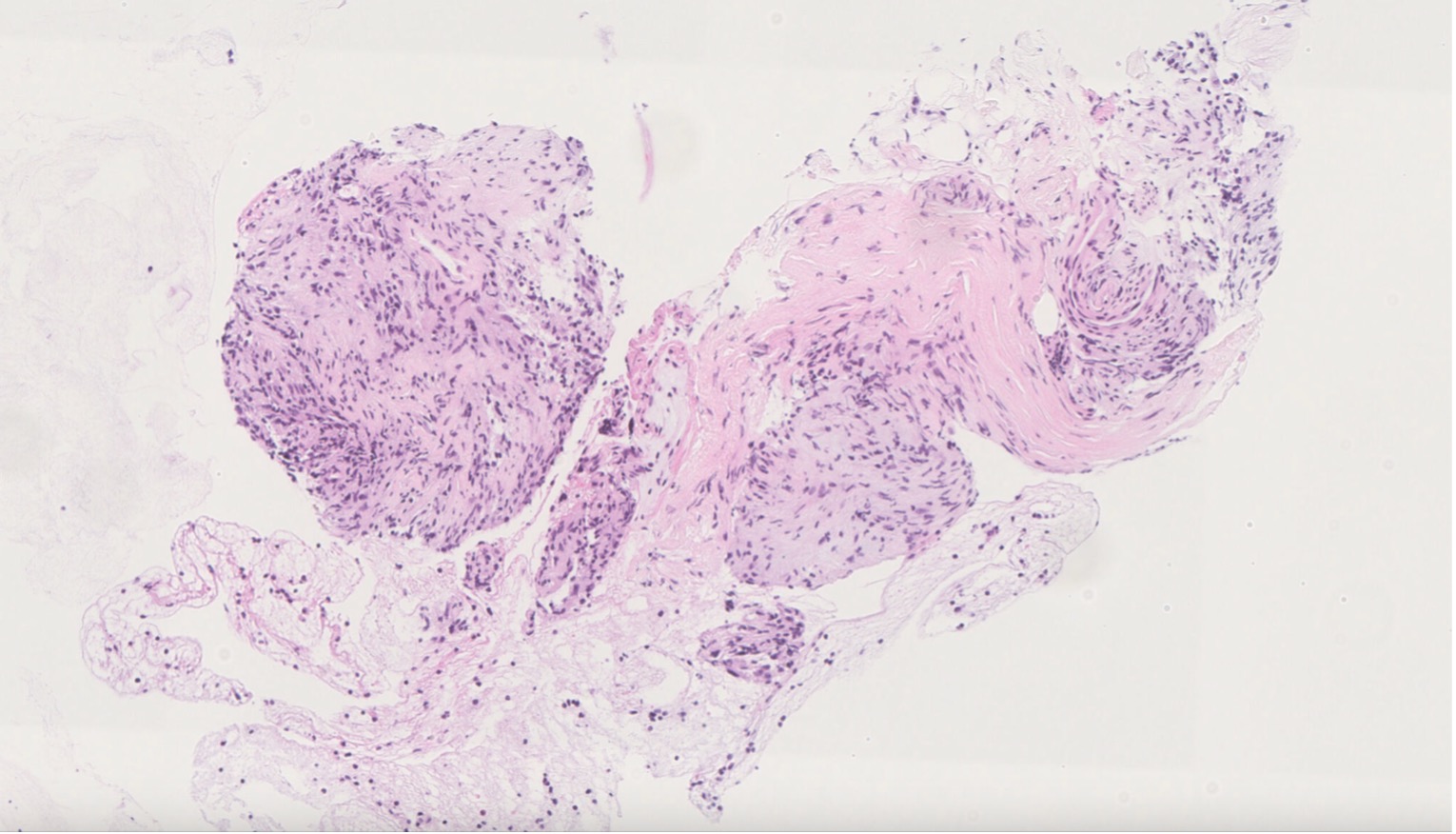
Figure: H&E stained histologic section of a Schwannoma, highlighting cellular Antoni A and myxoid Antoni B regions.
