Tuesday Poster Session
Category: Esophagus
P4912 - Potassium-Competitive Acid Blockers vs Proton Pump Inhibitors: A Real-World Comparative Effectiveness Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- KA
Khaled Alsabbagh Alchirazi, MD
Aurora Health Care
Brookfield, WI
Presenting Author(s)
Khaled Alsabbagh Alchirazi, MD1, Muaz Alsabbagh, MD2, Kinan Obeidat, MD3, Ahmed N.. Mohamed, MD4, Michelle Baliss, DO5, Ahmad Bazarbashi, MD6
1Aurora Health Care, Brookfield, WI; 2Detroit Medical Center/Wayne State University, Cleveland, OH; 3University of Texas Medical Branch, Santa Fe, TX; 4Cleveland Clinic Foundation, South Euclid, OH; 5Washington University School of Medicine in St. Louis, St. Louis, MO; 6Washington University School of Medicine in St. Louis / Barnes-Jewish Hospital, St. Louis, WA
Introduction: Gastroesophageal reflux disease (GERD) is a common condition that significantly impairs quality of life and may lead to serious complications. Proton pump inhibitors (PPIs) are widely used but limited by delayed onset, variable efficacy, and incomplete symptom relief in some patients. Potassium-competitive acid blockers (PCABs), which provide rapid and sustained acid suppression, have emerged as a promising alternative. This study compared real-world clinical outcomes of PCABs versus PPIs in patients with GERD and related acid-mediated disorders.
Methods: A retrospective cohort study was conducted using the TriNetX research network. Adult patients diagnosed with GERD, esophagitis, or peptic ulcer disease who received a PCAB or PPI were included. Propensity score matching (1:1) was performed to balance cohorts for demographics, comorbidities, antiplatelet and anticoagulant use, Helicobacter pylori status, and NSAID exposure. The primary outcome was gastrointestinal (GI) bleeding. Secondary outcomes included hospitalization, need for critical care, GI perforation, Clostridioides difficile infection (CDI), need for endoscopy, transfusion, and overall mortality. Logistic regression was used to estimate odds ratios (ORs) with 95% confidence intervals (CIs).
Results: After matching, 1,726 patients were included in each group with balanced baseline characteristics. Males comprised 56.9% of the PCAB group and 55.9% of the PPI group; over 80% were White. At 2-year follow-up, PCABs were associated with significantly better outcomes. Compared to PPIs, PCABs had lower risks of GI bleeding (OR 0.47, 95% CI 0.25–0.86), critical care need (OR 0.29, 95% CI 0.20–0.42), hospitalization (OR 0.42, 95% CI 0.32–0.54), and overall mortality (OR 0.23, 95% CI 0.15–0.34). PCABs also had lower odds of CDI (OR 0.57, 95% CI 0.37–0.89), EGD (OR 0.80, 95% CI 0.66–0.97), and transfusion (OR 0.21, 95% CI 0.12–0.37). No significant difference was seen in GI perforation (OR 1.01, 95% CI 0.42–2.43).
Discussion: In this large real-world matched cohort, PCABs were associated with superior outcomes compared to PPIs, including reduced risks of GI bleeding, hospitalization, intensive care, and death. These findings support PCABs as a potential alternative to PPIs, particularly for high-risk or treatment-resistant patients. Prospective studies are warranted to confirm these benefits and assess long-term safety.
