Tuesday Poster Session
Category: Esophagus
P4928 - Higher Risks With Gastrostomy Tube Placement After Esophagectomy: Evidence From the National Inpatient Sample Database
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- RV
Renuka Verma, MD (she/her/hers)
Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas
Las Vegas, NV
Presenting Author(s)
Renuka Verma, MD1, Kaitlyn Gernhard, DO2, Himsikhar Khataniar, MD3, Leandro Sierra, MD4, Sunny Kumar, MD5, Kamleshun Ramphul, MD6, Nikki Duong, MD7
1Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV; 2Allegheny Health Network Medicine Institute, Pittsburgh, PA; 3Allegheny General Hospital, Pittsburgh, PA; 4Department of Internal Medicine, Cleveland Clinic, Cleveland, OH; 5Wright Center for Graduate Medical Education, Scranton, PA; 6Independent researcher, Las Vegas, NV; 7Stanford University, Stanford, CA
Introduction: In advanced esophageal cancer, esophagectomy may be a part of the standard of care for treatment. This morbid surgery may lead to nutritional challenges, which often necessitate feeding tube placement. The efficacy and safety of gastrostomy vs. jejunostomy tube approaches in this setting remain very limited.
Methods: Adults with esophageal cancer who were hospitalized for esophagectomy were extracted via the National Inpatient Sample (2016-2022). Patients under 18 or with pre-existing gastrostomy tubes were excluded. The use of enteral feeding methods during index hospitalization was assessed for clinical characteristics across three groups: gastrostomy, jejunostomy, and no feeding tube placement. The primary outcome was all-cause in-hospital mortality. Secondary outcomes included sepsis, tube malfunction, acute kidney injury (AKI), critical care utilization, length of stay, and hospital charges.
Results: Among 15,365 patients who underwent esophagectomy, 12.9% received jejunostomy tubes, and 3.1% received gastrostomy tubes. The mean age and Charlson Comorbidity Index(CCI) scores between the three groups were comparable. All cohorts were predominantly male, White, and insured through Medicare. While a higher proportion of patients undergoing jejunostomy or gastrostomy tube placement were in the 51st-75th income quartile, a higher number among those without tube placement were one quartile lower (25th-50th). Palliative care use was highest in those undergoing gastrostomy tube placement. Gastrostomy tube placement was associated with significantly higher odds of complications as compared to those undergoing jejunostomy tube placement, including AKI, tube malfunction, sepsis, need for critical care, and all-cause mortality (Table 1b). The gastrostomy tube placement group had longer hospitalizations and incurred higher hospital charges.
Discussion: Compared to jejunostomy, gastrostomy tube placement was associated with significantly worse clinical outcomes and higher resource utilization. Given the rising incidence of esophageal cancer worldwide, it is imperative to optimise enteral access strategies to improve patient care. Future prospective studies are needed to validate these findings.
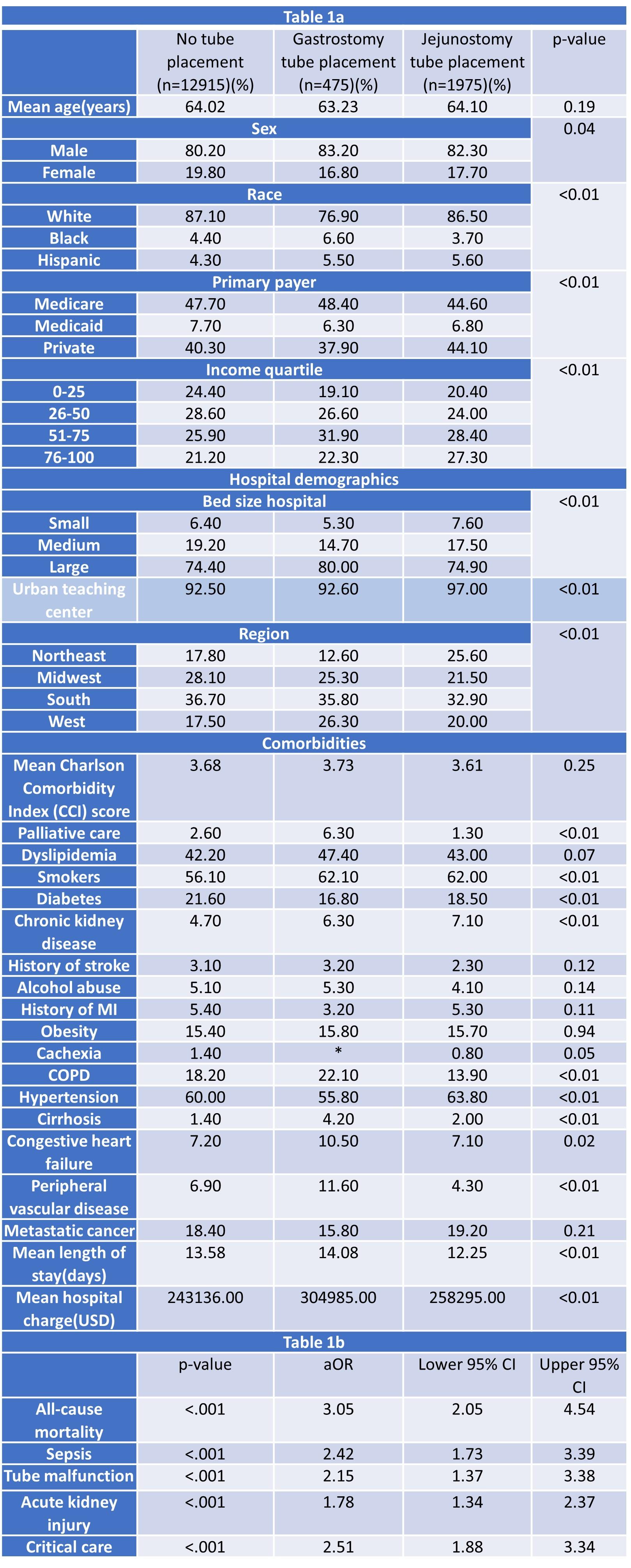