Disclosures:
Jad Moumen indicated no relevant financial relationships.
Zarbakht Nisar indicated no relevant financial relationships.
Shamayel Safdar indicated no relevant financial relationships.
Mohsin Chundrigar indicated no relevant financial relationships.
Mahima Gill indicated no relevant financial relationships.
Jad Moumen, MD, Zarbakht Nisar, MBBS, Shamayel Safdar, MBBS, Mohsin Chundrigar, MBBS, Mahima Gill, MD. P5015 - Swallowing the Truth: When Dysphagia Leads to a Schwannoma Surprise, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Albany Medical Center, Albany, NY
Introduction: Esophageal schwannoma, a relatively uncommon benign tumor arising from Schwann cells within the esophageal submucosa, comprises roughly 2% of esophageal neoplasms, with a female predilection. In fact, as of 2016 there were only 46 cases reported in the literature. While many patients remain asymptomatic, others may manifest a range of symptoms determined by tumor size and location, with dysphagia being the most prevalent. Diagnosis typically requires surgical resection or biopsy due to the nonspecific features observed on imaging studies. Here, we detail the case of a female patient presenting with dysphagia who was eventually found to have esophageal schwannoma.
Case Description/
Methods: A 59-year-old woman with a medical history of iatrogenic Cushing syndrome, diabetes, and hypothyroidism presented for evaluation of dysphagia and a globus sensation. CT imaging showed a peri-esophageal nodule measuring 1.0 × 1.0 × 1.3 cm. Esophagogastroduodenoscopy revealed a normal esophagus, and a single polyp was found in the stomach.
Endoscopic ultrasonography-guided fine-needle aspiration and histopathologic examination revealed bland spindle cells associated with a hardened vascular wall, consistent with a diagnosis of schwannoma. Since the patient’s symptoms were mild, she refused surgical evaluation and opted to repeat EUS after six months for monitoring.
Discussion: Symptoms related to esophageal schwannoma vary according to the location and size of the tumor. While most patients are asymptomatic, some can present with a variety of symptoms. Diagnosis can be established using various imaging techniques, including CT, MRI, and EUS; however, confirmation of the diagnosis requires pathologic examination after surgical resection or biopsy. EUS-FNA may be useful for both diagnosis and management of this tumor; however, diagnosis via biopsy can sometimes be challenging due to limited tissue availability and the submucosal benign tumor morphology.
The histologic features of schwannoma include spindle-shaped tumor cells arranged in a palisading pattern or with loose cellularity in a reticular array. Management depends on various factors, including symptoms, tumor size, and pathology. Resection of the tumor via surgery or endoscopy is the primary treatment, and complete excision usually suffices. Esophagectomy is reserved for cases with diffuse involvement.
Esophageal schwannoma, though rare, should be considered in submucosal esophageal masses, with treatment tailored to tumor specifics for optimal outcomes.
