Tuesday Poster Session
Category: Esophagus
P4908 - Endoscopic Management of Large Esophageal Mucosal Tears: A Systematic Review of Modern Closure Techniques and Outcomes
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mahmoud Barbarawi, MD (he/him/his)
DHR Health in affiliation with University of Houston, Tilman J. Fertitta College of Medicine
McAllen, TX
Presenting Author(s)
Mahmoud Barbarawi, MD1, Jathniel Panneflek, MD1, Majdi Salahie, MD2, Zaid Barbarawi, MD3, Adriana R. Silva Marin, MD4, Helen Mejia, MD5
1DHR Health in affiliation with University of Houston, Tilman J. Fertitta College of Medicine, McAllen, TX; 2DHR Health, McAllen, TX; 3Jordan University of Science and Technology, McAllen, TX; 4Facultad de Medicina Alberto Hurtado, Universidad Peruana Cayetano Heredia, McAllen, TX; 5Antillean Adventist Hospital, Willemstad, TX
Introduction: Large esophageal mucosal tears are life-threatening injuries traditionally managed surgically, but endoscopic techniques have emerged as effective first-line therapies. However, optimal endoscopic modality selection and predictors of success remain unclear. This systematic review evaluates the efficacy of endoscopic closure methods and identifies key factors influencing clinical success.
Methods: Following PRISMA guidelines, we searched PubMed, Embase, and Scopus (2010-2024) for studies reporting endoscopic management of large esophageal tears/perforations. We excluded small Mallory-Weiss tears and included English-language studies of all designs. Primary outcome was clinical success (complete healing within 30 days without surgery). Secondary outcomes included technical success, complications, and mortality. Qualitative synthesis was performed with quantitative pooling where data permitted.
Results: From 412 records identified, 38 studies met inclusion criteria after removing duplicates and screening, encompassing esophageal tears from various etiologies (spontaneous ruptures, iatrogenic perforations). Over-the-scope clips (OTSC) were most used (approximately 75% of studies), followed by endoscopic suturing and covered self-expanding metal stents. Pooled clinical success rate was approximately 85% with moderate heterogeneity between studies. OTSC demonstrated high success rates (80-95%) for acute perforations when deployed promptly. Endoscopic suturing showed favorable immediate outcomes (~88%) though long-term durability was lower (55-60%). Key predictors of endoscopic failure included: defect size >20mm, delayed intervention beyond 24-48 hours, poor tissue quality, and ongoing distal obstruction. Iatrogenic perforations had better outcomes than spontaneous ruptures. Procedure-related complications were uncommon, with 10-15% requiring surgical salvage. Overall mortality was low (5-10%) and primarily related to perforation-related sepsis rather than endoscopic procedures.
Discussion: Endoscopic management is highly effective for appropriately selected large esophageal tears when performed promptly by experienced operators. Success depends critically on timing, defect characteristics, and technique selection. We propose an algorithmic approach: OTSC for defects 2-3cm, endoscopic suturing for 3-5cm tears, and covered stents when primary closure fails. These findings support endoscopic therapy as 1st-line treatment for large esophageal tears, potentially avoiding major surgical morbidity.
