Tuesday Poster Session
Category: Esophagus
P4900 - A Systematic Review of Biomarkers and Non-Endoscopic Tissue Collection for EoE Diagnosis and Monitoring
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- HN
Hao The Nguyen
Rocky Vista University
waldorf, MD
Presenting Author(s)
Hao The Nguyen, 1, Shania Darville, 2, Arman Vaghefi, DO1, Michelle Hor, MD3
1Rocky Vista University, Colorado Springs, CO; 2University of South Florida, Tampa, FL; 3University of Colorado School of Medicine, Colorado Springs, CO
Introduction: Eosinophilic esophagitis (EoE) is an immune-mediated condition typically monitored via serial endoscopy with biopsies. Despite being the current standard, serial endoscopy is invasive, costly, and burdensome. Non-endoscopic biomarkers offer a potential alternative, but their diagnostic utility remains unclear. The objective of this study was to evaluate the diagnostic and disease monitoring performance of non-endoscopic biomarkers in adult EoE.
Methods: We conducted a systematic search of PubMed, Embase, and Cochrane Central from 2014 onward as part of a PROSPERO-registered review (CRD420251040649). This sub-analysis focused on adult patients. Inclusion criteria required original studies comparing non-endoscopic biomarkers to histologic or clinical outcomes in biopsy-confirmed EoE. Studies were excluded if pediatric-only or if age-specific data were not delineated. Two reviewers independently screened studies and extracted data on biomarker type, sample size, sensitivity, specificity, AUC, and risk of bias (QUADAS-2). Disagreements were resolved with a third reviewer.
Results: Sixteen out of 854 studies met inclusion, evaluating over 40 biomarkers from saliva, serum, breath, and minimally invasive esophageal sampling. Diagnostic performance varied. Eosinophil-derived neurotoxin (EDN) showed the most balanced accuracy (75.8% sensitivity, 73.3% specificity), while absolute eosinophil count (AEC) correlated more consistently with disease activity and treatment response (sensitivity up to 88%). Eosinophil cationic protein (ECP) and major basic protein (MBP) showed inconsistent results; fractional exhaled nitric oxide (FeNO) had poor reproducibility and wide variability. For sampling techniques, Cytosponge showed 75-84.6% sensitivity and 56-68% specificity; liquid-based cytology (LBC) showed 70% sensitivity and 81% specificity. Endoscopic biopsy achieved near-perfect sensitivity (up to 100%) and 96% specificity in reference studies. Meta-analysis and calculation of pooled data was not performed due to heterogeneity in studies, outcome definitions, and low study counts. Instead, findings were synthesized descriptively using a summary table and scatter plot.
Discussion: EDN, AEC, and Cytosponge sampling show potential as adjunctive tools for diagnosing or monitoring EoE. They may help guide triage and reduce reliance on endoscopy. However, findings were limited by heterogeneity, small sample sizes, and inconsistent performance. Further validation is necessary before clinical integration.
