Tuesday Poster Session
Category: Esophagus
P4996 - Unraveling Dermatomyositis: Severe Dysphagia and Cutaneous Findings in a 69-Year-Old Man
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mikayla Cunney (she/her/hers)
Virginia Commonwealth University School of Medicine and Richmond VA Medical Center
Richmond, VA
Presenting Author(s)
Mikayla Cunney, 1, Vinay Jahagirdar, MBBS2, Asiya Tafader, MD2, Cathy Massoud, MD3, Brian Davis, MD4
1Virginia Commonwealth University School of Medicine and Richmond VA Medical Center, Richmond, VA; 2Division of Gastroenterology, Hepatology and Nutrition, Virginia Commonwealth University Health System, Richmond, VA; 3Hunter Holmes McGuire VA Medical Center, Richmond, VA; 4Medical Director of Liver Transplantation, Hunter Holmes McGuire VA Medical Center, Richmond, VA
Introduction: Dermatomyositis is an idiopathic inflammatory myopathy characterized by proximal muscle weakness and pathognomonic skin findings. Dysphagia, which occurs in up to 40% of cases, can result from oropharyngeal muscle involvement and may present before muscle symptoms. We present a case of dermatomyositis with prominent cutaneous manifestations and severe dysphagia, emphasizing early recognition and immunosuppressive management.
Case Description/
Methods: A 69-year-old African American male initially presented to his primary care physician with a violaceous rash and mass on his left lower eyelid. A few days later, he developed a coalescing, pruritic rash on his chest, arms, and face, along with periungual erythema. A week after the rash presented, he reported progressive dysphagia to both solids and liquids, along with odynophagia and a 30-pound weight loss. Dermatology suspected dermatomyositis and performed a skin biopsy. He was admitted for worsening dysphagia and failure to thrive. Further workup revealed elevated creatine kinase (~800 U/L), LDH, AST, and positive TIF-1γ antibodies. Despite equivocal proximal muscle weakness, his rash, lymphadenopathy, cytopenias, and dysphagia supported the diagnosis of dermatomyositis. CT imaging showed cervical and axillary lymphadenopathy; however biopsy was negative for malignancy. His EGD was unremarkable, but a modified barium swallow demonstrated severe oropharyngeal dysphagia with aspiration. The inpatient GI team was consulted for possible PEG tube placement. However, it was decided to start therapy for dermatomyositis, and monitor if dysphagia improved.
He was treated with IVIG, high-dose corticosteroids, and mycophenolate mofetil. His swallowing function improved significantly by day 2 of therapy and although not fully back to baseline, he resumed eating without aspiration events.
Discussion: Dysphagia in dermatomyositis is frequently due to cricopharyngeal and oropharyngeal muscle dysfunction and may precede or occur in the absence of overt muscle weakness. The patient’s TIF-1γ positivity, associated with increased malignancy risk, warranted thorough malignancy screening. This case demonstrates the need to consider dermatomyositis in patients presenting with rapidly progressive dysphagia and cutaneous findings, even in the absence of clear muscle weakness. It may be prudent to monitor for improvement of dysphagia symptoms with immunosuppressive therapy, rather than rush to enteral feeding via PEG in such cases.
