Tuesday Poster Session
Category: Esophagus
P4990 - The Long Road to a Rare Diagnosis: Dysphagia Lusoria Post-Roux-en-Y Gastric Bypass
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Melvin Joy, MD (he/him/his)
HCA Healthcare Citrus Hospital
Inverness, FL
Presenting Author(s)
Melvin Joy, MD1, Nathaniel J. Leavitt, DO2, Pujan Kandel, MD2, Siddharth Mathur, MD3
1HCA Healthcare Citrus Hospital, Inverness, FL; 2HCA Florida Healthcare, Inverness, FL; 3HCA Florida Citrus Hospital, Inverness, FL
Introduction: Dysphagia lusoria is an uncommon vascular anomaly in which an aberrant right subclavian artery (ARSA) compresses the esophagus. Diagnosis is often delayed as the dysphagia is misattributed to more common conditions, particularly in patients with altered foregut anatomy. In this report, we describe a case illustrating the clinical significance and diagnostic challenge of dysphagia lusoria in a post-Roux-en-Y gastric bypass (RYGB) patient.
Case Description/
Methods: A 70-year-old woman with a history of RYGB, with Billroth II anatomy, and hiatal hernia repair developed progressive solid-food dysphagia beginning in her late 50s. Endoscopic evaluation was unrevealing, and though BRAVO pH testing did show severe acid reflux, only minimal relief was provided by antireflux therapy. Further endoscopies identified a benign-appearing gastroesophageal junction (GEJ) anastomotic stricture and over the next 11 years she underwent a total of 14 EGDs with 12 dilations, which provided only transient relief. Her dysphagia slowly progressed, ultimately with daily symptoms, occasional dysphagia of liquids, and a 20-pound weight loss. Evaluation with barium esophagram and high-resolution manometry were otherwise non-diagnostic and no definitive etiology was identified. A contrast-enhanced CT of the neck and chest was eventually obtained and revealed an ARSA traveling posterior to the esophagus with compression against the trachea anteriorly, which confirmed the diagnosis of dysphagia lusoria.
Discussion: This case underscores how coexisting pathologies can lead to anchoring bias and delay recognition of a rare etiology with a post-surgical GEJ stricture obscuring the much less common diagnosis of dysphagia lusoria. The turning point of this extended diagnostic odyssey came with cross-sectional imaging, definitively identifying the ARSA after nearly 11 years of inconclusive workup and only transient symptom relief. Retrospectively, new or persistent dysphagia after foregut surgery should prompt evaluation with contrast enhanced CT of the neck and chest. Had that diagnostic pathway been adopted earlier, the patient might have been spared numerous endoscopies and dilations. This case highlights the importance of maintaining a broad differential of diagnoses for refractory dysphagia, including rare vascular anomalies and pursuing definitive imaging when symptoms persist despite negative endoscopic and motility workups.
