Tuesday Poster Session
Category: Esophagus
P5008 - Rituximab-Induced Esophageal Ulcers and Strictures Presenting as Dysphagia
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- MS
Muhammed Yaman Swied, MBBS
Southern Illinois University
Springfield, IL
Presenting Author(s)
Muhammed Yaman Swied, MBBS, Obada Daaboul, MD, Muaataz Azzawi, MD, Abdul Swied, MD
Southern Illinois University, Springfield, IL
Introduction: Rituximab is a monoclonal antibody that targets CD20 on B lymphocytes and is approved for treating multiple hematological and autoimmune disorders. Rituximab may cause gastrointestinal side effects like colitis, diarrhea, and bowel obstruction or perforation. Infusion-related reactions include throat irritation, but they are not linked to any specific esophageal disease. We report a rare case of rituximab-induced esophageal ulcers and strictures causing severe dysphagia.
Case Description/
Methods: A 53-year-old female with stage IV follicular lymphoma on rituximab presented to the clinic for evaluation of new-onset dysphagia. She underwent an esophagram that revealed nonspecific findings. She underwent esophagogastroduodenoscopy (EGD), revealing cratered and linear esophageal ulcers oozing blood throughout the esophagus, with two benign-appearing intrinsic moderate stenoses, traversed after dilation. Pathology revealed active esophagitis with ulceration, but was negative for Barrett's esophagus, malignancy, viral or fungal etiology. Despite being on omeprazole and then vonoprazan for two months, symptoms didn’t improve, prompting a repeat EGD that showed many linear and superficial esophageal ulcers with diffuse severe friability, erosions, sloughing, and ulceration. Pathology revealed ulceration with acute inflammation. After consulting with pathology, there was a suspicion that rituximab caused the esophageal injury, leading to its discontinuation. Eight months after stopping rituximab, the patient showed moderate symptomatic improvement. EGD revealed improvement in esophagitis and a benign stenosis, which was successfully dilated. Pathology showed no abnormalities
Discussion: Esophageal ulcers and strictures can arise from gastroesophageal reflux disease, medication, infections, eosinophilic esophagitis, radiation, chemotherapy, autoimmune disorders, caustic injury, or malignancy. Due to extensive mucosal sloughing and a positive pathergy sign, inflammatory disorders like Behçet’s disease were considered but ruled out by pathology, with an extensive evaluation, including history, labs, and biopsies, excluding most etiologies and identifying rituximab as the likely culprit, supported by symptom improvement after its discontinuation. This case highlights rituximab as a potential cause of esophageal ulcerations and strictures, causing dysphagia in the absence of other identifiable etiologies. Discontinuation or substitution with alternative agents may alleviate symptoms and confirm the diagnosis.
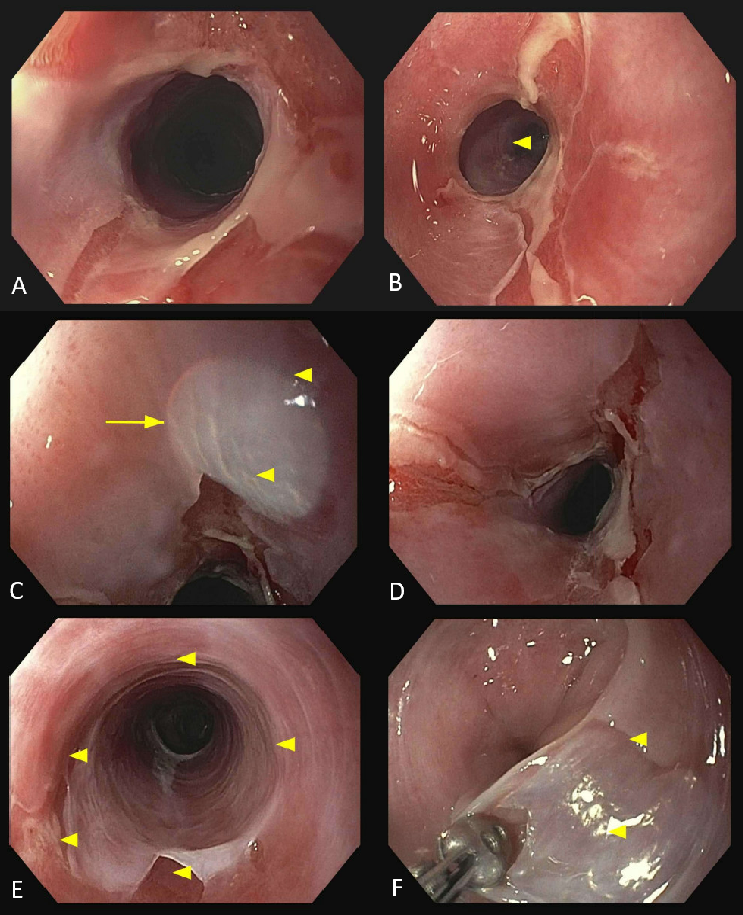
Figure: Endoscopic images of the esophagus from Esophagogastroduodenoscopies performed before discontinuation of rituximab therapy.
