Tuesday Poster Session
Category: Esophagus
P4969 - Esophageal Manifestations of Mediastinal Histoplasmosis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Vanessa I. Rodriguez, MD
Vanderbilt University Medical Center
Nashville, TN
Presenting Author(s)
Vanessa I. Rodriguez, MD, Lauren Sanchez, MD, Adesola Oje, MD, Rishi Naik, MD
Vanderbilt University Medical Center, Nashville, TN
Introduction:
Histoplasmosis, endemic to the Ohio and Mississippi River valleys, primarily affects humans through inhalation of spores from contaminated soil. While most immunocompetent hosts experience self-limited disease, some develop significant complications. Diagnosis is challenging as manifestations can mimic malignancy, tuberculosis, and sarcoidosis. Antigen testing may be negative in localized disease, often necessitating tissue biopsy for definitive diagnosis.
Esophageal involvement in mediastinal histoplasmosis can lead to significant complications. We present a 44-year-old immunocompetent female who developed esophageal diverticula and pericarditis following histoplasmosis infection.
Case Description/
Methods: A 44-year-old female with prior gastric sleeve surgery developed dysphagia, chest pain, and fever during a cruise. Initially diagnosed with COVID-19, symptoms worsened despite treatment. CT imaging revealed a 4.4 x 7 cm mediastinal mass with extension into the subcarinal region (Figure 1). Video-assisted thoracoscopic surgery demonstrated necrotizing granulomatous inflammation with GMS staining, showing rare yeast forms consistent with Histoplasma species.
Treatment included 6 weeks of piperacillin-tazobactam and itraconazole for presumed histoplasmosis despite negative antigen testing. Her course was complicated by esophageal tear requiring stenting and subsequent pericarditis requiring pericardiocentesis. Laboratory studies showed WBC 10.8 x 10^9/L (4.0-11.0) and CRP 273 mg/L (< 10). Itraconazole was discontinued due to possible contribution to her pericarditis.
Endoscopic evaluation revealed a mid-esophageal traction diverticulum related to histoplasmosis-mediated inflammation, and a second possible epiphrenic diverticulum, which is planned for further evaluation to assess for esophagogastric junction outflow obstruction.
Discussion: This case illustrates challenges in diagnosing and managing histoplasmosis in an immunocompetent patient with overlapping respiratory, gastrointestinal, and cardiovascular manifestations. Initial misdiagnosis as viral illness delayed appropriate treatment until tissue diagnosis revealed Histoplasma. The progression from mediastinal involvement to pericarditis with constrictive physiology exemplifies potential complications. This case emphasizes maintaining high suspicion for fungal infections in patients with mediastinal masses, even in immunocompetent hosts, and highlights the importance of tissue diagnosis and multidisciplinary management.
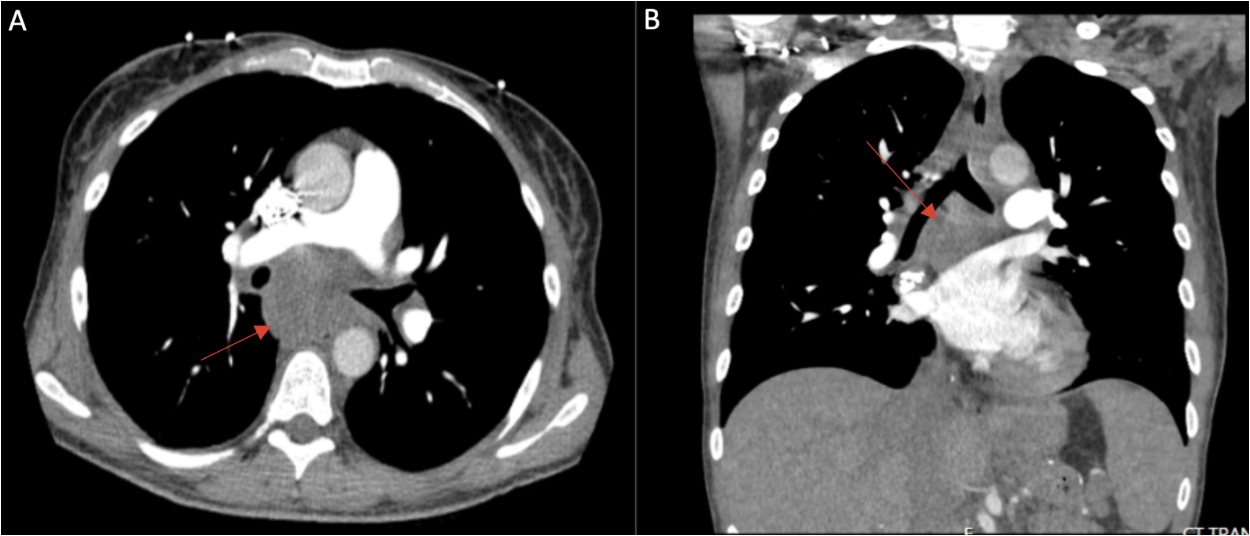
Figure: Figure1: CT chest demonstrating a 4.4 x 7 cm heterogeneous mediastinal mass (red arrows) in axial (A) and coronal (B) views.
Disclosures:
Vanessa Rodriguez indicated no relevant financial relationships.
Lauren Sanchez indicated no relevant financial relationships.
Adesola Oje indicated no relevant financial relationships.
Rishi Naik indicated no relevant financial relationships.
