Tuesday Poster Session
Category: Esophagus
P4971 - The Perfect Storm: Lymphocytic Esophagitis in an HIV-Positive Patient
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Jake Cresta, MD (he/him/his)
Walter Reed National Military Medical Center
Bethesda, MD
Presenting Author(s)
Jake Cresta, MD, Roy Wong, MD, Robert Spiller, DO, MS
Walter Reed National Military Medical Center, Bethesda, MD
Introduction: Lymphocytic esophagitis (LyE) is a rare inflammatory disorder of the esophagus, first described in 2006, characterized by increased intraepithelial lymphocytes. It is associated with immune-mediated conditions and chronic esophageal irritation. Clinically and endoscopically, LyE mimics eosinophilic esophagitis (EoE) and has been linked to autoimmune diseases and immunodeficiencies. Due to its rarity, treatment is empiric and often includes proton pump inhibitors (PPIs) and topical corticosteroids.
Case Description/
Methods: A 46-year-old female with well-controlled HIV and a history of recurrent esophageal candidiasis complicated by strictures and Schatzki rings presented with progressive dysphagia. Despite prior fluconazole therapy, periodic dilations, and long-term PPI use, she experienced worsening symptoms after self-discontinuing omeprazole. Esophagogastroduodenoscopy revealed a persistent stricture, dilated with an 52F Maloney dilator. Biopsies from the mid-esophagus demonstrated marked intraepithelial lymphocytosis and benign squamous epithelium with spongiosis, but no eosinophils or fungal elements, consistent with LyE. The patient was restarted on omeprazole 40 mg daily and swallowed fluticasone, leading to significant symptom improvement.
Discussion: This case underscores LyE as an underrecognized esophageal condition, particularly in immunocompromised individuals. Though often associated with autoimmune disorders, its relationship with chronic infections like HIV and Candida esophagitis is poorly understood. While Candida can also cause intraepithelial lymphocytosis, the absence of fungal elements on biopsy excluded this etiology. LyE and EoE share overlapping features, including dysphagia and esophageal webs, though LyE is less often associated with food impaction. Histologic findings in LyE include peripapillary lymphocytosis, spongiosis, and absence of eosinophils or pathogens. Diagnosis is generally based on intraepithelial lymphocyte counts >20 per high-power field (normal: 3-10). Management includes PPIs, swallowed corticosteroids, and endoscopic dilation. Mucosal corticosteroid injections may also reduce inflammation and fibrosis. This case illustrates the complex interplay of immune dysfunction, chronic infection, and esophageal irritation in the pathogenesis of LyE. It highlights the need for heightened clinical awareness and further research to define standardized diagnostic and treatment approaches for this emerging condition.
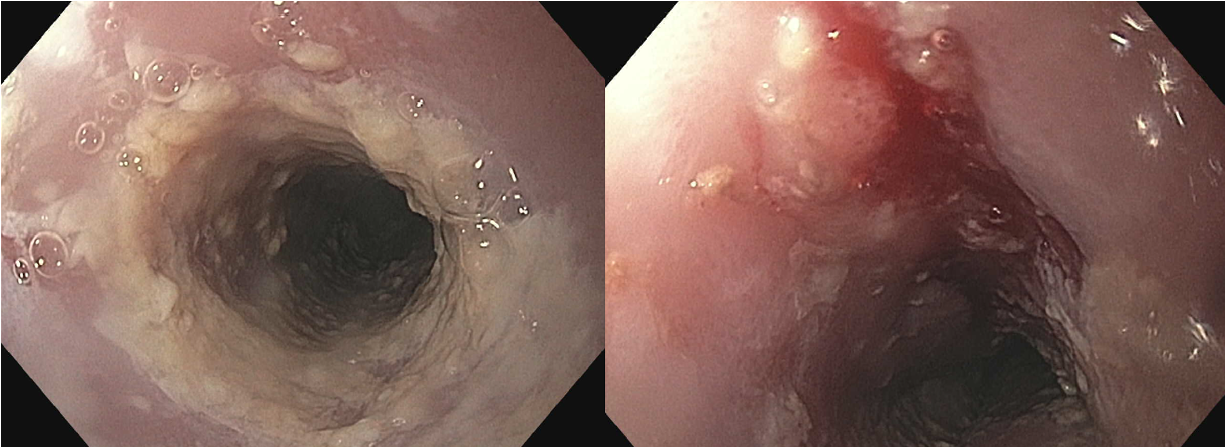
Figure: Figure 1 - Endoscopic images from several years earlier: Left panel demonstrates the proximal esophagus with short, friable stricture at 22cm from incisors which was intervally dilated with Maloney 28F and 32F. Dilation effect visualized on the right panel.