A: Upper third of the esophagus – Stenosis/Stricture
B: Lower third of the esophagus – Stenosis/Stricture
C: Middle third of the esophagus – Ulcer
D: Middle third of the esophagus – Ulcer
E & F: Epithelium sloughing
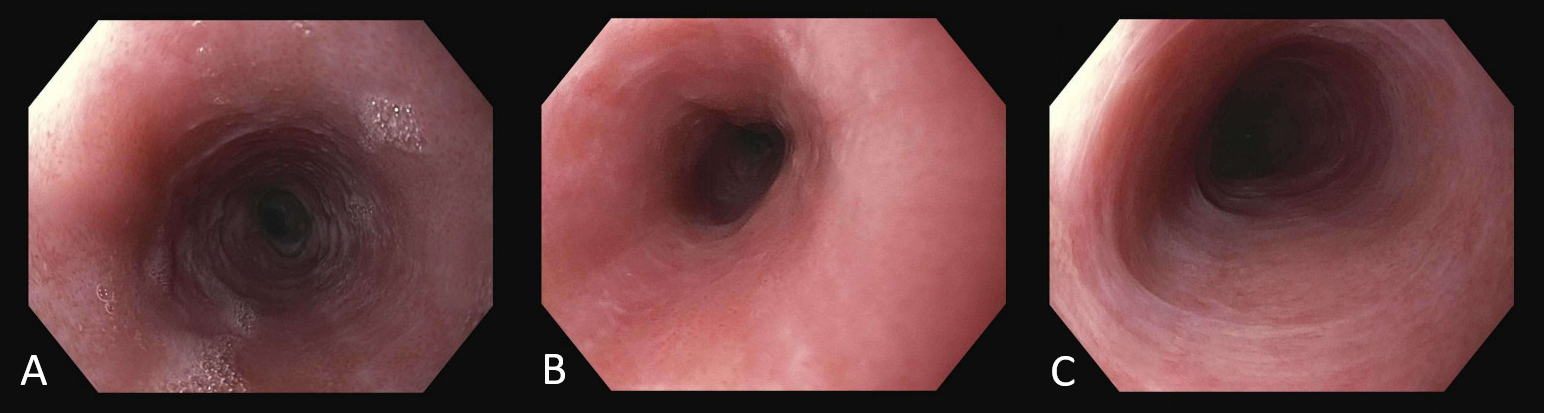
Figure: Endoscopic images of the esophagus from Esophagogastroduodenoscopy performed after discontinuation of rituximab therapy, showing improvement in ulcerations and inflammation.
A: Upper third of the esophagus – Improvement in ulceration and inflammation
B: Middle third of the esophagus – Improvement in ulceration and inflammation
C: Lower third of the esophagus – Improvement in ulceration and inflammation
Disclosures:
Muhammed Yaman Swied indicated no relevant financial relationships.
Obada Daaboul indicated no relevant financial relationships.
Muaataz Azzawi indicated no relevant financial relationships.
Abdul Swied indicated no relevant financial relationships.