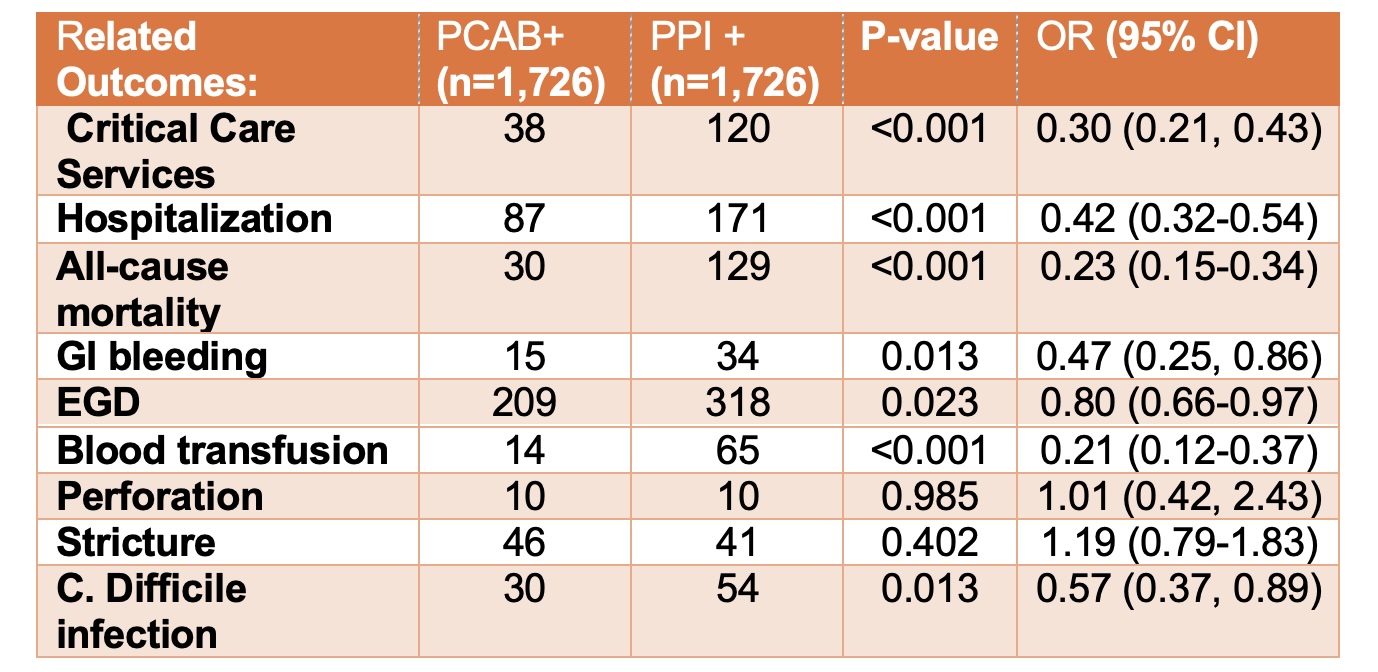
Figure: Clinical outcomes in matched patients treated with PCABs vs PPIs.
Disclosures:
Khaled Alsabbagh Alchirazi indicated no relevant financial relationships.
Muaz Alsabbagh indicated no relevant financial relationships.
Kinan Obeidat indicated no relevant financial relationships.
Ahmed Mohamed indicated no relevant financial relationships.
Michelle Baliss indicated no relevant financial relationships.
Ahmad Bazarbashi indicated no relevant financial relationships.
Khaled Alsabbagh Alchirazi, MD1, Muaz Alsabbagh, MD2, Kinan Obeidat, MD3, Ahmed N.. Mohamed, MD4, Michelle Baliss, DO5, Ahmad Bazarbashi, MD6. P4912 - Potassium-Competitive Acid Blockers vs Proton Pump Inhibitors: A Real-World Comparative Effectiveness Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Aurora Health Care, Brookfield, WI; 2Detroit Medical Center/Wayne State University, Cleveland, OH; 3University of Texas Medical Branch, Santa Fe, TX; 4Cleveland Clinic Foundation, South Euclid, OH; 5Washington University School of Medicine in St. Louis, St. Louis, MO; 6Washington University School of Medicine in St. Louis / Barnes-Jewish Hospital, St. Louis, WA
Introduction: Gastroesophageal reflux disease (GERD) is a common condition that significantly impairs quality of life and may lead to serious complications. Proton pump inhibitors (PPIs) are widely used but limited by delayed onset, variable efficacy, and incomplete symptom relief in some patients. Potassium-competitive acid blockers (PCABs), which provide rapid and sustained acid suppression, have emerged as a promising alternative. This study compared real-world clinical outcomes of PCABs versus PPIs in patients with GERD and related acid-mediated disorders.
Methods: A retrospective cohort study was conducted using the TriNetX research network. Adult patients diagnosed with GERD, esophagitis, or peptic ulcer disease who received a PCAB or PPI were included. Propensity score matching (1:1) was performed to balance cohorts for demographics, comorbidities, antiplatelet and anticoagulant use, Helicobacter pylori status, and NSAID exposure. The primary outcome was gastrointestinal (GI) bleeding. Secondary outcomes included hospitalization, need for critical care, GI perforation, Clostridioides difficile infection (CDI), need for endoscopy, transfusion, and overall mortality. Logistic regression was used to estimate odds ratios (ORs) with 95% confidence intervals (CIs).
Results: After matching, 1,726 patients were included in each group with balanced baseline characteristics. Males comprised 56.9% of the PCAB group and 55.9% of the PPI group; over 80% were White. At 2-year follow-up, PCABs were associated with significantly better outcomes. Compared to PPIs, PCABs had lower risks of GI bleeding (OR 0.47, 95% CI 0.25–0.86), critical care need (OR 0.29, 95% CI 0.20–0.42), hospitalization (OR 0.42, 95% CI 0.32–0.54), and overall mortality (OR 0.23, 95% CI 0.15–0.34). PCABs also had lower odds of CDI (OR 0.57, 95% CI 0.37–0.89), EGD (OR 0.80, 95% CI 0.66–0.97), and transfusion (OR 0.21, 95% CI 0.12–0.37). No significant difference was seen in GI perforation (OR 1.01, 95% CI 0.42–2.43).