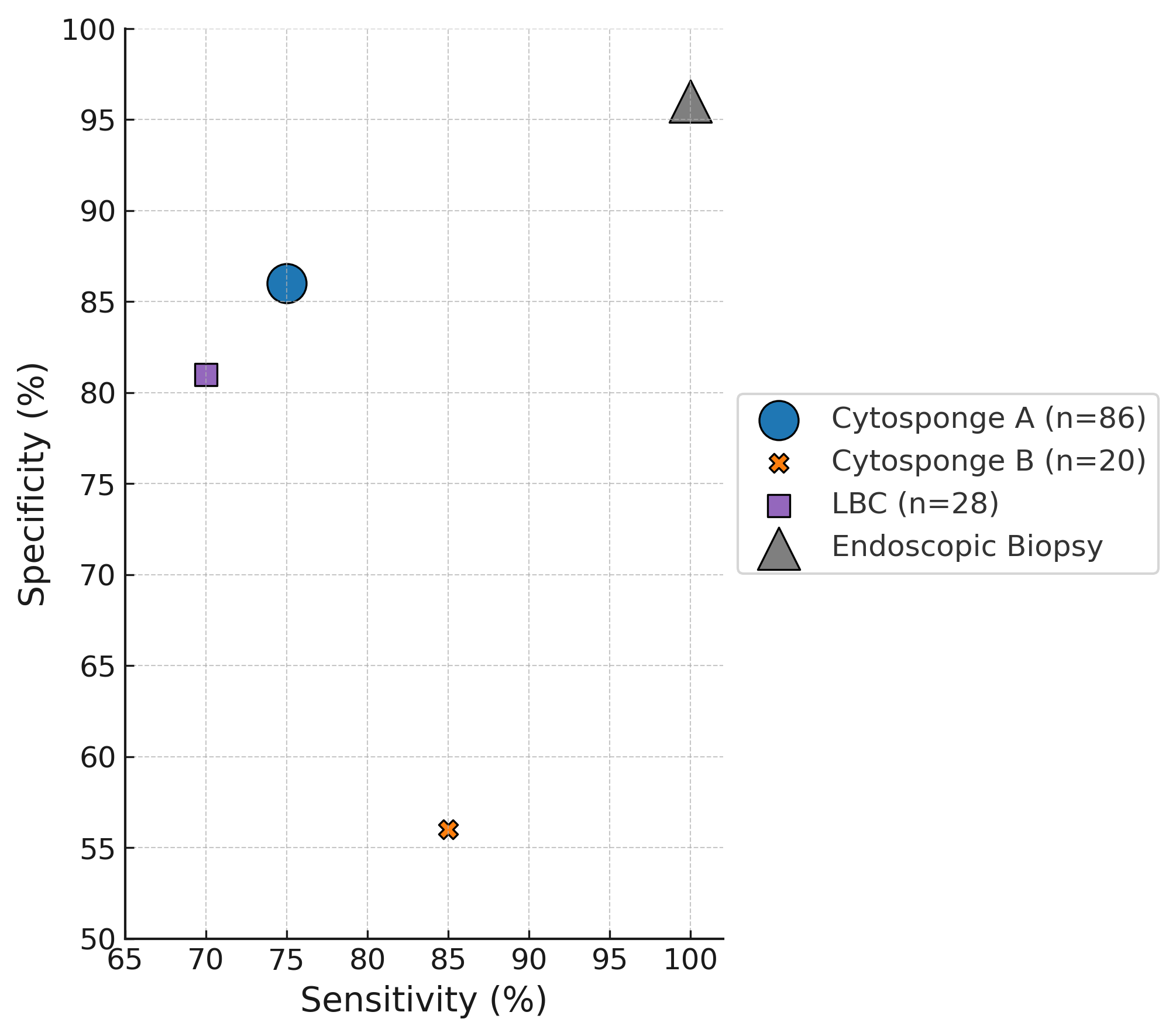
Figure: Diagnostic performance of Cytosponge and liquid-based cytology (LBC) compared to endoscopic biopsy. Bubble area scales to study n; shapes indicate modality
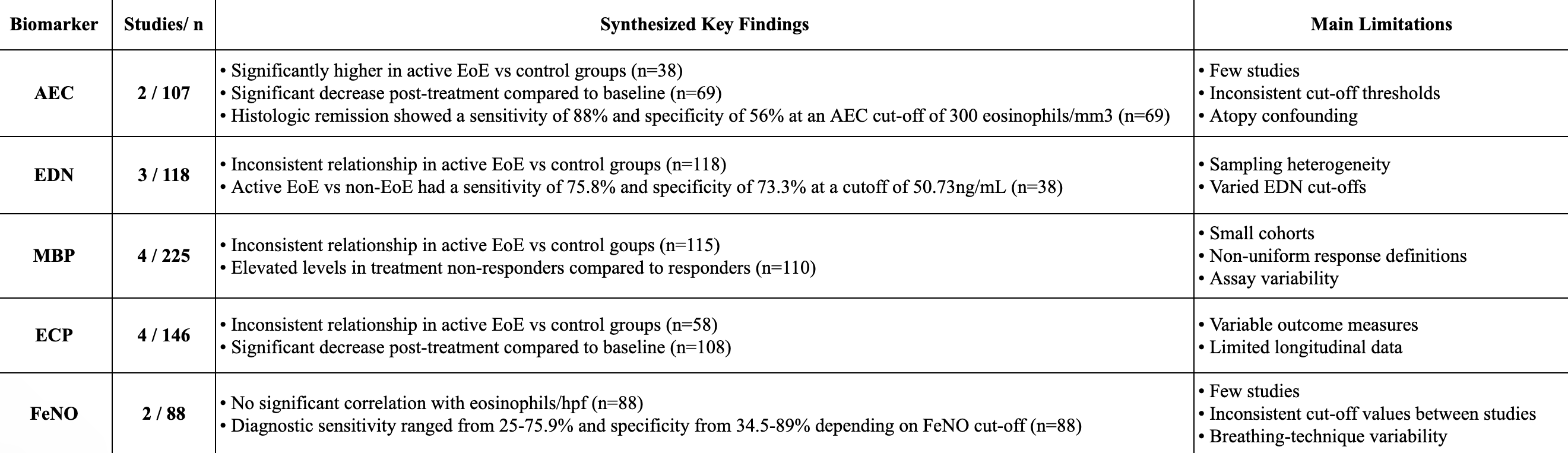
Figure: Synthesized findings from studies highlighting variability in diagnostic utility of biomarkers and key methodological limitations.
Disclosures:
Hao The Nguyen indicated no relevant financial relationships.
Shania Darville indicated no relevant financial relationships.
Arman Vaghefi indicated no relevant financial relationships.
Michelle Hor indicated no relevant financial relationships.
Hao The Nguyen, 1, Shania Darville, 2, Arman Vaghefi, DO1, Michelle Hor, MD3. P4900 - A Systematic Review of Biomarkers and Non-Endoscopic Tissue Collection for EoE Diagnosis and Monitoring, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Rocky Vista University, Colorado Springs, CO; 2University of South Florida, Tampa, FL; 3University of Colorado School of Medicine, Colorado Springs, CO
Introduction: Eosinophilic esophagitis (EoE) is an immune-mediated condition typically monitored via serial endoscopy with biopsies. Despite being the current standard, serial endoscopy is invasive, costly, and burdensome. Non-endoscopic biomarkers offer a potential alternative, but their diagnostic utility remains unclear. The objective of this study was to evaluate the diagnostic and disease monitoring performance of non-endoscopic biomarkers in adult EoE.