Muhammed Yaman Swied, MBBS, Obada Daaboul, MD, Muaataz Azzawi, MD, Abdul Swied, MD. P5008 - Rituximab-Induced Esophageal Ulcers and Strictures Presenting as Dysphagia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Southern Illinois University, Springfield, IL
Introduction: Rituximab is a monoclonal antibody that targets CD20 on B lymphocytes and is approved for treating multiple hematological and autoimmune disorders. Rituximab may cause gastrointestinal side effects like colitis, diarrhea, and bowel obstruction or perforation. Infusion-related reactions include throat irritation, but they are not linked to any specific esophageal disease. We report a rare case of rituximab-induced esophageal ulcers and strictures causing severe dysphagia.
Case Description/
Methods: A 53-year-old female with stage IV follicular lymphoma on rituximab presented to the clinic for evaluation of new-onset dysphagia. She underwent an esophagram that revealed nonspecific findings. She underwent esophagogastroduodenoscopy (EGD), revealing cratered and linear esophageal ulcers oozing blood throughout the esophagus, with two benign-appearing intrinsic moderate stenoses, traversed after dilation. Pathology revealed active esophagitis with ulceration, but was negative for Barrett's esophagus, malignancy, viral or fungal etiology. Despite being on omeprazole and then vonoprazan for two months, symptoms didn’t improve, prompting a repeat EGD that showed many linear and superficial esophageal ulcers with diffuse severe friability, erosions, sloughing, and ulceration. Pathology revealed ulceration with acute inflammation. After consulting with pathology, there was a suspicion that rituximab caused the esophageal injury, leading to its discontinuation. Eight months after stopping rituximab, the patient showed moderate symptomatic improvement. EGD revealed improvement in esophagitis and a benign stenosis, which was successfully dilated. Pathology showed no abnormalities
Discussion: Esophageal ulcers and strictures can arise from gastroesophageal reflux disease, medication, infections, eosinophilic esophagitis, radiation, chemotherapy, autoimmune disorders, caustic injury, or malignancy. Due to extensive mucosal sloughing and a positive pathergy sign, inflammatory disorders like Behçet’s disease were considered but ruled out by pathology, with an extensive evaluation, including history, labs, and biopsies, excluding most etiologies and identifying rituximab as the likely culprit, supported by symptom improvement after its discontinuation. This case highlights rituximab as a potential cause of esophageal ulcerations and strictures, causing dysphagia in the absence of other identifiable etiologies. Discontinuation or substitution with alternative agents may alleviate symptoms and confirm the diagnosis.
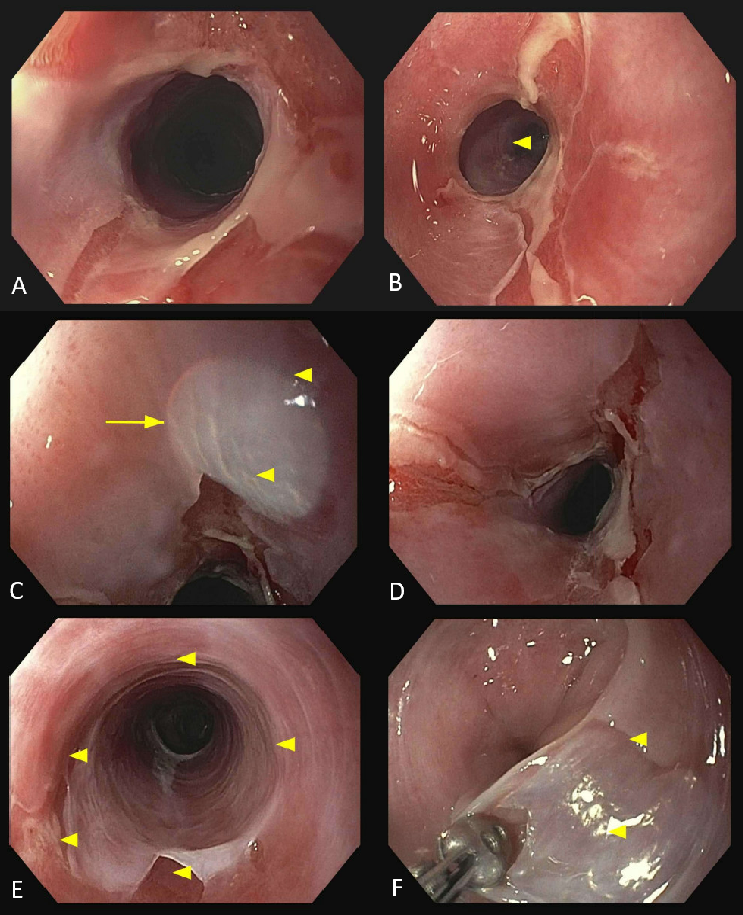
Figure: Endoscopic images of the esophagus from Esophagogastroduodenoscopies performed before discontinuation of rituximab therapy.
