Tuesday Poster Session
Category: Esophagus
P4914 - Association Between SGLT2 Inhibitor Use and the Risk of Eosinophilic Esophagitis in Patients With Type 2 Diabetes Mellitus: A Retrospective Cohort Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- MD
Miqdad Dafaallah, MD (he/him/his)
Mercyone Des Moines Medical Center
Chelsea, MA
Presenting Author(s)
Miqdad Dafaallah, MD1, Ali Osman, MD, MSCI Candidate2, Abdelaziz Mohamed, MBBS3, Monzer Abdalla, MD4, Mohamed Abdallah, MD5
1Mercyone Des Moines Medical Center, Iowa, IA; 2Washington University School of Medicine in St. Louis, Ballwin, MO; 3One Brooklyn Health-Interfaith Medical Center, Brooklyn, NY; 4Rosalind Franklin University of Medicine and Science, Evanston, IL; 5Corewell Health, Royal Oak, MI
Introduction: Sodium-Glucose Cotransporter 2 inhibitors (SGLT2is) are widely used to treat type 2 diabetes mellitus (T2DM) and recent interest has emerged in their potential immune-modulating effects(1). SGLT2is have shown to have anti-inflammatory effects which are related to their cardiovascular and renal outcomes in patients with T2DM(2). Therefore, the protective association between eosinophilic eosophagitis (EoE) and SGLT2is may be biologically possible given that EoE pathogenesis is driven by type 2 cytokine-mediated inflammation, promoting eosinophil infiltration(3). This retrospective cohort study explores the association between SGLT2 inhibitor use and the risk of developing EoE in patients with T2DM.
Methods: We performed a retrospective cohort study using the TriNetX Global Collaborative Network. Adults aged 18-65 with T2DM were included and divided into two cohorts: those prescribed SGLT2is and those treated with other antidiabetic medications. Patients with type 1 diabetes mellitus, prior EoE, IBD, connective tissue disease, malignancy, or history of bariatric or esophageal surgeries were excluded. Propensity score matching was performed. The primary outcome was a new diagnosis of EoE after cohort entry. Risk analysis and Kaplan-Meier survival analysis were conducted.
Results: After matching, 37,948 patients were included in each group. Baseline characteristics were balanced (Table 1). 358 patients in SGLT2i users and 536 patients in non-SGLT2i users were excluded from the results because they had the outcome prior to starting them on antidiabetic medications. Incident EoE occurred in 269 (0.072%) SGT2i users and 371 (0.099%) in non SGLT2i users. SGLT2i use was associated with 38% relative reduction in EoE risk (RR 1.38; 95% Cl 1.179-1.614; p< 0.001). Survival analysis showed no significant difference in time to diagnosis (HR 1.093; 95% Cl 0.931-1.282; p=0.14) (Table 2 and 3)
Discussion: SGLTis were associated with a significantly reduced risk of EoE incidence in patients with T2DM. The lack of significance in time-to-diagnosis analysis may reflect the low incidence of EoE, diagnostic delays, or uniform endoscopic surveillance across cohorts. Limitations of this study include reliance on ICD coding for the outcome without histologic confirmation and unmeasured confounding related to healthcare utilization patterns (e.g. frequency of EGD).
These findings suggest a possible immune-modulating role for SGLT2is and may guide future research into inflammation-targeted therapies in EoE.
