Tuesday Poster Session
Category: Esophagus
P5001 - Pseudoachalasia in an Achalasia Patient: A Case of a Ticking Time Bomb
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Hannah WF Fiske, MD (she/her/hers)
Yale Digestive Diseases
New Haven, CT
Presenting Author(s)
Hannah WF. Goodrich, MD1, Thiruvengadam Muniraj, MD2, Amir Masoud, MD3
1Yale Digestive Diseases, New Haven, CT; 2Yale University School of Medicine, New Haven, CT; 3Hartford Healthcare/Connecticut GI, Fairfield, CT
Introduction: The differential for dysphagia is broad, with dysphagia aortica being an incredibly rare cause of pseudoachalasia. In a patient with longstanding, refractory achalasia who presents with progressive dysphagia, Occam’s Razor would suggest that the underlying cause remains achalasia itself. We present a case in which a patient with known achalasia developed concurrent pseudoachalasia due to dysphagia aortica. This case underscores the diligence of her gastroenterologist in identifying an unsuspected aortic aneurysm – an entity that the cardiothoracic surgery team deemed “a ticking time bomb.”
Case Description/
Methods: Our patient is a 31-year-old female with history of type II achalasia, having undergone two laparoscopic Heller myotomies (with Dor fundoplication ultimately replacing the original Toupet) and a Peroral Endoscopic Myotomy (POEM). Following her successful POEM, she had 4 years of symptom control before experiencing progressive dysphagia.
Esophagogastroduodenoscopy (EGD) revealed mid-esophageal tortuosity (Fig 1a), concerning for either extrinsic compression or evolving post-surgical changes in the setting of achalasia. EUS showed a thin open lower esophageal sphincter (LES), a loose fundoplication (Fig 1b), and a markedly dilated vascular structure in the mid-thoracic esophagus, exerting a clear mass effect (Fig 1c).
A gated CT angiogram confirmed a large saccular aneurysm arising from the posterior medial aortic arch. The aneurysmal sac measured 4.6x4.2x2.5cm and caused significant compression of the esophagus (Fig 2).
Given the aneurysm’s size and saccular nature, cardiothoracic surgery expedited intervention within two weeks of diagnosis. She underwent a successful open thoracoabdominal aortic aneurysm repair. Further testing revealed underlying connective tissue disease as the likely etiology.
Discussion: This case illustrates a rare instance of pseudoachalasia secondary to vascular compression from an aortic aneurysm in a patient with established primary achalasia. While the differential for dysphagia is broad, in patients with a history of refractory achalasia, it can be tempting to attribute symptoms to the primary diagnosis itself. This case highlights the importance of Hickam’s Dictum, reminding us that patients may have multiple coexisting diseases simultaneously. In this case, the gastroenterologist’s careful attention to alternate possibilities and thorough workup uncovered the true etiology of the patient’s symptoms, ultimately saving her life.
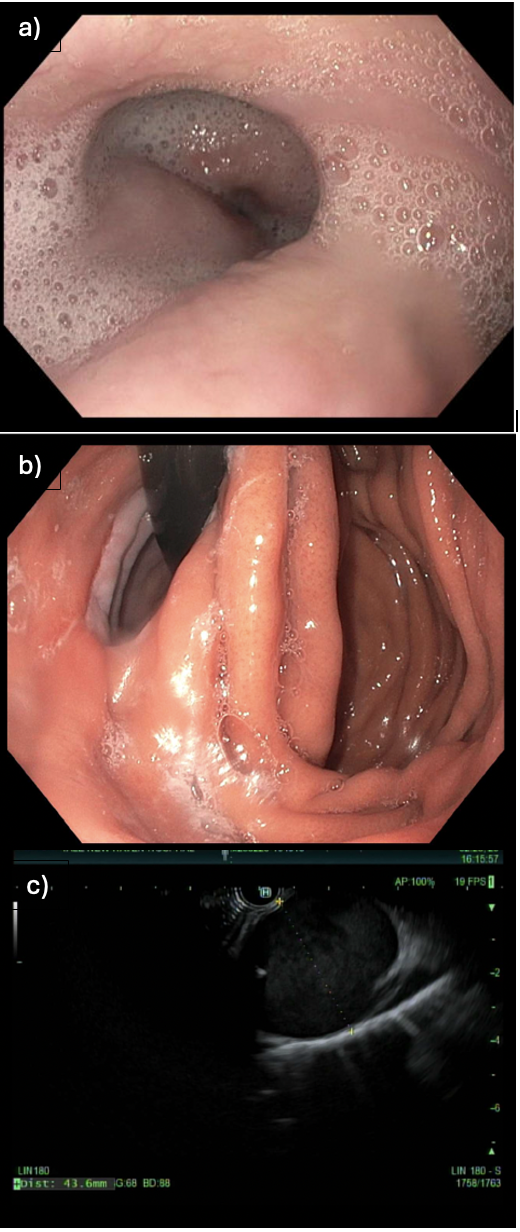
Figure: Figure 1: Images from the endoscopic ultrasound
(a) Mid-esophageal tortuosity, concerning for extrinsic compression.