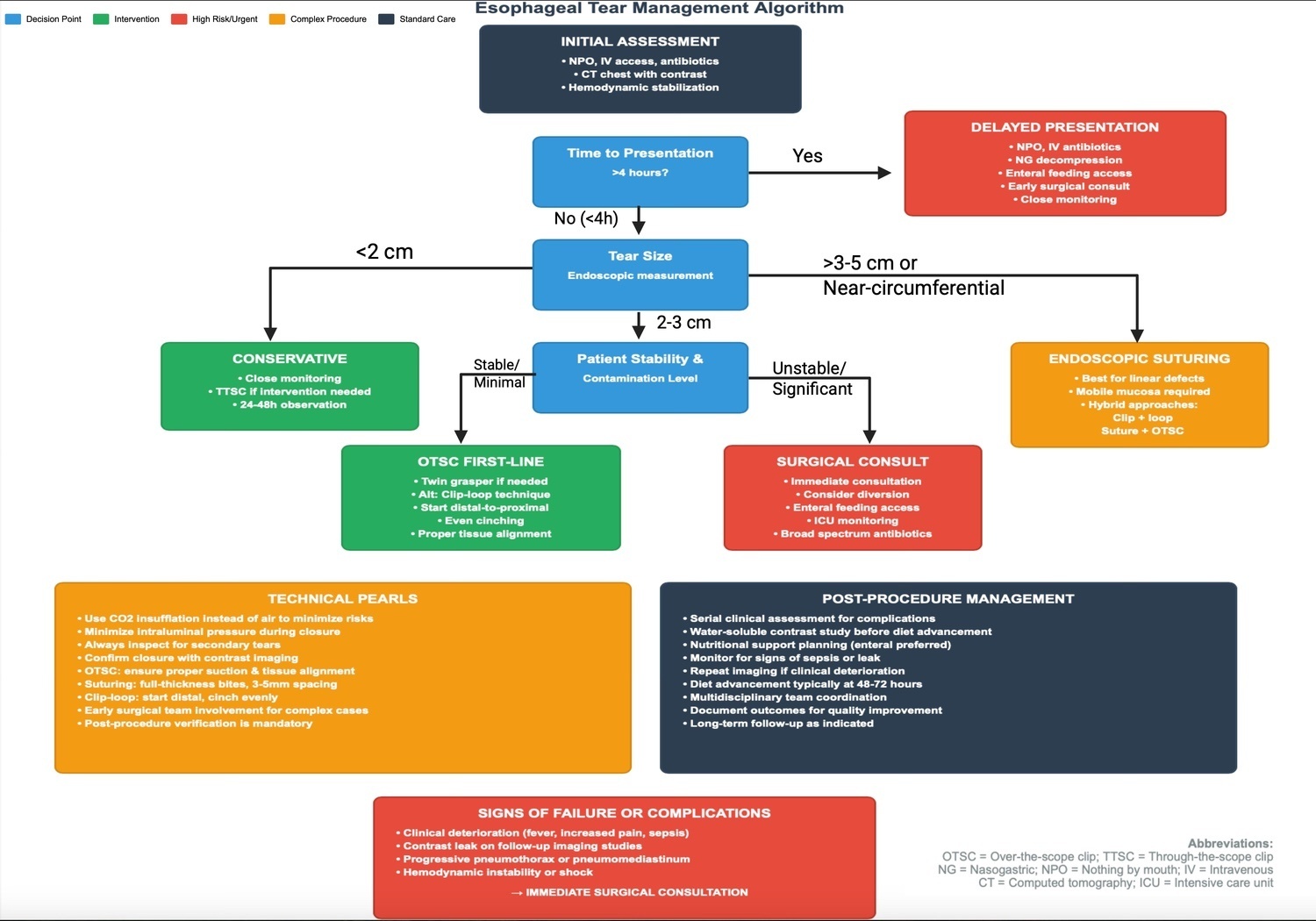
Figure: Figure 1: Proposed algorithm for endoscopic management of esophageal mucosal tears.
Decision-making is based on defect size, timing of presentation, and patient stability. OTSC is recommended for 2–3 cm tears, endoscopic suturing for 3–5 cm defects, and covered stents for failed primary closure or extensive injury. Early surgical consultation is advised for large, delayed, or complicated cases.

Figure: Figure 2: PRISMA flow diagram outlining the study selection process.
Depicts the number of records identified, screened, assessed for eligibility, and ultimately included in the systematic review on endoscopic management of large esophageal mucosal tears, with reasons for exclusion at each stage.
Tables with specifics can be provided upon request.
Disclosures:
Mahmoud Barbarawi indicated no relevant financial relationships.
Jathniel Panneflek indicated no relevant financial relationships.
Majdi Salahie indicated no relevant financial relationships.
Zaid Barbarawi indicated no relevant financial relationships.
Adriana R. Silva Marin indicated no relevant financial relationships.
Helen Mejia indicated no relevant financial relationships.