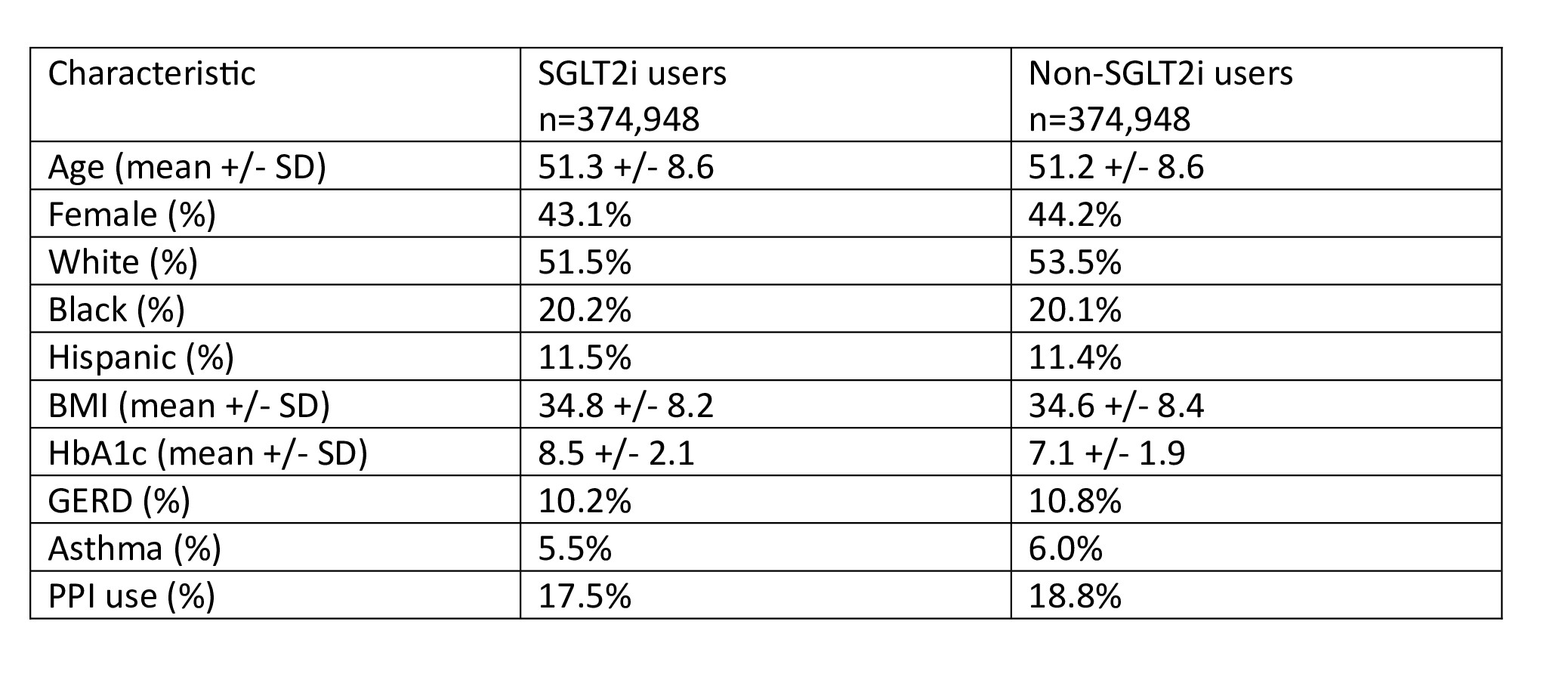
Figure: Table 1: Baseline characteristics after matching
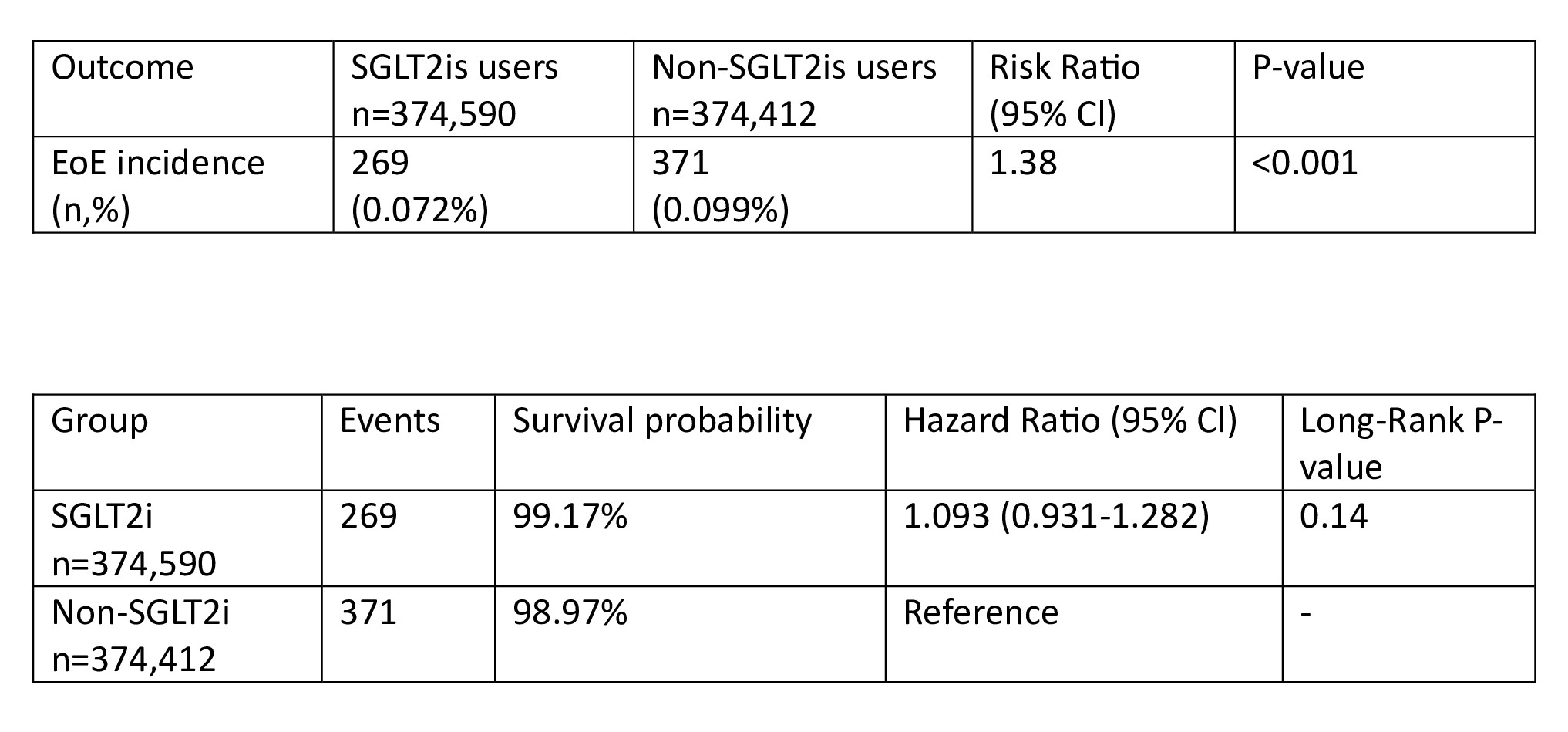
Figure: Table 2: EoE incidence risk analysis and Table 3: Kaplan-Meier Survival analysis
Disclosures:
Miqdad Dafaallah indicated no relevant financial relationships.
Ali Osman indicated no relevant financial relationships.
Abdelaziz Mohamed indicated no relevant financial relationships.
Monzer Abdalla indicated no relevant financial relationships.
Mohamed Abdallah indicated no relevant financial relationships.
Miqdad Dafaallah, MD1, Ali Osman, MD, MSCI Candidate2, Abdelaziz Mohamed, MBBS3, Monzer Abdalla, MD4, Mohamed Abdallah, MD5. P4914 - Association Between SGLT2 Inhibitor Use and the Risk of Eosinophilic Esophagitis in Patients With Type 2 Diabetes Mellitus: A Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mercyone Des Moines Medical Center, Iowa, IA; 2Washington University School of Medicine in St. Louis, Ballwin, MO; 3One Brooklyn Health-Interfaith Medical Center, Brooklyn, NY; 4Rosalind Franklin University of Medicine and Science, Evanston, IL; 5Corewell Health, Royal Oak, MI
Introduction: Sodium-Glucose Cotransporter 2 inhibitors (SGLT2is) are widely used to treat type 2 diabetes mellitus (T2DM) and recent interest has emerged in their potential immune-modulating effects(1). SGLT2is have shown to have anti-inflammatory effects which are related to their cardiovascular and renal outcomes in patients with T2DM(2). Therefore, the protective association between eosinophilic eosophagitis (EoE) and SGLT2is may be biologically possible given that EoE pathogenesis is driven by type 2 cytokine-mediated inflammation, promoting eosinophil infiltration(3). This retrospective cohort study explores the association between SGLT2 inhibitor use and the risk of developing EoE in patients with T2DM.
Methods: We performed a retrospective cohort study using the TriNetX Global Collaborative Network. Adults aged 18-65 with T2DM were included and divided into two cohorts: those prescribed SGLT2is and those treated with other antidiabetic medications. Patients with type 1 diabetes mellitus, prior EoE, IBD, connective tissue disease, malignancy, or history of bariatric or esophageal surgeries were excluded. Propensity score matching was performed. The primary outcome was a new diagnosis of EoE after cohort entry. Risk analysis and Kaplan-Meier survival analysis were conducted.