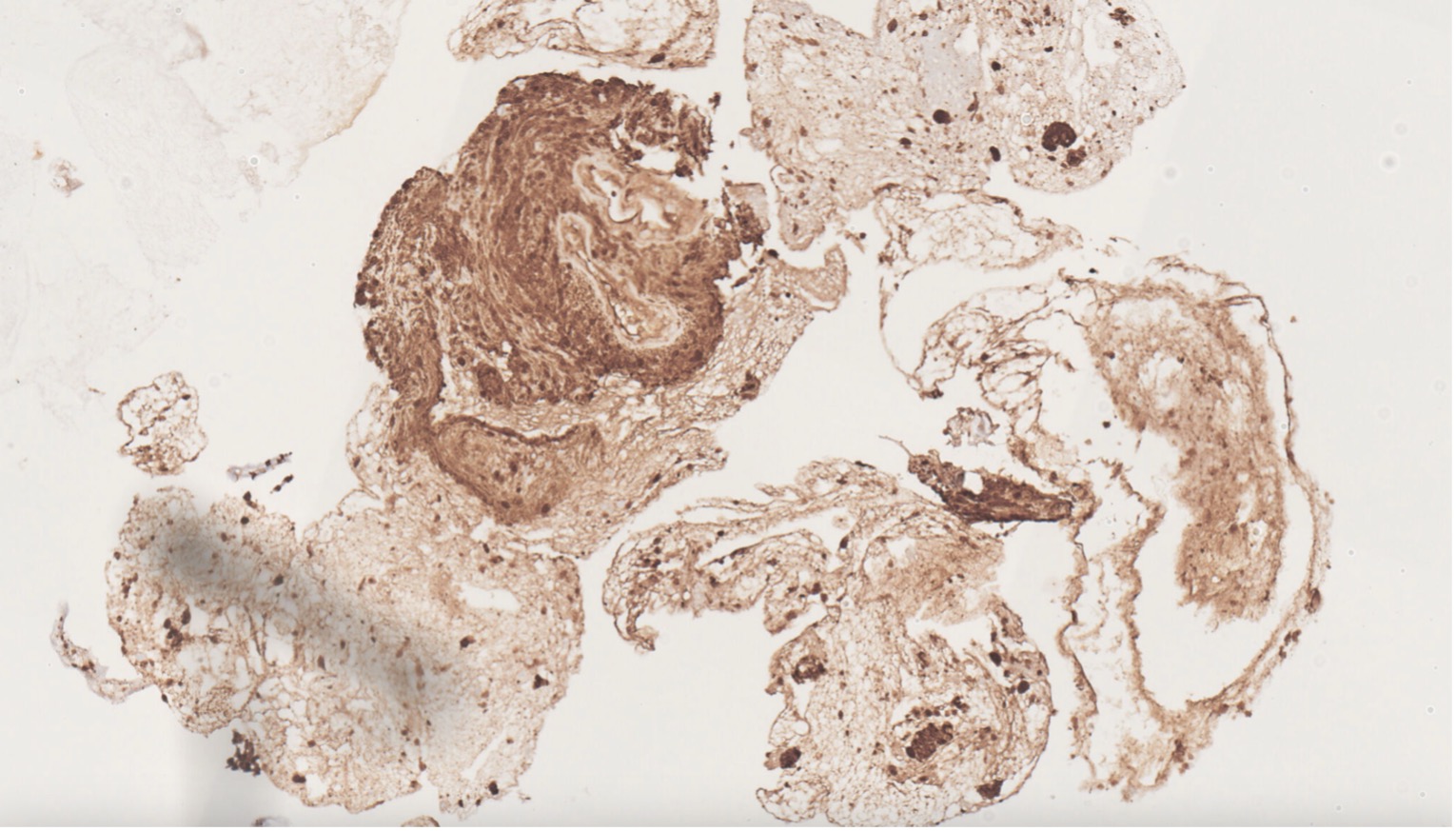
Figure: Immunohistochemical staining of a Schwannoma showing characteristic S100 positivity.