Mahmoud Barbarawi, MD1, Jathniel Panneflek, MD1, Majdi Salahie, MD2, Zaid Barbarawi, MD3, Adriana R. Silva Marin, MD4, Helen Mejia, MD5. P4908 - Endoscopic Management of Large Esophageal Mucosal Tears: A Systematic Review of Modern Closure Techniques and Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1DHR Health in affiliation with University of Houston, Tilman J. Fertitta College of Medicine, McAllen, TX; 2DHR Health, McAllen, TX; 3Jordan University of Science and Technology, McAllen, TX; 4Facultad de Medicina Alberto Hurtado, Universidad Peruana Cayetano Heredia, McAllen, TX; 5Antillean Adventist Hospital, Willemstad, TX
Introduction: Large esophageal mucosal tears are life-threatening injuries traditionally managed surgically, but endoscopic techniques have emerged as effective first-line therapies. However, optimal endoscopic modality selection and predictors of success remain unclear. This systematic review evaluates the efficacy of endoscopic closure methods and identifies key factors influencing clinical success.
Methods: Following PRISMA guidelines, we searched PubMed, Embase, and Scopus (2010-2024) for studies reporting endoscopic management of large esophageal tears/perforations. We excluded small Mallory-Weiss tears and included English-language studies of all designs. Primary outcome was clinical success (complete healing within 30 days without surgery). Secondary outcomes included technical success, complications, and mortality. Qualitative synthesis was performed with quantitative pooling where data permitted.
Results: From 412 records identified, 38 studies met inclusion criteria after removing duplicates and screening, encompassing esophageal tears from various etiologies (spontaneous ruptures, iatrogenic perforations). Over-the-scope clips (OTSC) were most used (approximately 75% of studies), followed by endoscopic suturing and covered self-expanding metal stents. Pooled clinical success rate was approximately 85% with moderate heterogeneity between studies. OTSC demonstrated high success rates (80-95%) for acute perforations when deployed promptly. Endoscopic suturing showed favorable immediate outcomes (~88%) though long-term durability was lower (55-60%). Key predictors of endoscopic failure included: defect size >20mm, delayed intervention beyond 24-48 hours, poor tissue quality, and ongoing distal obstruction. Iatrogenic perforations had better outcomes than spontaneous ruptures. Procedure-related complications were uncommon, with 10-15% requiring surgical salvage. Overall mortality was low (5-10%) and primarily related to perforation-related sepsis rather than endoscopic procedures.