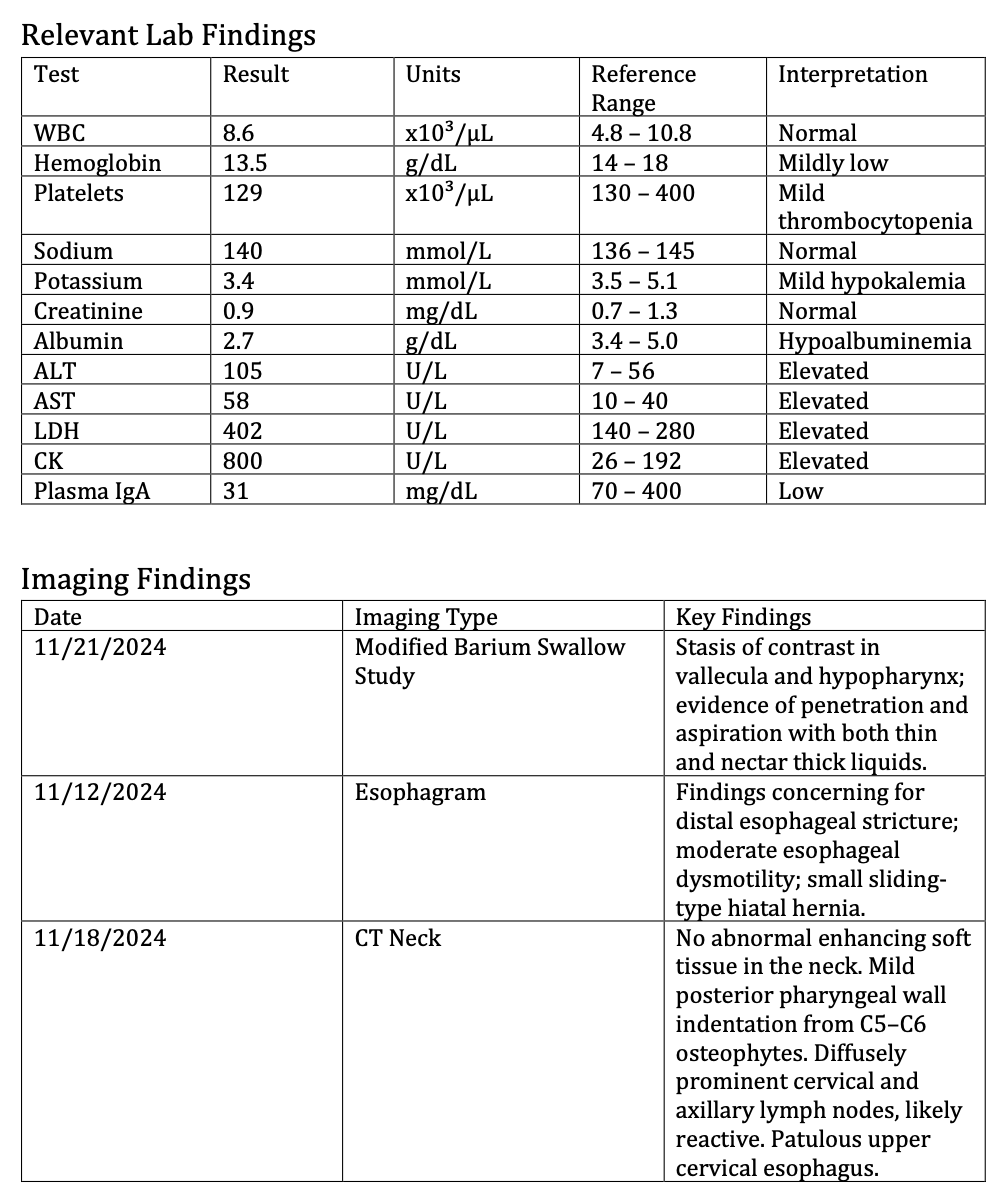
Figure: Table: Key Laboratory Findings
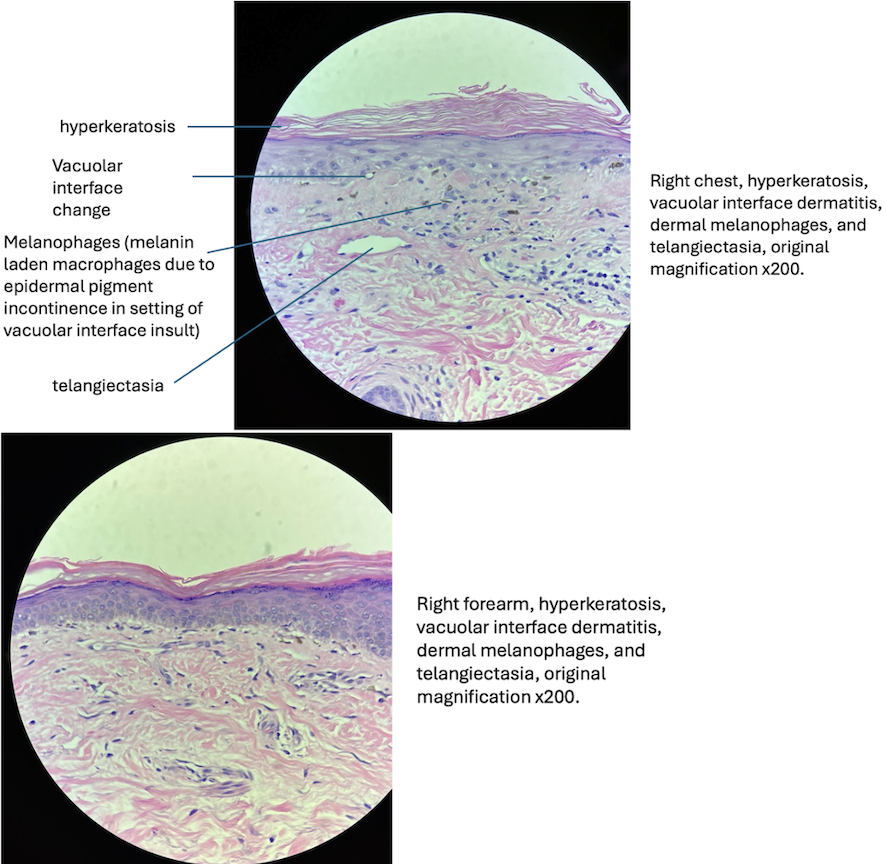
Figure: Figure: Histopathologic Features Consistent with Dermatomyositis
Disclosures:
Mikayla Cunney indicated no relevant financial relationships.
Vinay Jahagirdar indicated no relevant financial relationships.
Asiya Tafader indicated no relevant financial relationships.
Cathy Massoud indicated no relevant financial relationships.
Brian Davis indicated no relevant financial relationships.
Mikayla Cunney, 1, Vinay Jahagirdar, MBBS2, Asiya Tafader, MD2, Cathy Massoud, MD3, Brian Davis, MD4. P4996 - Unraveling Dermatomyositis: Severe Dysphagia and Cutaneous Findings in a 69-Year-Old Man, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Virginia Commonwealth University School of Medicine and Richmond VA Medical Center, Richmond, VA; 2Division of Gastroenterology, Hepatology and Nutrition, Virginia Commonwealth University Health System, Richmond, VA; 3Hunter Holmes McGuire VA Medical Center, Richmond, VA; 4Medical Director of Liver Transplantation, Hunter Holmes McGuire VA Medical Center, Richmond, VA
Introduction: Dermatomyositis is an idiopathic inflammatory myopathy characterized by proximal muscle weakness and pathognomonic skin findings. Dysphagia, which occurs in up to 40% of cases, can result from oropharyngeal muscle involvement and may present before muscle symptoms. We present a case of dermatomyositis with prominent cutaneous manifestations and severe dysphagia, emphasizing early recognition and immunosuppressive management.
Case Description/
Methods: A 69-year-old African American male initially presented to his primary care physician with a violaceous rash and mass on his left lower eyelid. A few days later, he developed a coalescing, pruritic rash on his chest, arms, and face, along with periungual erythema. A week after the rash presented, he reported progressive dysphagia to both solids and liquids, along with odynophagia and a 30-pound weight loss. Dermatology suspected dermatomyositis and performed a skin biopsy. He was admitted for worsening dysphagia and failure to thrive. Further workup revealed elevated creatine kinase (~800 U/L), LDH, AST, and positive TIF-1γ antibodies. Despite equivocal proximal muscle weakness, his rash, lymphadenopathy, cytopenias, and dysphagia supported the diagnosis of dermatomyositis. CT imaging showed cervical and axillary lymphadenopathy; however biopsy was negative for malignancy. His EGD was unremarkable, but a modified barium swallow demonstrated severe oropharyngeal dysphagia with aspiration. The inpatient GI team was consulted for possible PEG tube placement. However, it was decided to start therapy for dermatomyositis, and monitor if dysphagia improved.