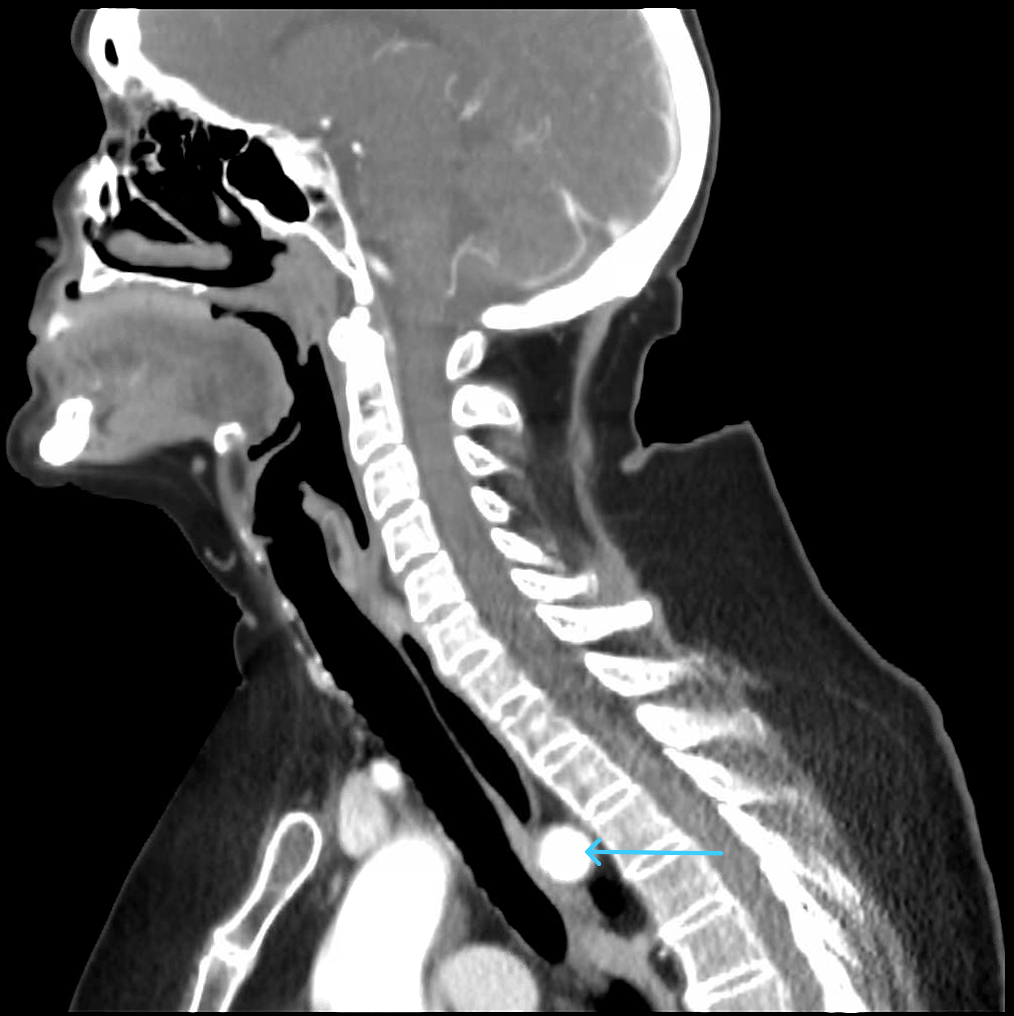
Figure: Sagittal CT image showing the aberrant right subclavian artery (blue arrow) traversing behind the esophagus.
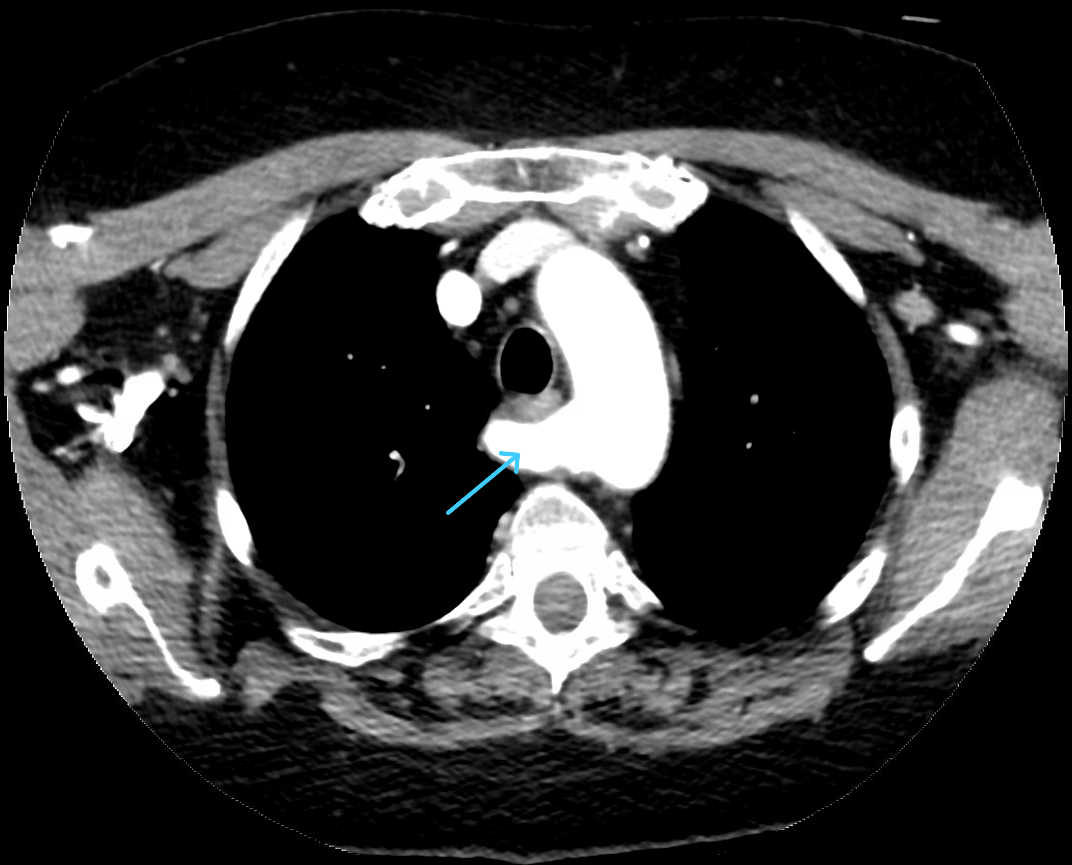
Figure: Axial CT scan (mediastinal window) at the level of the aortic arch, showing the aberrant right subclavian artery posterior to the esophagus (blue arrow).
Disclosures:
Melvin Joy indicated no relevant financial relationships.
Nathaniel Leavitt indicated no relevant financial relationships.
Pujan Kandel indicated no relevant financial relationships.
Siddharth Mathur indicated no relevant financial relationships.
Melvin Joy, MD1, Nathaniel J. Leavitt, DO2, Pujan Kandel, MD2, Siddharth Mathur, MD3. P4990 - The Long Road to a Rare Diagnosis: Dysphagia Lusoria Post-Roux-en-Y Gastric Bypass, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1HCA Healthcare Citrus Hospital, Inverness, FL; 2HCA Florida Healthcare, Inverness, FL; 3HCA Florida Citrus Hospital, Inverness, FL
Introduction: Dysphagia lusoria is an uncommon vascular anomaly in which an aberrant right subclavian artery (ARSA) compresses the esophagus. Diagnosis is often delayed as the dysphagia is misattributed to more common conditions, particularly in patients with altered foregut anatomy. In this report, we describe a case illustrating the clinical significance and diagnostic challenge of dysphagia lusoria in a post-Roux-en-Y gastric bypass (RYGB) patient.
Case Description/
Methods: A 70-year-old woman with a history of RYGB, with Billroth II anatomy, and hiatal hernia repair developed progressive solid-food dysphagia beginning in her late 50s. Endoscopic evaluation was unrevealing, and though BRAVO pH testing did show severe acid reflux, only minimal relief was provided by antireflux therapy. Further endoscopies identified a benign-appearing gastroesophageal junction (GEJ) anastomotic stricture and over the next 11 years she underwent a total of 14 EGDs with 12 dilations, which provided only transient relief. Her dysphagia slowly progressed, ultimately with daily symptoms, occasional dysphagia of liquids, and a 20-pound weight loss. Evaluation with barium esophagram and high-resolution manometry were otherwise non-diagnostic and no definitive etiology was identified. A contrast-enhanced CT of the neck and chest was eventually obtained and revealed an ARSA traveling posterior to the esophagus with compression against the trachea anteriorly, which confirmed the diagnosis of dysphagia lusoria.
