Tuesday Poster Session
Category: Esophagus
P5007 - Spontaneous Eosinophilic Esophagitis (EoE) Perforation: A Rare Presentation
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Rutwik Pradeep Sharma, MD (he/him/his)
University of Michigan-Sparrow Hospital
Lansing, MI
Presenting Author(s)
Rutwik Pradeep. Sharma, MD1, Maitri Shah, MD2, Mythili Menon Pathiyil, MD3, Abhishek Satishchandran, MD, PhD4
1University of Michigan-Sparrow Hospital, Lansing, MI; 2University of Michigan Health - Sparrow, Lansing, MI; 3Saint Vincent Hospital, Worcester, MA; 4University of Michigan-Sparrow Hospital, Ann Arbor, MI
Introduction: EoE is an immune-mediated disease that causes esophageal dysfunction. We present a case of a spontaneous esophageal perforation in a 24-year-old male who was subsequently diagnosed with EoE.
Case Description/
Methods: A 24-year-old male presented to our hospital with complaints of chest pain and odynophagia for one week. The patient reported chronic solid food dysphagia but no recent history of food impaction or vomiting. He had intermittently been taking pantoprazole, sucralfate, and viscous lidocaine without much improvement. His exam and vitals were unremarkable. His computerized tomography (CT) angiogram revealed a 4 cm contained fluid pocket within the mid-esophageal wall. A subsequent gastrografin esophagram demonstrated a contained leak in the mid-esophagus (Image 1). The differential diagnosis was a ruptured duplication cyst versus a contained perforation. Following a multidisciplinary evaluation, he was kept nil by mouth (NPO) and started on intravenous(IV) antibiotics. The patient continued to report odynophagia. He underwent a diagnostic upper endoscopy with fluoroscopy, which revealed a narrow esophageal lumen that could only be traversed with a neonatal XP gastroscope. The endoscopic findings included longitudinal furrows, edema, diffuse exudate, and strictures suggestive of EoE (Image 2). A deep ulceration with a sinus tract was identified at 30 cm from the incisors. The esophageal biopsies revealed up to 100 eosinophils per high-power field. Stent placement, endovac therapy, and primary closure were considered. However, given the duration of the perforation ( >7 days) and clinical stability, the decision was made to maintain a strict NPO diet, total parenteral nutrition (TPN), IV pantoprazole 40 mg twice daily, IV antibiotics, and initiate IM Dupilumab 300 mg once weekly. Steroids were avoided in the setting of a perforation. A CT chest and esophagram, performed 2 weeks later, showed complete resolution of the cavity and no residual leak. The patient clinically improved, and a repeat endoscopy revealed no residual perforation, accompanied by a reduction of EoE features.
Discussion: According to our literature review, spontaneous perforation is an infrequent presenting scenario in undiagnosed EoE, as they are typically associated with food impaction-related necrosis or Boerhaave Syndrome. Neither were present here. We wish to highlight this rare presentation of EoE and successful management using conservative measures in a condition known to have high morbidity and mortality.
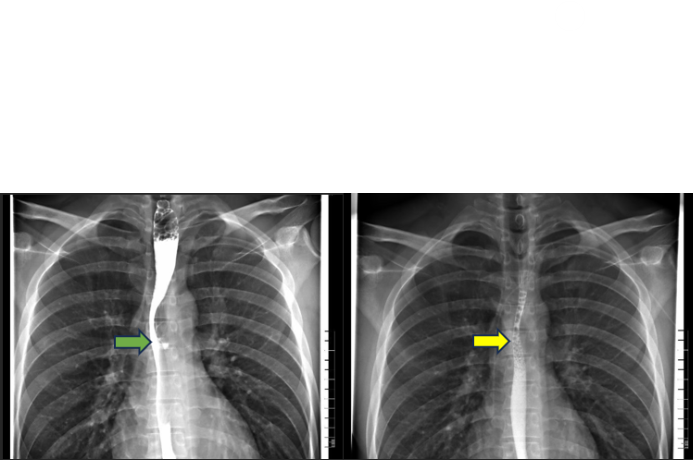
Figure: Image 1 (a)Green Arrow- Esophogram showing contained perforation
(b)Yellow Arrow- Esophogram showing no extravasation of the contrast
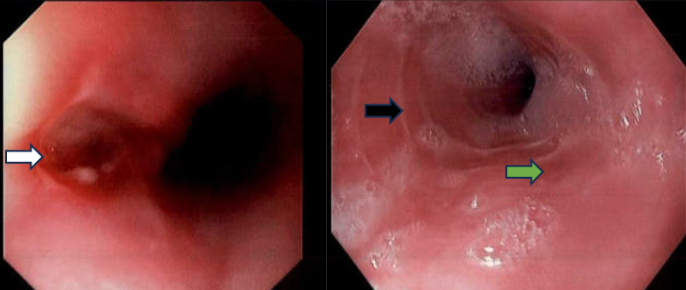
Figure: Image 2 (a) White arrow- Spontaneous perforation leading to a sinus tract
(b)Black arrow- Concentric rings and strictures
(c)Green arrow- Longitudinal furrows
The total EoE endoscopic reference score (EREFS) of 8.
Disclosures:
Rutwik Sharma indicated no relevant financial relationships.
Maitri Shah indicated no relevant financial relationships.
Mythili Menon Pathiyil indicated no relevant financial relationships.
Abhishek Satishchandran indicated no relevant financial relationships.