Figure: Table 1a.Comparing demographics of esophageal cancer patients undergoing esophagectomy with vs. without tube placements
Table 1b.Complications in gastrostomy tube placement (vs jejunostomy)
Disclosures:
Renuka Verma indicated no relevant financial relationships.
Kaitlyn Gernhard indicated no relevant financial relationships.
Himsikhar Khataniar indicated no relevant financial relationships.
Leandro Sierra indicated no relevant financial relationships.
Sunny Kumar indicated no relevant financial relationships.
Kamleshun Ramphul indicated no relevant financial relationships.
Nikki Duong indicated no relevant financial relationships.
Renuka Verma, MD1, Kaitlyn Gernhard, DO2, Himsikhar Khataniar, MD3, Leandro Sierra, MD4, Sunny Kumar, MD5, Kamleshun Ramphul, MD6, Nikki Duong, MD7. P4928 - Higher Risks With Gastrostomy Tube Placement After Esophagectomy: Evidence From the National Inpatient Sample Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV; 2Allegheny Health Network Medicine Institute, Pittsburgh, PA; 3Allegheny General Hospital, Pittsburgh, PA; 4Department of Internal Medicine, Cleveland Clinic, Cleveland, OH; 5Wright Center for Graduate Medical Education, Scranton, PA; 6Independent researcher, Las Vegas, NV; 7Stanford University, Stanford, CA
Introduction: In advanced esophageal cancer, esophagectomy may be a part of the standard of care for treatment. This morbid surgery may lead to nutritional challenges, which often necessitate feeding tube placement. The efficacy and safety of gastrostomy vs. jejunostomy tube approaches in this setting remain very limited.
Methods: Adults with esophageal cancer who were hospitalized for esophagectomy were extracted via the National Inpatient Sample (2016-2022). Patients under 18 or with pre-existing gastrostomy tubes were excluded. The use of enteral feeding methods during index hospitalization was assessed for clinical characteristics across three groups: gastrostomy, jejunostomy, and no feeding tube placement. The primary outcome was all-cause in-hospital mortality. Secondary outcomes included sepsis, tube malfunction, acute kidney injury (AKI), critical care utilization, length of stay, and hospital charges.
Results: Among 15,365 patients who underwent esophagectomy, 12.9% received jejunostomy tubes, and 3.1% received gastrostomy tubes. The mean age and Charlson Comorbidity Index(CCI) scores between the three groups were comparable. All cohorts were predominantly male, White, and insured through Medicare. While a higher proportion of patients undergoing jejunostomy or gastrostomy tube placement were in the 51st-75th income quartile, a higher number among those without tube placement were one quartile lower (25th-50th). Palliative care use was highest in those undergoing gastrostomy tube placement. Gastrostomy tube placement was associated with significantly higher odds of complications as compared to those undergoing jejunostomy tube placement, including AKI, tube malfunction, sepsis, need for critical care, and all-cause mortality (Table 1b). The gastrostomy tube placement group had longer hospitalizations and incurred higher hospital charges.