(b) Fundoplication from previous Heller myotomy, confirmed to be loose and not the cause of the patient’s dysphagia.
(c) Thoracic large saccular dilated vessel, later determined to be the aorta.
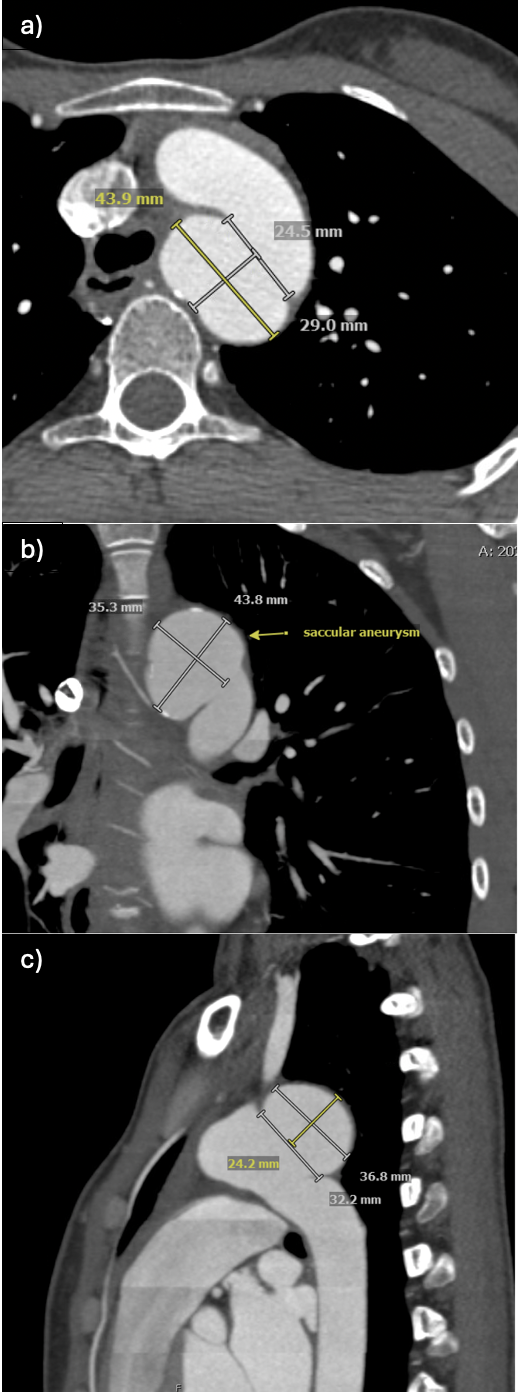
Figure: Figure 2: Images from the gated CT scan, revealing a large saccular aneurysm causing compression on the esophagus.
Disclosures:
Hannah Goodrich indicated no relevant financial relationships.
Thiruvengadam Muniraj indicated no relevant financial relationships.
Amir Masoud indicated no relevant financial relationships.