Methods: We conducted a systematic search of PubMed, Embase, and Cochrane Central from 2014 onward as part of a PROSPERO-registered review (CRD420251040649). This sub-analysis focused on adult patients. Inclusion criteria required original studies comparing non-endoscopic biomarkers to histologic or clinical outcomes in biopsy-confirmed EoE. Studies were excluded if pediatric-only or if age-specific data were not delineated. Two reviewers independently screened studies and extracted data on biomarker type, sample size, sensitivity, specificity, AUC, and risk of bias (QUADAS-2). Disagreements were resolved with a third reviewer.
Results: Sixteen out of 854 studies met inclusion, evaluating over 40 biomarkers from saliva, serum, breath, and minimally invasive esophageal sampling. Diagnostic performance varied. Eosinophil-derived neurotoxin (EDN) showed the most balanced accuracy (75.8% sensitivity, 73.3% specificity), while absolute eosinophil count (AEC) correlated more consistently with disease activity and treatment response (sensitivity up to 88%). Eosinophil cationic protein (ECP) and major basic protein (MBP) showed inconsistent results; fractional exhaled nitric oxide (FeNO) had poor reproducibility and wide variability. For sampling techniques, Cytosponge showed 75-84.6% sensitivity and 56-68% specificity; liquid-based cytology (LBC) showed 70% sensitivity and 81% specificity. Endoscopic biopsy achieved near-perfect sensitivity (up to 100%) and 96% specificity in reference studies. Meta-analysis and calculation of pooled data was not performed due to heterogeneity in studies, outcome definitions, and low study counts. Instead, findings were synthesized descriptively using a summary table and scatter plot.