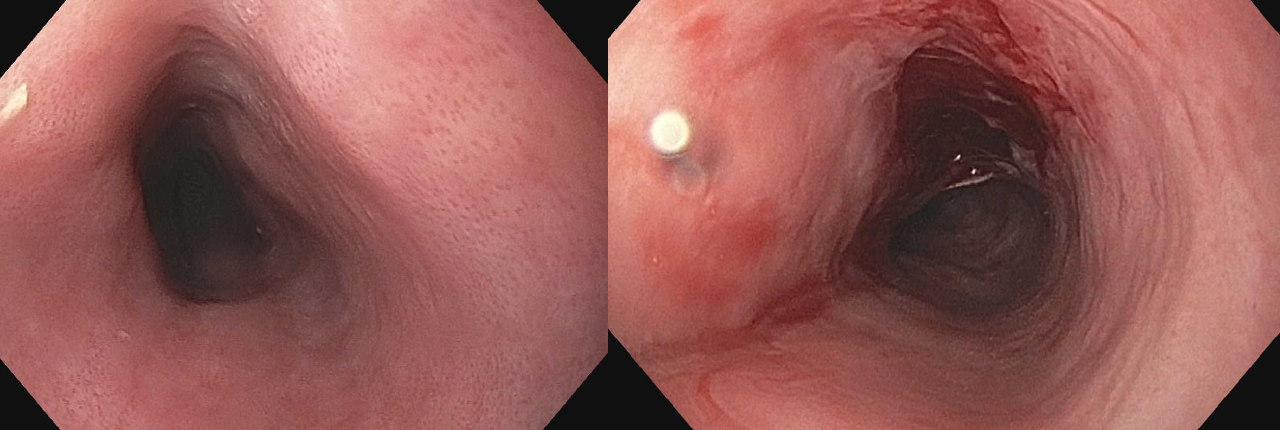
Figure: Figure 2 - Endoscopic images at time of current presentation: Recurrence of proximal esophageal stricture (left panel) which was dilated with Maloney 44F, 48F and 52F with dilation effect. There was a mucosal rent revealed post-dilation (right panel).
Disclosures:
Jake Cresta indicated no relevant financial relationships.
Roy Wong indicated no relevant financial relationships.
Robert Spiller indicated no relevant financial relationships.
Jake Cresta, MD, Roy Wong, MD, Robert Spiller, DO, MS. P4971 - The Perfect Storm: Lymphocytic Esophagitis in an HIV-Positive Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Walter Reed National Military Medical Center, Bethesda, MD
Introduction: Lymphocytic esophagitis (LyE) is a rare inflammatory disorder of the esophagus, first described in 2006, characterized by increased intraepithelial lymphocytes. It is associated with immune-mediated conditions and chronic esophageal irritation. Clinically and endoscopically, LyE mimics eosinophilic esophagitis (EoE) and has been linked to autoimmune diseases and immunodeficiencies. Due to its rarity, treatment is empiric and often includes proton pump inhibitors (PPIs) and topical corticosteroids.
Case Description/
Methods: A 46-year-old female with well-controlled HIV and a history of recurrent esophageal candidiasis complicated by strictures and Schatzki rings presented with progressive dysphagia. Despite prior fluconazole therapy, periodic dilations, and long-term PPI use, she experienced worsening symptoms after self-discontinuing omeprazole. Esophagogastroduodenoscopy revealed a persistent stricture, dilated with an 52F Maloney dilator. Biopsies from the mid-esophagus demonstrated marked intraepithelial lymphocytosis and benign squamous epithelium with spongiosis, but no eosinophils or fungal elements, consistent with LyE. The patient was restarted on omeprazole 40 mg daily and swallowed fluticasone, leading to significant symptom improvement.
Discussion: This case underscores LyE as an underrecognized esophageal condition, particularly in immunocompromised individuals. Though often associated with autoimmune disorders, its relationship with chronic infections like HIV and Candida esophagitis is poorly understood. While Candida can also cause intraepithelial lymphocytosis, the absence of fungal elements on biopsy excluded this etiology. LyE and EoE share overlapping features, including dysphagia and esophageal webs, though LyE is less often associated with food impaction. Histologic findings in LyE include peripapillary lymphocytosis, spongiosis, and absence of eosinophils or pathogens. Diagnosis is generally based on intraepithelial lymphocyte counts >20 per high-power field (normal: 3-10). Management includes PPIs, swallowed corticosteroids, and endoscopic dilation. Mucosal corticosteroid injections may also reduce inflammation and fibrosis. This case illustrates the complex interplay of immune dysfunction, chronic infection, and esophageal irritation in the pathogenesis of LyE. It highlights the need for heightened clinical awareness and further research to define standardized diagnostic and treatment approaches for this emerging condition.