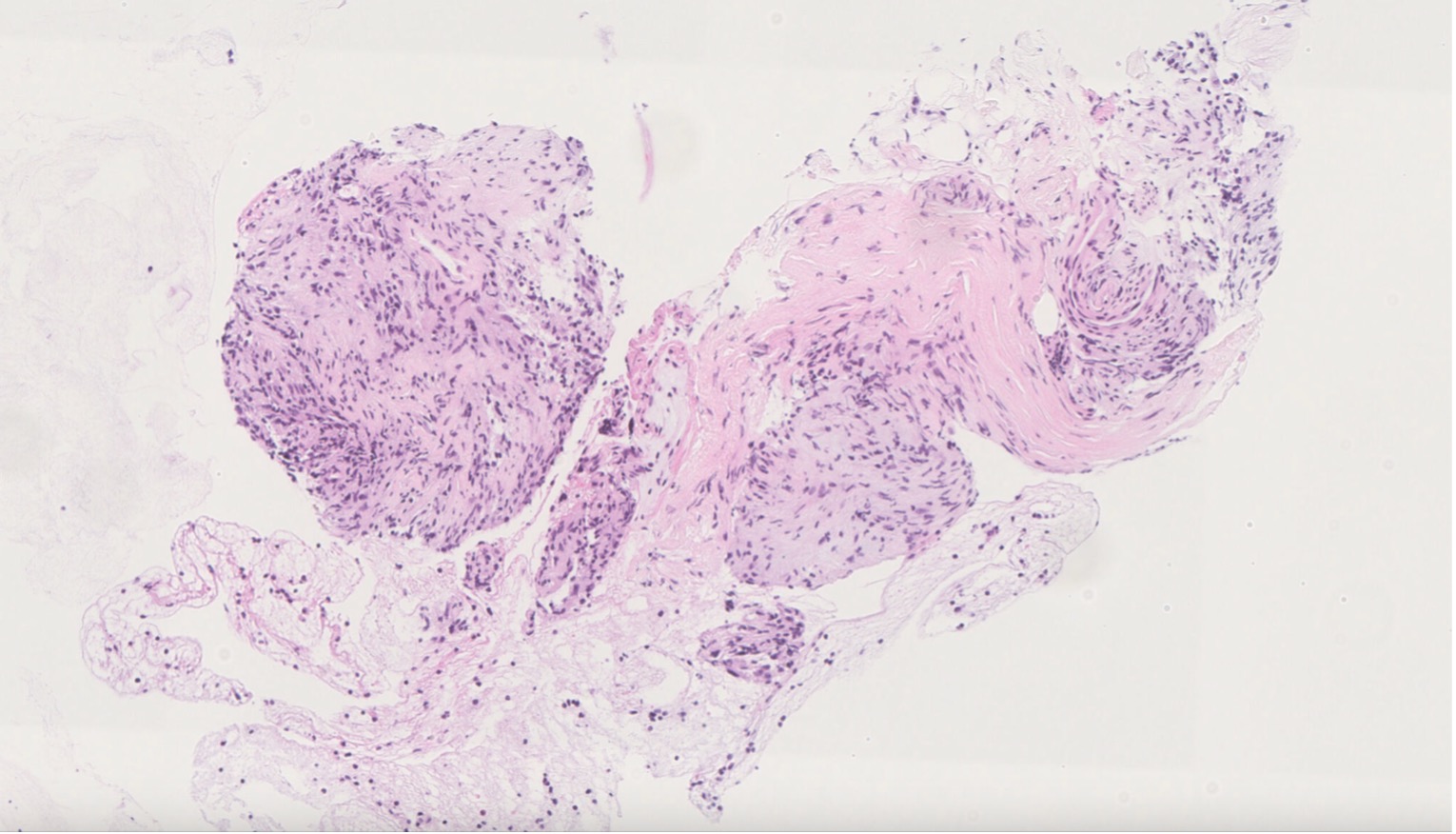
Figure: H&E stained histologic section of a Schwannoma, highlighting cellular Antoni A and myxoid Antoni B regions.
Disclosures:
Jad Moumen indicated no relevant financial relationships.
Zarbakht Nisar indicated no relevant financial relationships.
Shamayel Safdar indicated no relevant financial relationships.
Mohsin Chundrigar indicated no relevant financial relationships.
Mahima Gill indicated no relevant financial relationships.
Jad Moumen, MD, Zarbakht Nisar, MBBS, Shamayel Safdar, MBBS, Mohsin Chundrigar, MBBS, Mahima Gill, MD. P5015 - Swallowing the Truth: When Dysphagia Leads to a Schwannoma Surprise, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