A: Upper third of the esophagus – Stenosis/Stricture
B: Lower third of the esophagus – Stenosis/Stricture
C: Middle third of the esophagus – Ulcer
D: Middle third of the esophagus – Ulcer
E & F: Epithelium sloughing
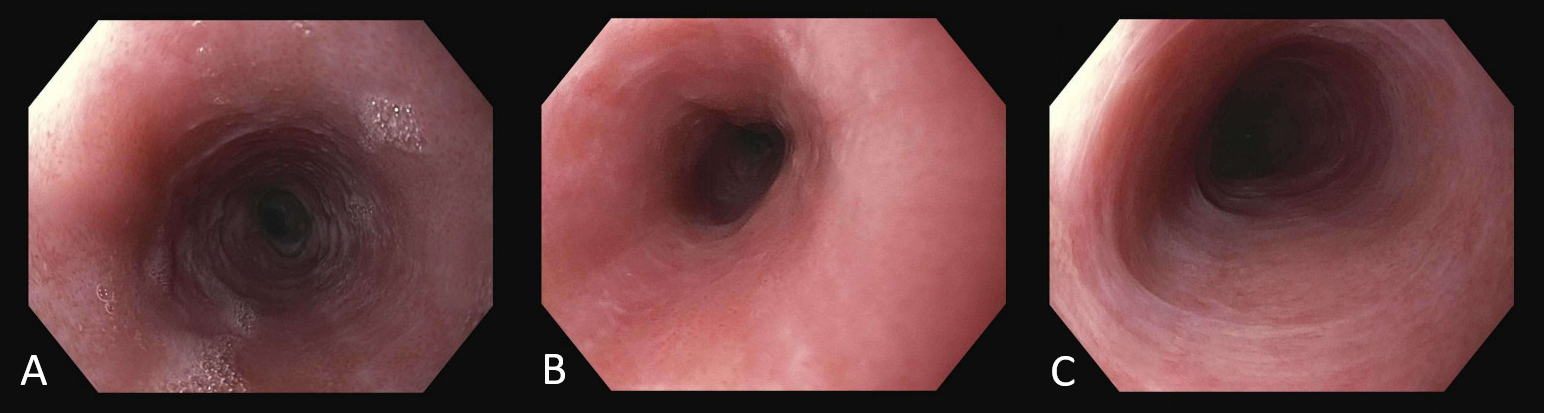
Figure: Endoscopic images of the esophagus from Esophagogastroduodenoscopy performed after discontinuation of rituximab therapy, showing improvement in ulcerations and inflammation.
A: Upper third of the esophagus – Improvement in ulceration and inflammation
B: Middle third of the esophagus – Improvement in ulceration and inflammation
C: Lower third of the esophagus – Improvement in ulceration and inflammation
Disclosures:
Muhammed Yaman Swied indicated no relevant financial relationships.
Obada Daaboul indicated no relevant financial relationships.
Muaataz Azzawi indicated no relevant financial relationships.
Abdul Swied indicated no relevant financial relationships.
Muhammed Yaman Swied, MBBS, Obada Daaboul, MD, Muaataz Azzawi, MD, Abdul Swied, MD. P5008 - Rituximab-Induced Esophageal Ulcers and Strictures Presenting as Dysphagia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