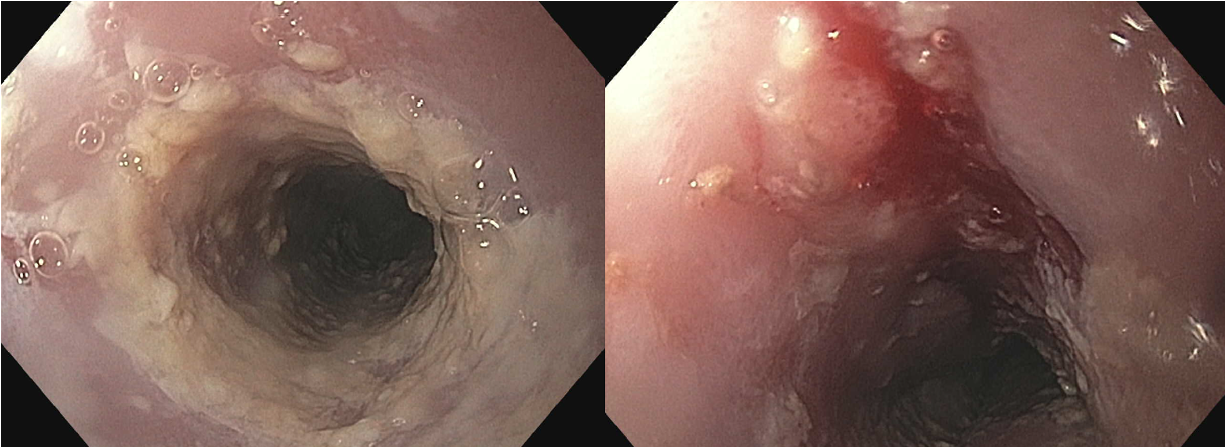
Figure: Figure 1 - Endoscopic images from several years earlier: Left panel demonstrates the proximal esophagus with short, friable stricture at 22cm from incisors which was intervally dilated with Maloney 28F and 32F. Dilation effect visualized on the right panel.
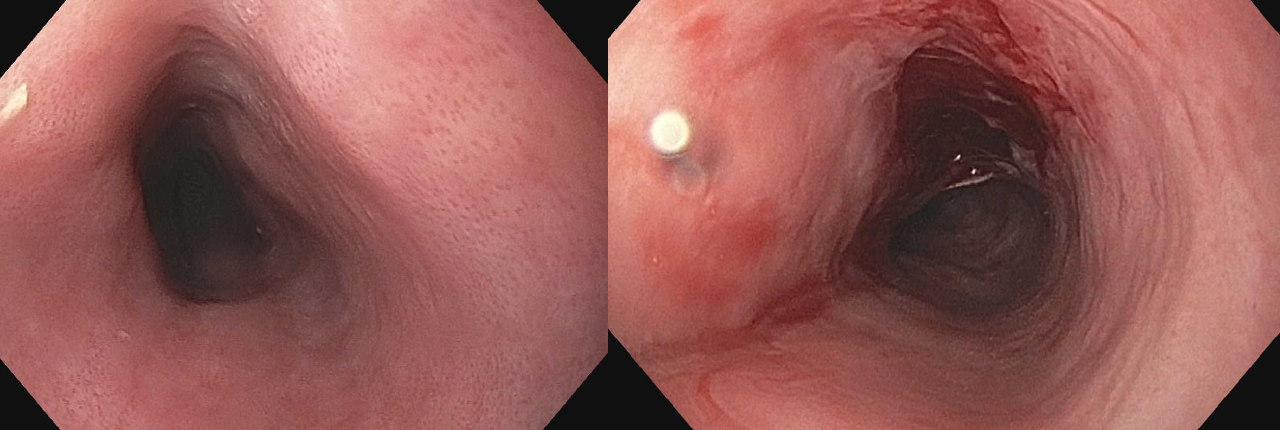
Figure: Figure 2 - Endoscopic images at time of current presentation: Recurrence of proximal esophageal stricture (left panel) which was dilated with Maloney 44F, 48F and 52F with dilation effect. There was a mucosal rent revealed post-dilation (right panel).
Disclosures:
Jake Cresta indicated no relevant financial relationships.
Roy Wong indicated no relevant financial relationships.
Robert Spiller indicated no relevant financial relationships.
Jake Cresta, MD, Roy Wong, MD, Robert Spiller, DO, MS. P4971 - The Perfect Storm: Lymphocytic Esophagitis in an HIV-Positive Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