Discussion: Compared to jejunostomy, gastrostomy tube placement was associated with significantly worse clinical outcomes and higher resource utilization. Given the rising incidence of esophageal cancer worldwide, it is imperative to optimise enteral access strategies to improve patient care. Future prospective studies are needed to validate these findings.
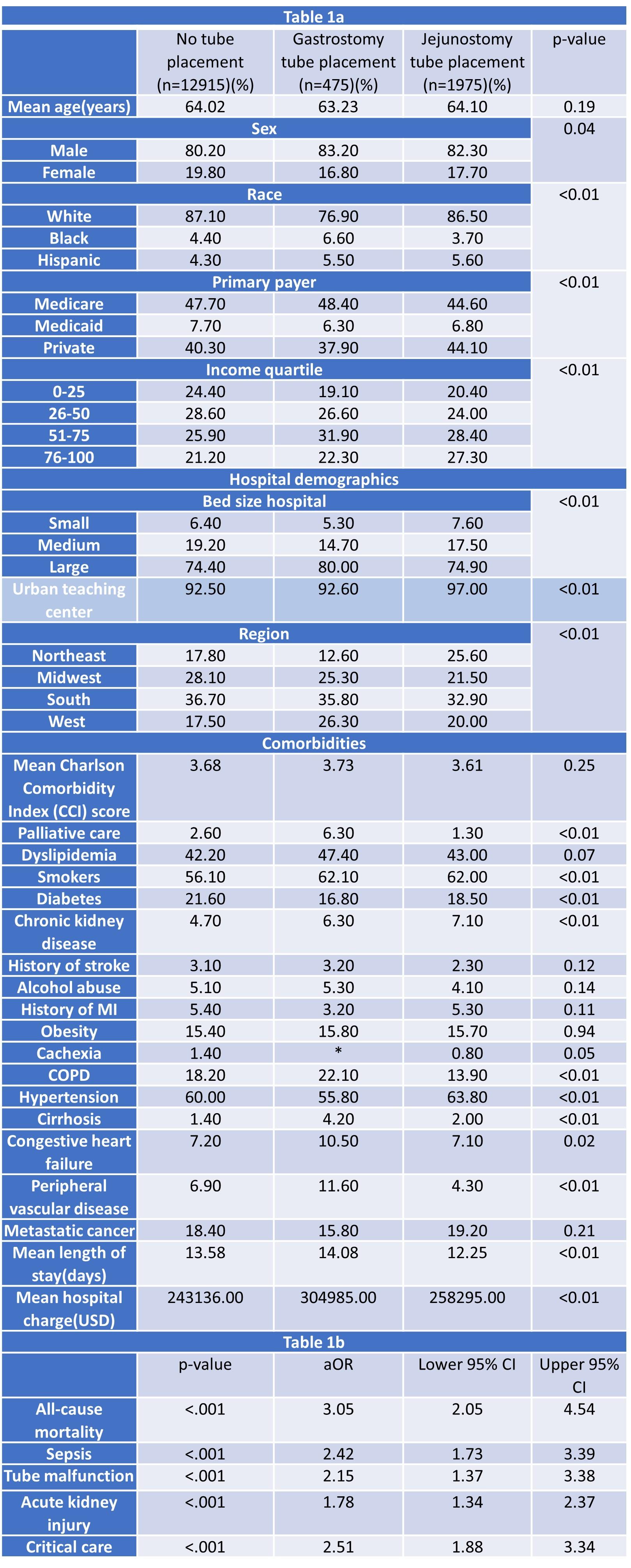
Figure: Table 1a.Comparing demographics of esophageal cancer patients undergoing esophagectomy with vs. without tube placements
Table 1b.Complications in gastrostomy tube placement (vs jejunostomy)
Disclosures:
Renuka Verma indicated no relevant financial relationships.
Kaitlyn Gernhard indicated no relevant financial relationships.
Himsikhar Khataniar indicated no relevant financial relationships.
Leandro Sierra indicated no relevant financial relationships.
Sunny Kumar indicated no relevant financial relationships.
Kamleshun Ramphul indicated no relevant financial relationships.
Nikki Duong indicated no relevant financial relationships.
Renuka Verma, MD1, Kaitlyn Gernhard, DO2, Himsikhar Khataniar, MD3, Leandro Sierra, MD4, Sunny Kumar, MD5, Kamleshun Ramphul, MD6, Nikki Duong, MD7. P4928 - Higher Risks With Gastrostomy Tube Placement After Esophagectomy: Evidence From the National Inpatient Sample Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