Hannah WF. Goodrich, MD1, Thiruvengadam Muniraj, MD2, Amir Masoud, MD3. P5001 - Pseudoachalasia in an Achalasia Patient: A Case of a Ticking Time Bomb, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Yale Digestive Diseases, New Haven, CT; 2Yale University School of Medicine, New Haven, CT; 3Hartford Healthcare/Connecticut GI, Fairfield, CT
Introduction: The differential for dysphagia is broad, with dysphagia aortica being an incredibly rare cause of pseudoachalasia. In a patient with longstanding, refractory achalasia who presents with progressive dysphagia, Occam’s Razor would suggest that the underlying cause remains achalasia itself. We present a case in which a patient with known achalasia developed concurrent pseudoachalasia due to dysphagia aortica. This case underscores the diligence of her gastroenterologist in identifying an unsuspected aortic aneurysm – an entity that the cardiothoracic surgery team deemed “a ticking time bomb.”
Case Description/
Methods: Our patient is a 31-year-old female with history of type II achalasia, having undergone two laparoscopic Heller myotomies (with Dor fundoplication ultimately replacing the original Toupet) and a Peroral Endoscopic Myotomy (POEM). Following her successful POEM, she had 4 years of symptom control before experiencing progressive dysphagia.
Esophagogastroduodenoscopy (EGD) revealed mid-esophageal tortuosity (Fig 1a), concerning for either extrinsic compression or evolving post-surgical changes in the setting of achalasia. EUS showed a thin open lower esophageal sphincter (LES), a loose fundoplication (Fig 1b), and a markedly dilated vascular structure in the mid-thoracic esophagus, exerting a clear mass effect (Fig 1c).
A gated CT angiogram confirmed a large saccular aneurysm arising from the posterior medial aortic arch. The aneurysmal sac measured 4.6x4.2x2.5cm and caused significant compression of the esophagus (Fig 2).
Given the aneurysm’s size and saccular nature, cardiothoracic surgery expedited intervention within two weeks of diagnosis. She underwent a successful open thoracoabdominal aortic aneurysm repair. Further testing revealed underlying connective tissue disease as the likely etiology.
Discussion: This case illustrates a rare instance of pseudoachalasia secondary to vascular compression from an aortic aneurysm in a patient with established primary achalasia. While the differential for dysphagia is broad, in patients with a history of refractory achalasia, it can be tempting to attribute symptoms to the primary diagnosis itself. This case highlights the importance of Hickam’s Dictum, reminding us that patients may have multiple coexisting diseases simultaneously. In this case, the gastroenterologist’s careful attention to alternate possibilities and thorough workup uncovered the true etiology of the patient’s symptoms, ultimately saving her life.
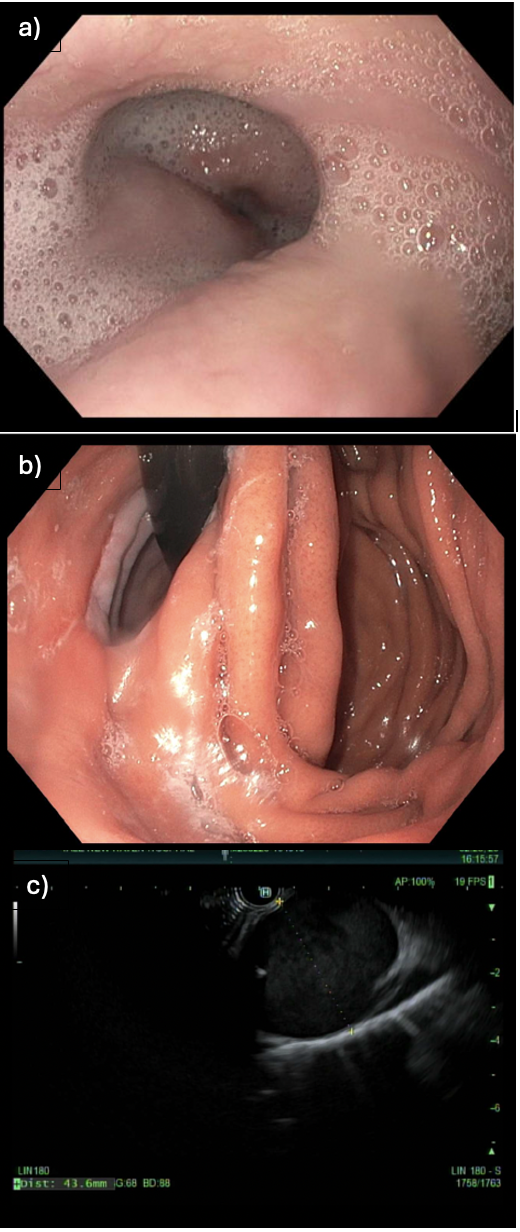
Figure: Figure 1: Images from the endoscopic ultrasound
(a) Mid-esophageal tortuosity, concerning for extrinsic compression.