Results: After matching, 37,948 patients were included in each group. Baseline characteristics were balanced (Table 1). 358 patients in SGLT2i users and 536 patients in non-SGLT2i users were excluded from the results because they had the outcome prior to starting them on antidiabetic medications. Incident EoE occurred in 269 (0.072%) SGT2i users and 371 (0.099%) in non SGLT2i users. SGLT2i use was associated with 38% relative reduction in EoE risk (RR 1.38; 95% Cl 1.179-1.614; p< 0.001). Survival analysis showed no significant difference in time to diagnosis (HR 1.093; 95% Cl 0.931-1.282; p=0.14) (Table 2 and 3)
Discussion: SGLTis were associated with a significantly reduced risk of EoE incidence in patients with T2DM. The lack of significance in time-to-diagnosis analysis may reflect the low incidence of EoE, diagnostic delays, or uniform endoscopic surveillance across cohorts. Limitations of this study include reliance on ICD coding for the outcome without histologic confirmation and unmeasured confounding related to healthcare utilization patterns (e.g. frequency of EGD).
These findings suggest a possible immune-modulating role for SGLT2is and may guide future research into inflammation-targeted therapies in EoE.
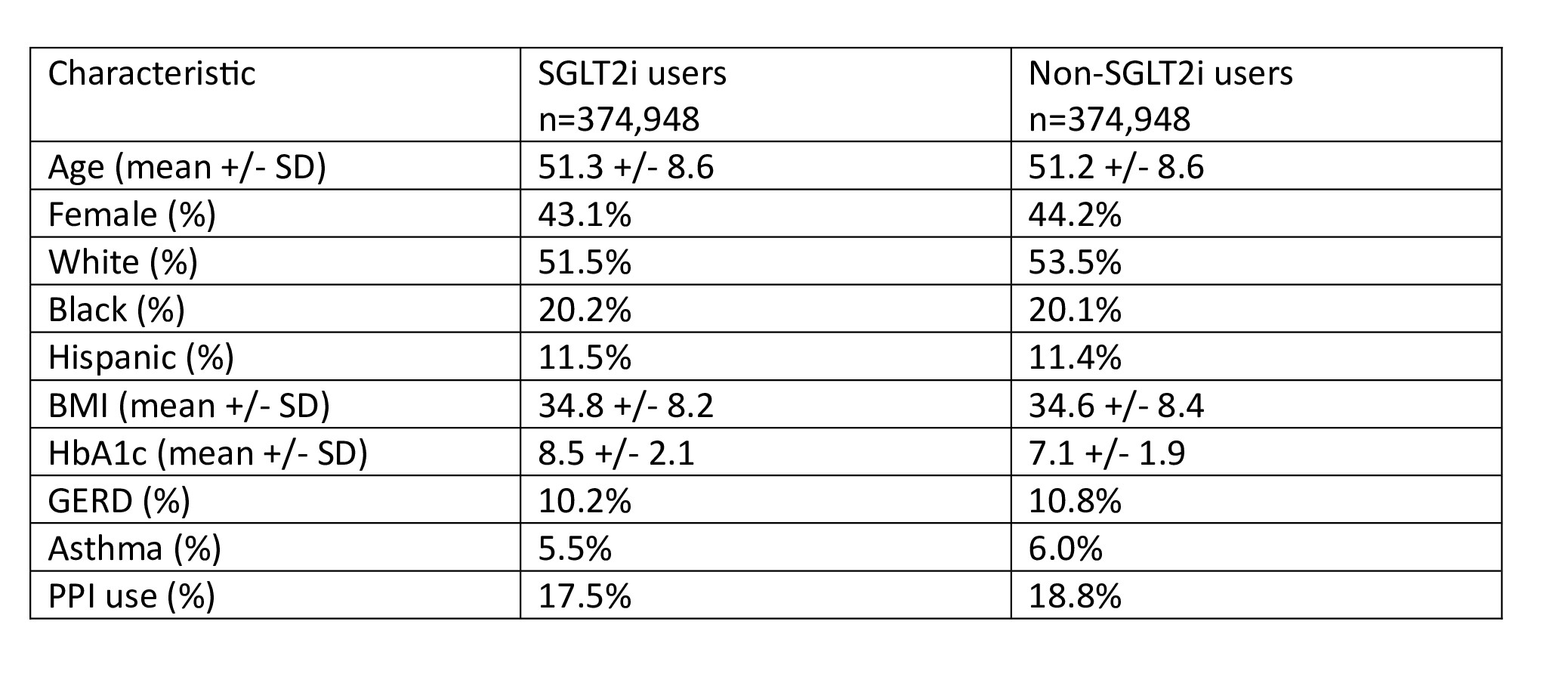
Figure: Table 1: Baseline characteristics after matching
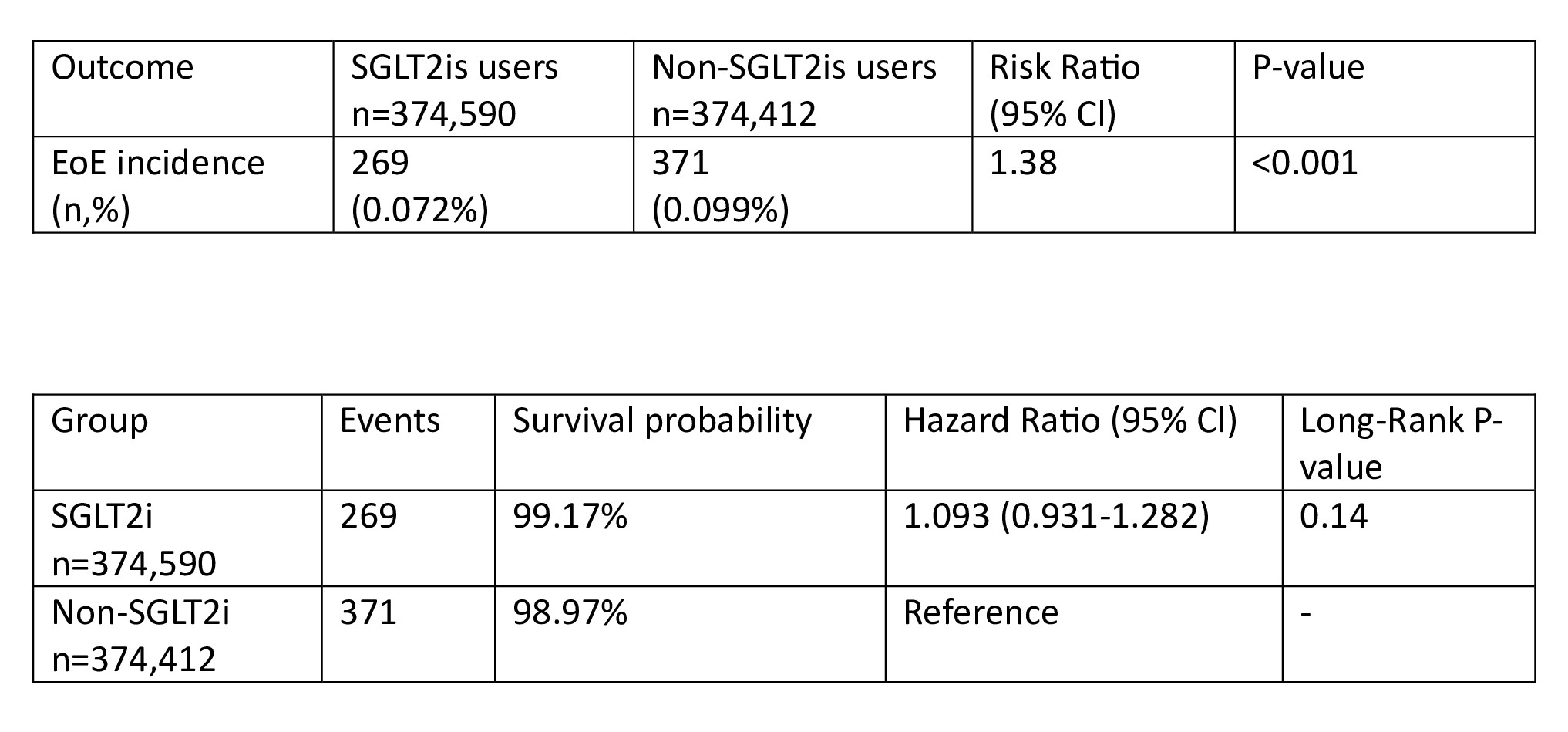
Figure: Table 2: EoE incidence risk analysis and Table 3: Kaplan-Meier Survival analysis
Disclosures:
Miqdad Dafaallah indicated no relevant financial relationships.
Ali Osman indicated no relevant financial relationships.
Abdelaziz Mohamed indicated no relevant financial relationships.
Monzer Abdalla indicated no relevant financial relationships.
Mohamed Abdallah indicated no relevant financial relationships.
Miqdad Dafaallah, MD1, Ali Osman, MD, MSCI Candidate2, Abdelaziz Mohamed, MBBS3, Monzer Abdalla, MD4, Mohamed Abdallah, MD5. P4914 - Association Between SGLT2 Inhibitor Use and the Risk of Eosinophilic Esophagitis in Patients With Type 2 Diabetes Mellitus: A Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