Discussion: EDN, AEC, and Cytosponge sampling show potential as adjunctive tools for diagnosing or monitoring EoE. They may help guide triage and reduce reliance on endoscopy. However, findings were limited by heterogeneity, small sample sizes, and inconsistent performance. Further validation is necessary before clinical integration.
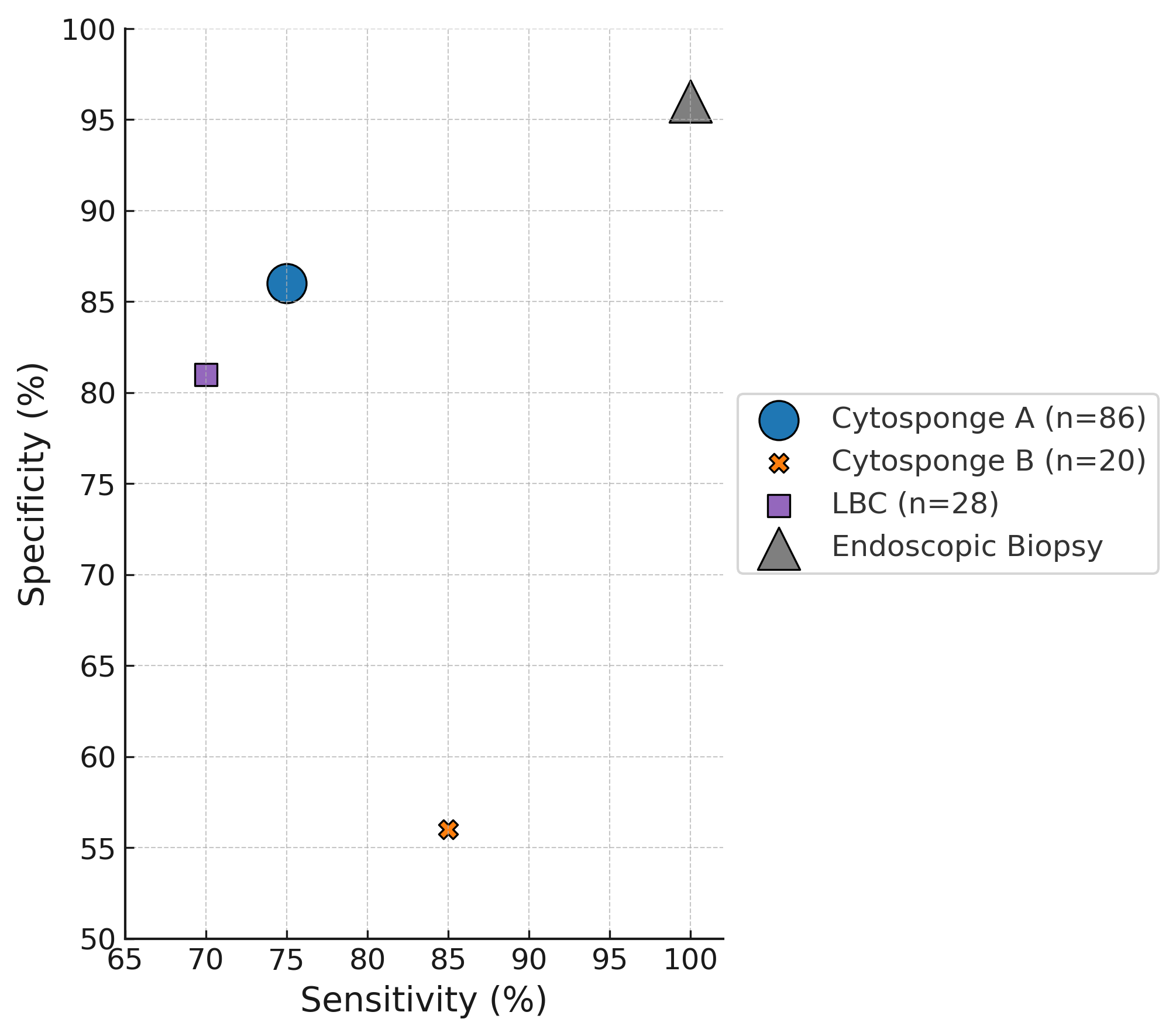
Figure: Diagnostic performance of Cytosponge and liquid-based cytology (LBC) compared to endoscopic biopsy. Bubble area scales to study n; shapes indicate modality
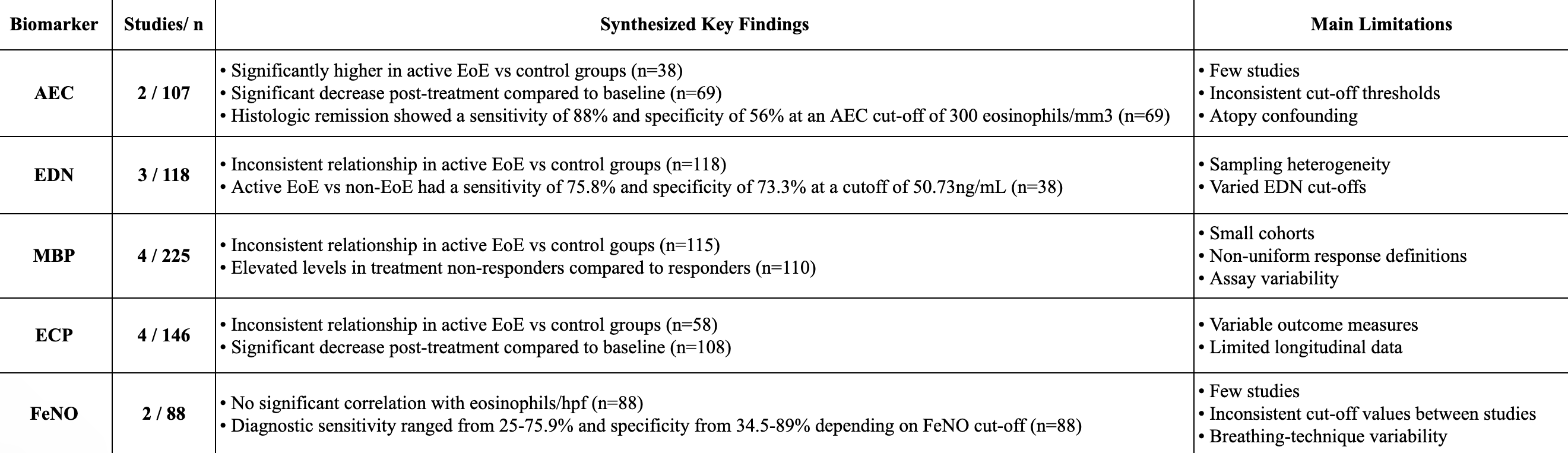
Figure: Synthesized findings from studies highlighting variability in diagnostic utility of biomarkers and key methodological limitations.
Disclosures:
Hao The Nguyen indicated no relevant financial relationships.
Shania Darville indicated no relevant financial relationships.
Arman Vaghefi indicated no relevant financial relationships.
Michelle Hor indicated no relevant financial relationships.
Hao The Nguyen, 1, Shania Darville, 2, Arman Vaghefi, DO1, Michelle Hor, MD3. P4900 - A Systematic Review of Biomarkers and Non-Endoscopic Tissue Collection for EoE Diagnosis and Monitoring, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