Discussion: This case underscores how coexisting pathologies can lead to anchoring bias and delay recognition of a rare etiology with a post-surgical GEJ stricture obscuring the much less common diagnosis of dysphagia lusoria. The turning point of this extended diagnostic odyssey came with cross-sectional imaging, definitively identifying the ARSA after nearly 11 years of inconclusive workup and only transient symptom relief. Retrospectively, new or persistent dysphagia after foregut surgery should prompt evaluation with contrast enhanced CT of the neck and chest. Had that diagnostic pathway been adopted earlier, the patient might have been spared numerous endoscopies and dilations. This case highlights the importance of maintaining a broad differential of diagnoses for refractory dysphagia, including rare vascular anomalies and pursuing definitive imaging when symptoms persist despite negative endoscopic and motility workups.
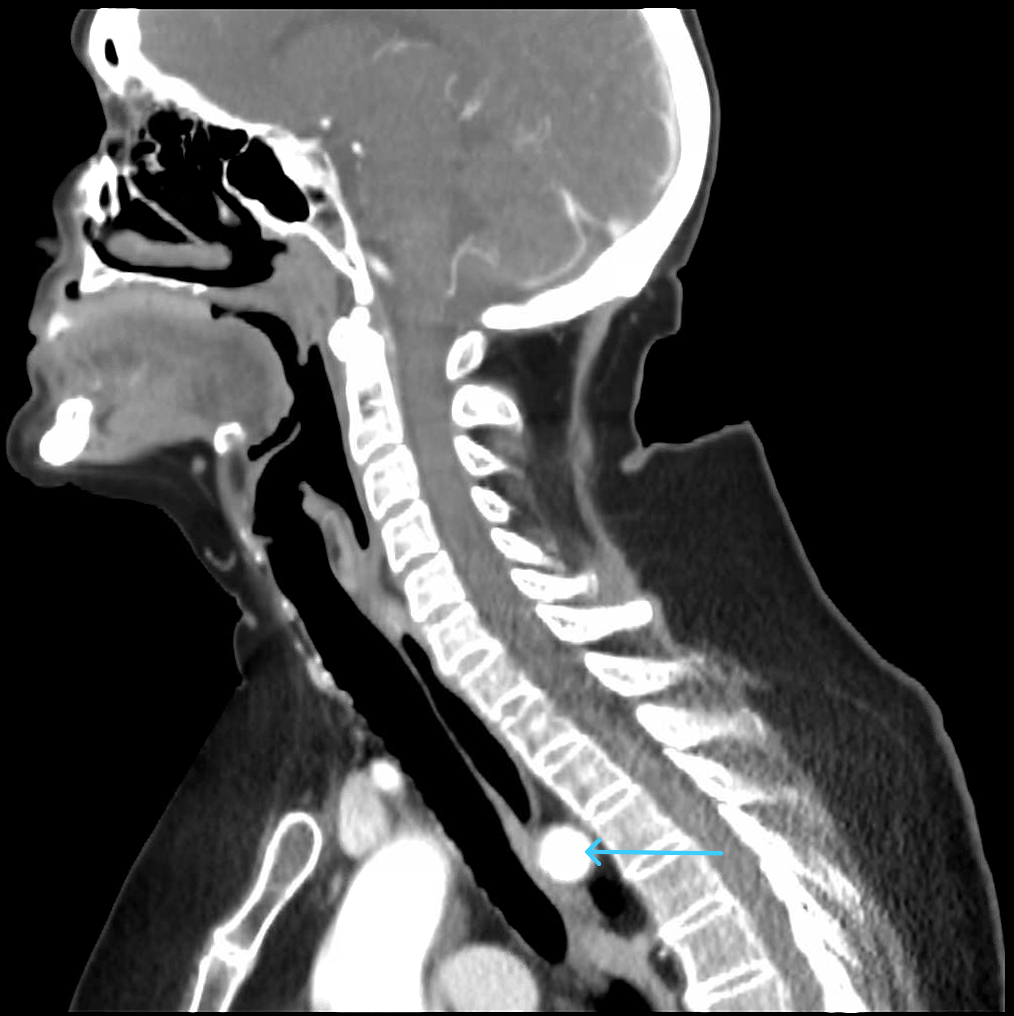
Figure: Sagittal CT image showing the aberrant right subclavian artery (blue arrow) traversing behind the esophagus.