(b) Fundoplication from previous Heller myotomy, confirmed to be loose and not the cause of the patient’s dysphagia.
(c) Thoracic large saccular dilated vessel, later determined to be the aorta.
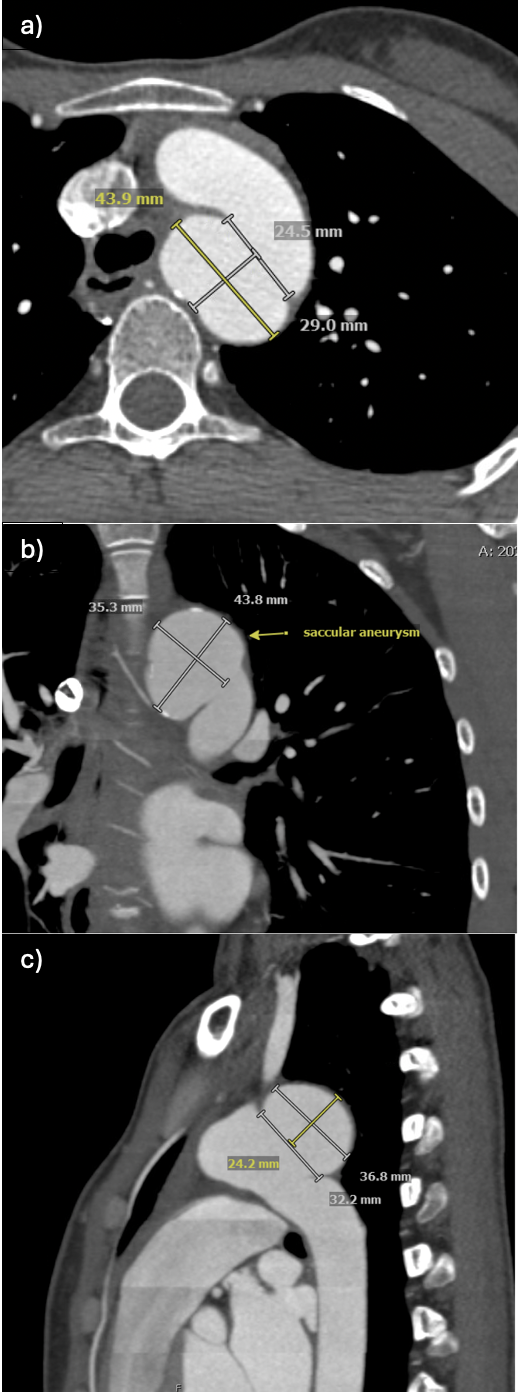
Figure: Figure 2: Images from the gated CT scan, revealing a large saccular aneurysm causing compression on the esophagus.
Disclosures:
Hannah Goodrich indicated no relevant financial relationships.
Thiruvengadam Muniraj indicated no relevant financial relationships.
Amir Masoud indicated no relevant financial relationships.
Hannah WF. Goodrich, MD1, Thiruvengadam Muniraj, MD2, Amir Masoud, MD3. P5001 - Pseudoachalasia in an Achalasia Patient: A Case of a Ticking Time Bomb, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