Vanessa I. Rodriguez, MD, Lauren Sanchez, MD, Adesola Oje, MD, Rishi Naik, MD. P4969 - Esophageal Manifestations of Mediastinal Histoplasmosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Vanderbilt University Medical Center, Nashville, TN
Introduction:
Histoplasmosis, endemic to the Ohio and Mississippi River valleys, primarily affects humans through inhalation of spores from contaminated soil. While most immunocompetent hosts experience self-limited disease, some develop significant complications. Diagnosis is challenging as manifestations can mimic malignancy, tuberculosis, and sarcoidosis. Antigen testing may be negative in localized disease, often necessitating tissue biopsy for definitive diagnosis.
Esophageal involvement in mediastinal histoplasmosis can lead to significant complications. We present a 44-year-old immunocompetent female who developed esophageal diverticula and pericarditis following histoplasmosis infection.
Case Description/
Methods: A 44-year-old female with prior gastric sleeve surgery developed dysphagia, chest pain, and fever during a cruise. Initially diagnosed with COVID-19, symptoms worsened despite treatment. CT imaging revealed a 4.4 x 7 cm mediastinal mass with extension into the subcarinal region (Figure 1). Video-assisted thoracoscopic surgery demonstrated necrotizing granulomatous inflammation with GMS staining, showing rare yeast forms consistent with Histoplasma species.
Treatment included 6 weeks of piperacillin-tazobactam and itraconazole for presumed histoplasmosis despite negative antigen testing. Her course was complicated by esophageal tear requiring stenting and subsequent pericarditis requiring pericardiocentesis. Laboratory studies showed WBC 10.8 x 10^9/L (4.0-11.0) and CRP 273 mg/L (< 10). Itraconazole was discontinued due to possible contribution to her pericarditis.
Endoscopic evaluation revealed a mid-esophageal traction diverticulum related to histoplasmosis-mediated inflammation, and a second possible epiphrenic diverticulum, which is planned for further evaluation to assess for esophagogastric junction outflow obstruction.
Discussion: This case illustrates challenges in diagnosing and managing histoplasmosis in an immunocompetent patient with overlapping respiratory, gastrointestinal, and cardiovascular manifestations. Initial misdiagnosis as viral illness delayed appropriate treatment until tissue diagnosis revealed Histoplasma. The progression from mediastinal involvement to pericarditis with constrictive physiology exemplifies potential complications. This case emphasizes maintaining high suspicion for fungal infections in patients with mediastinal masses, even in immunocompetent hosts, and highlights the importance of tissue diagnosis and multidisciplinary management.
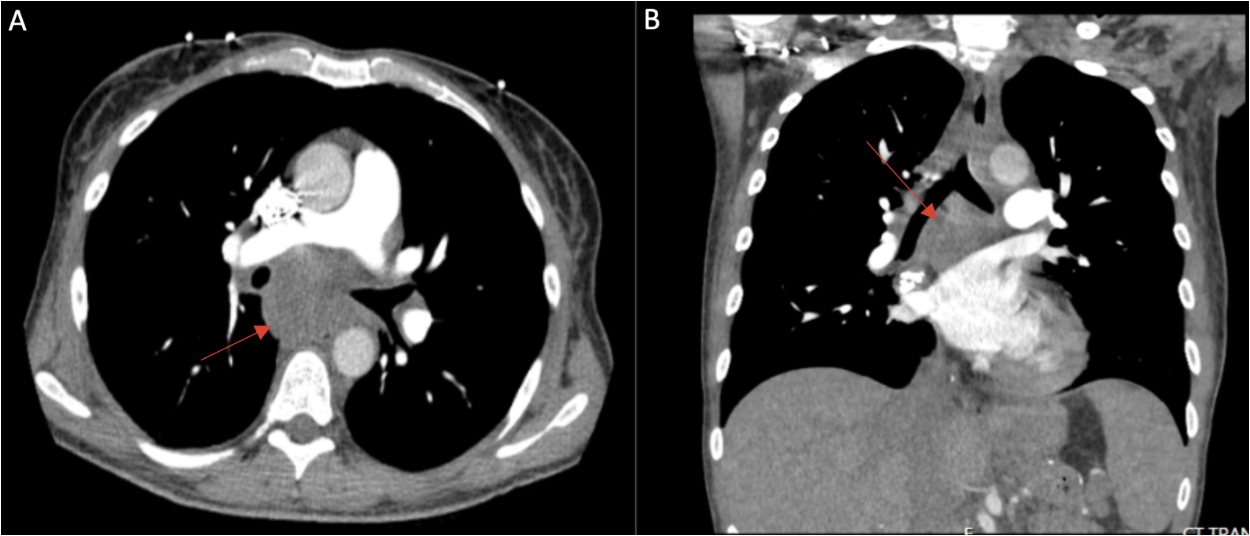
Figure: Figure1: CT chest demonstrating a 4.4 x 7 cm heterogeneous mediastinal mass (red arrows) in axial (A) and coronal (B) views.
Disclosures:
Vanessa Rodriguez indicated no relevant financial relationships.
Lauren Sanchez indicated no relevant financial relationships.
Adesola Oje indicated no relevant financial relationships.
Rishi Naik indicated no relevant financial relationships.
Vanessa I. Rodriguez, MD, Lauren Sanchez, MD, Adesola Oje, MD, Rishi Naik, MD. P4969 - Esophageal Manifestations of Mediastinal Histoplasmosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