Rutwik Pradeep. Sharma, MD1, Maitri Shah, MD2, Mythili Menon Pathiyil, MD3, Abhishek Satishchandran, MD, PhD4. P5007 - Spontaneous Eosinophilic Esophagitis (EoE) Perforation: A Rare Presentation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Michigan-Sparrow Hospital, Lansing, MI; 2University of Michigan Health - Sparrow, Lansing, MI; 3Saint Vincent Hospital, Worcester, MA; 4University of Michigan-Sparrow Hospital, Ann Arbor, MI
Introduction: EoE is an immune-mediated disease that causes esophageal dysfunction. We present a case of a spontaneous esophageal perforation in a 24-year-old male who was subsequently diagnosed with EoE.
Case Description/
Methods: A 24-year-old male presented to our hospital with complaints of chest pain and odynophagia for one week. The patient reported chronic solid food dysphagia but no recent history of food impaction or vomiting. He had intermittently been taking pantoprazole, sucralfate, and viscous lidocaine without much improvement. His exam and vitals were unremarkable. His computerized tomography (CT) angiogram revealed a 4 cm contained fluid pocket within the mid-esophageal wall. A subsequent gastrografin esophagram demonstrated a contained leak in the mid-esophagus (Image 1). The differential diagnosis was a ruptured duplication cyst versus a contained perforation. Following a multidisciplinary evaluation, he was kept nil by mouth (NPO) and started on intravenous(IV) antibiotics. The patient continued to report odynophagia. He underwent a diagnostic upper endoscopy with fluoroscopy, which revealed a narrow esophageal lumen that could only be traversed with a neonatal XP gastroscope. The endoscopic findings included longitudinal furrows, edema, diffuse exudate, and strictures suggestive of EoE (Image 2). A deep ulceration with a sinus tract was identified at 30 cm from the incisors. The esophageal biopsies revealed up to 100 eosinophils per high-power field. Stent placement, endovac therapy, and primary closure were considered. However, given the duration of the perforation ( >7 days) and clinical stability, the decision was made to maintain a strict NPO diet, total parenteral nutrition (TPN), IV pantoprazole 40 mg twice daily, IV antibiotics, and initiate IM Dupilumab 300 mg once weekly. Steroids were avoided in the setting of a perforation. A CT chest and esophagram, performed 2 weeks later, showed complete resolution of the cavity and no residual leak. The patient clinically improved, and a repeat endoscopy revealed no residual perforation, accompanied by a reduction of EoE features.
Discussion: According to our literature review, spontaneous perforation is an infrequent presenting scenario in undiagnosed EoE, as they are typically associated with food impaction-related necrosis or Boerhaave Syndrome. Neither were present here. We wish to highlight this rare presentation of EoE and successful management using conservative measures in a condition known to have high morbidity and mortality.
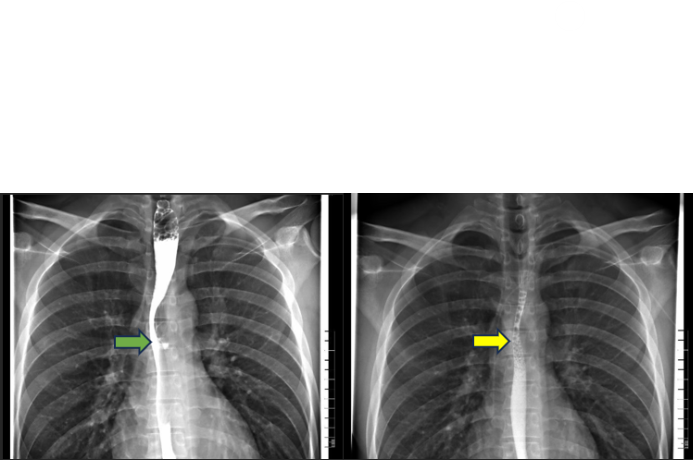
Figure: Image 1 (a)Green Arrow- Esophogram showing contained perforation
(b)Yellow Arrow- Esophogram showing no extravasation of the contrast
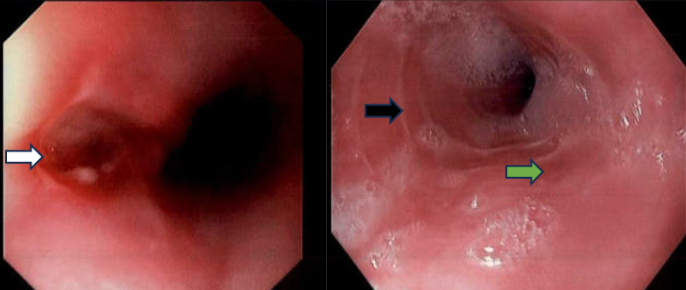
Figure: Image 2 (a) White arrow- Spontaneous perforation leading to a sinus tract
(b)Black arrow- Concentric rings and strictures
(c)Green arrow- Longitudinal furrows
The total EoE endoscopic reference score (EREFS) of 8.
Disclosures:
Rutwik Sharma indicated no relevant financial relationships.
Maitri Shah indicated no relevant financial relationships.
Mythili Menon Pathiyil indicated no relevant financial relationships.
Abhishek Satishchandran indicated no relevant financial relationships.
Rutwik Pradeep. Sharma, MD1, Maitri Shah, MD2, Mythili Menon Pathiyil, MD3, Abhishek Satishchandran, MD, PhD4. P5007 - Spontaneous Eosinophilic Esophagitis (EoE) Perforation: A Rare Presentation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