He was treated with IVIG, high-dose corticosteroids, and mycophenolate mofetil. His swallowing function improved significantly by day 2 of therapy and although not fully back to baseline, he resumed eating without aspiration events.
Discussion: Dysphagia in dermatomyositis is frequently due to cricopharyngeal and oropharyngeal muscle dysfunction and may precede or occur in the absence of overt muscle weakness. The patient’s TIF-1γ positivity, associated with increased malignancy risk, warranted thorough malignancy screening. This case demonstrates the need to consider dermatomyositis in patients presenting with rapidly progressive dysphagia and cutaneous findings, even in the absence of clear muscle weakness. It may be prudent to monitor for improvement of dysphagia symptoms with immunosuppressive therapy, rather than rush to enteral feeding via PEG in such cases.
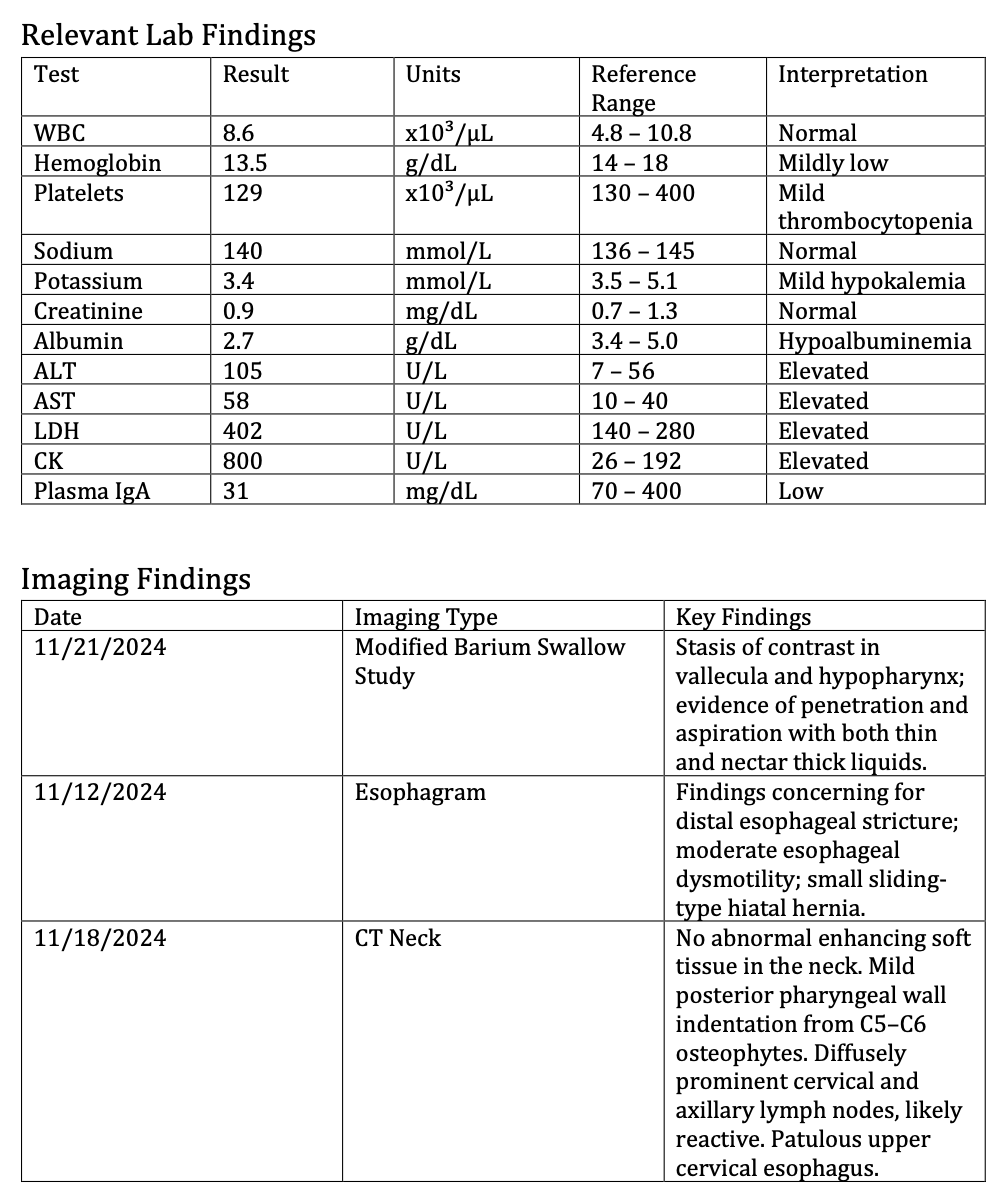
Figure: Table: Key Laboratory Findings
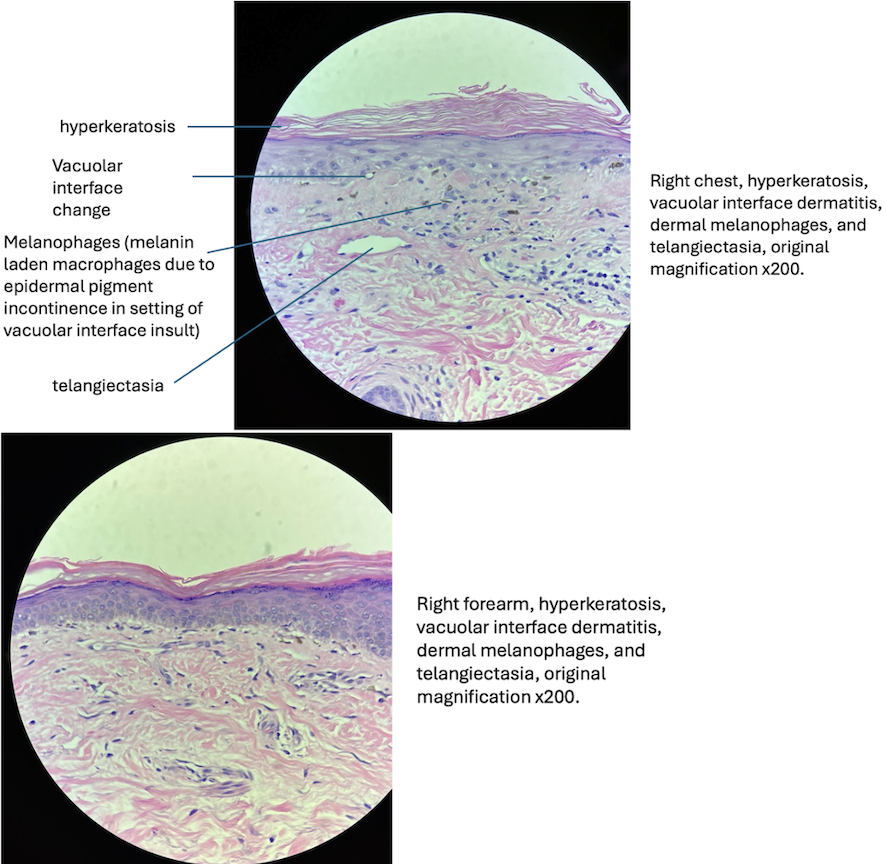
Figure: Figure: Histopathologic Features Consistent with Dermatomyositis
Disclosures:
Mikayla Cunney indicated no relevant financial relationships.
Vinay Jahagirdar indicated no relevant financial relationships.
Asiya Tafader indicated no relevant financial relationships.
Cathy Massoud indicated no relevant financial relationships.
Brian Davis indicated no relevant financial relationships.
Mikayla Cunney, 1, Vinay Jahagirdar, MBBS2, Asiya Tafader, MD2, Cathy Massoud, MD3, Brian Davis, MD4. P4996 - Unraveling Dermatomyositis: Severe Dysphagia and Cutaneous Findings in a 69-Year-Old Man, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