Discussion: In this large real-world matched cohort, PCABs were associated with superior outcomes compared to PPIs, including reduced risks of GI bleeding, hospitalization, intensive care, and death. These findings support PCABs as a potential alternative to PPIs, particularly for high-risk or treatment-resistant patients. Prospective studies are warranted to confirm these benefits and assess long-term safety.
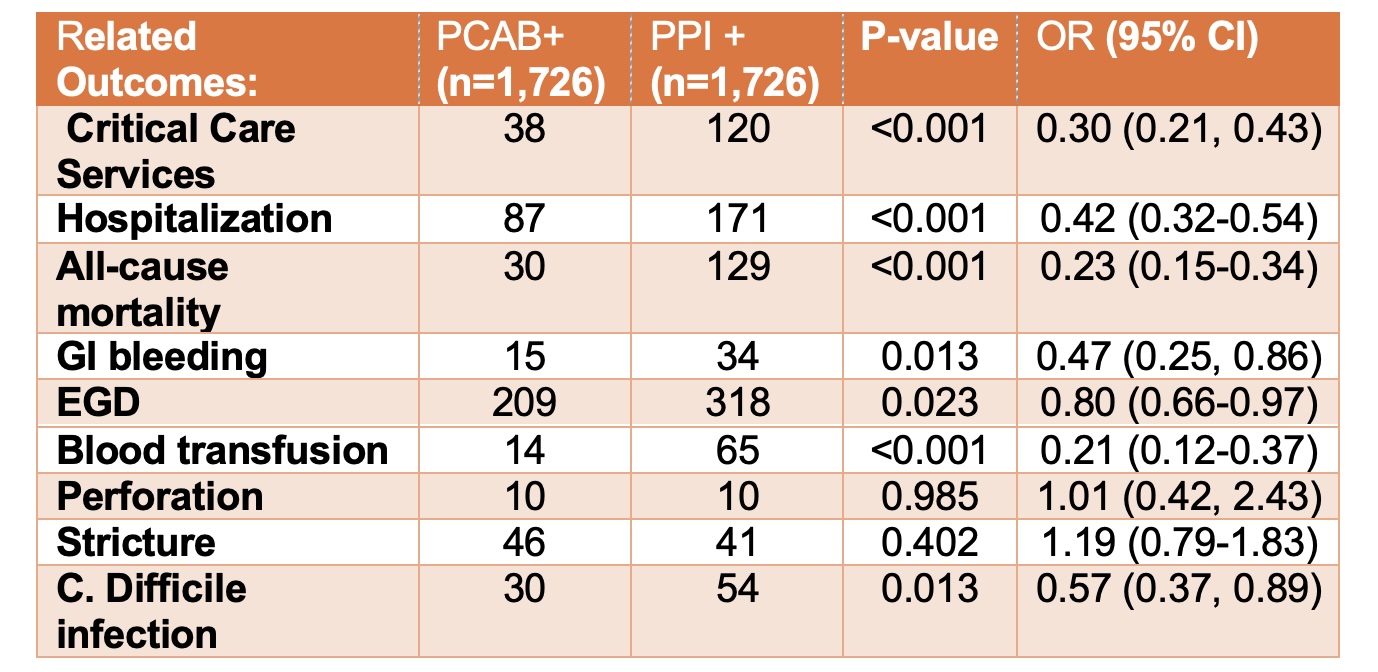
Figure: Clinical outcomes in matched patients treated with PCABs vs PPIs.
Disclosures:
Khaled Alsabbagh Alchirazi indicated no relevant financial relationships.
Muaz Alsabbagh indicated no relevant financial relationships.
Kinan Obeidat indicated no relevant financial relationships.
Ahmed Mohamed indicated no relevant financial relationships.
Michelle Baliss indicated no relevant financial relationships.
Ahmad Bazarbashi indicated no relevant financial relationships.
Khaled Alsabbagh Alchirazi, MD1, Muaz Alsabbagh, MD2, Kinan Obeidat, MD3, Ahmed N.. Mohamed, MD4, Michelle Baliss, DO5, Ahmad Bazarbashi, MD6. P4912 - Potassium-Competitive Acid Blockers vs Proton Pump Inhibitors: A Real-World Comparative Effectiveness Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