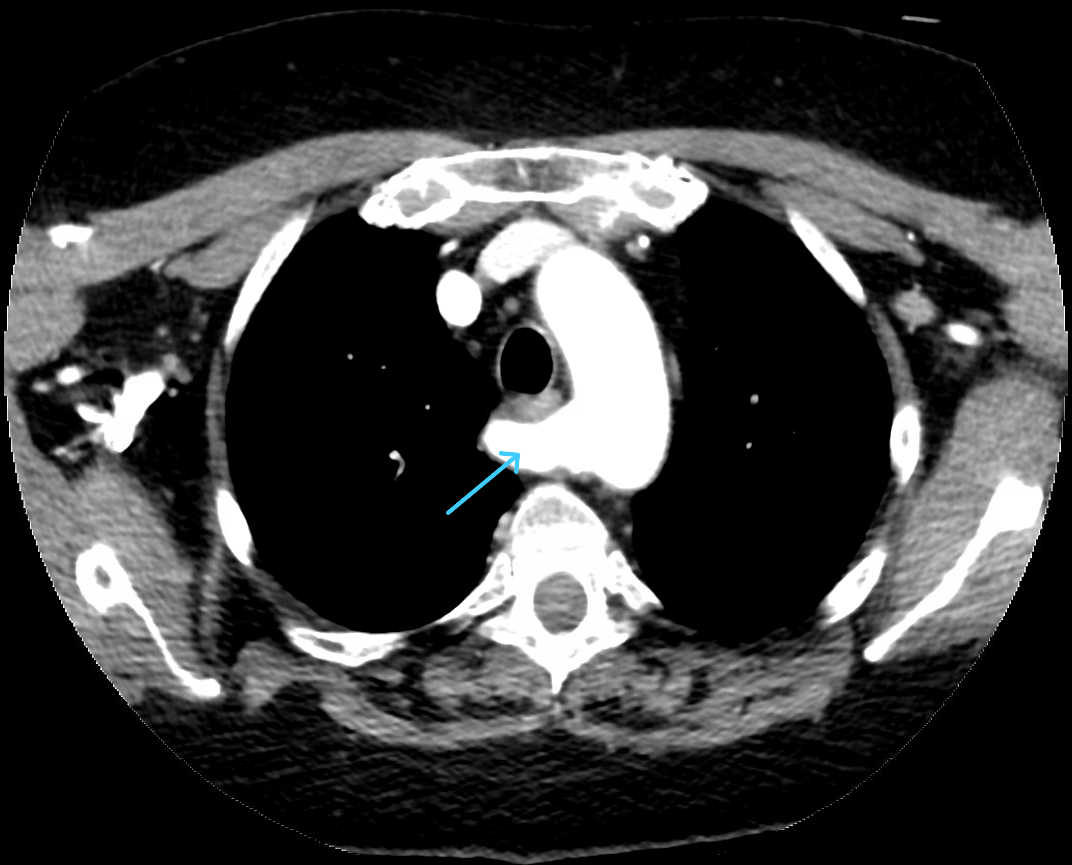
Figure: Axial CT scan (mediastinal window) at the level of the aortic arch, showing the aberrant right subclavian artery posterior to the esophagus (blue arrow).
Disclosures:
Melvin Joy indicated no relevant financial relationships.
Nathaniel Leavitt indicated no relevant financial relationships.
Pujan Kandel indicated no relevant financial relationships.
Siddharth Mathur indicated no relevant financial relationships.
Melvin Joy, MD1, Nathaniel J. Leavitt, DO2, Pujan Kandel, MD2, Siddharth Mathur, MD3. P4990 - The Long Road to a Rare Diagnosis: Dysphagia Lusoria Post-Roux-en-Y Gastric Bypass, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