Discussion: Endoscopic management is highly effective for appropriately selected large esophageal tears when performed promptly by experienced operators. Success depends critically on timing, defect characteristics, and technique selection. We propose an algorithmic approach: OTSC for defects 2-3cm, endoscopic suturing for 3-5cm tears, and covered stents when primary closure fails. These findings support endoscopic therapy as 1st-line treatment for large esophageal tears, potentially avoiding major surgical morbidity.
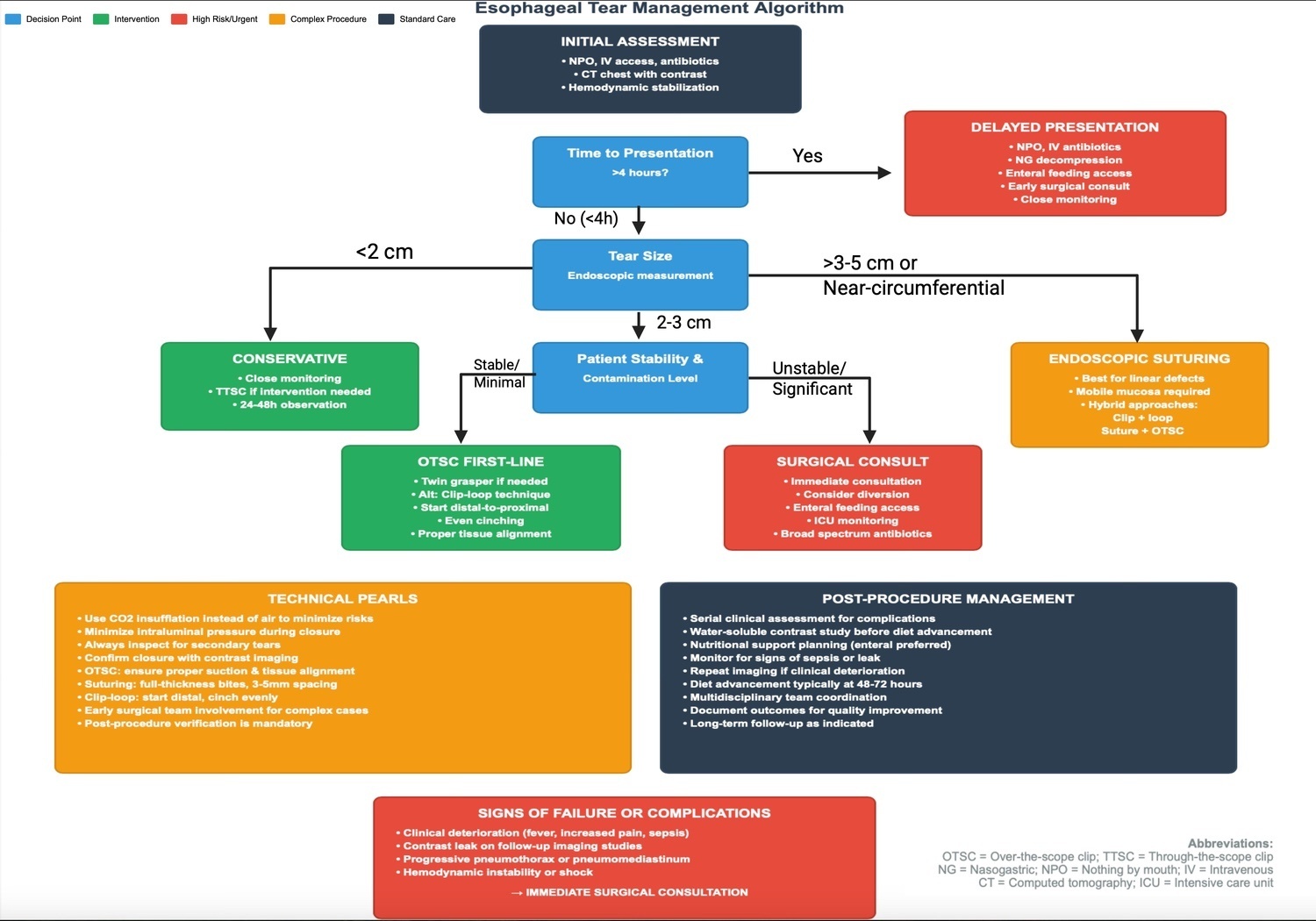
Figure: Figure 1: Proposed algorithm for endoscopic management of esophageal mucosal tears.
Decision-making is based on defect size, timing of presentation, and patient stability. OTSC is recommended for 2–3 cm tears, endoscopic suturing for 3–5 cm defects, and covered stents for failed primary closure or extensive injury. Early surgical consultation is advised for large, delayed, or complicated cases.

Figure: Figure 2: PRISMA flow diagram outlining the study selection process.
Depicts the number of records identified, screened, assessed for eligibility, and ultimately included in the systematic review on endoscopic management of large esophageal mucosal tears, with reasons for exclusion at each stage.
Tables with specifics can be provided upon request.
Disclosures:
Mahmoud Barbarawi indicated no relevant financial relationships.
Jathniel Panneflek indicated no relevant financial relationships.
Majdi Salahie indicated no relevant financial relationships.
Zaid Barbarawi indicated no relevant financial relationships.
Adriana R. Silva Marin indicated no relevant financial relationships.
Helen Mejia indicated no relevant financial relationships.
Mahmoud Barbarawi, MD1, Jathniel Panneflek, MD1, Majdi Salahie, MD2, Zaid Barbarawi, MD3, Adriana R. Silva Marin, MD4, Helen Mejia, MD5. P4908 - Endoscopic Management of Large Esophageal Mucosal Tears: A Systematic Review of Modern Closure Techniques and Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
