Tuesday Poster Session
Category: Esophagus
P4897 - Breaking the 15-mm Barrier: Liberal Ring Sizing and Index 30-mm Balloon Dilation Minimize Post-Magnetic Sphincter Augmentation Dysphagia in a 10-Year Retrospective Cohort
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ifrah Fatima, MD
University of Missouri - Kansas City School of Medicine
Kansas City, MO
Presenting Author(s)
Award: ACG Presidential Poster Award
Ifrah Fatima, MD1, Mir Zulqarnain, DO1, Noor Hassan, MD2, Mohamed Ahmed, MD1, Abbas Bader, 1, Sruthi Sripada, 1, Pallavi Jonnalagadda, BSE3, Kensey Gosch, 1, Todd Moore, MD4, Sreeni Jonnalagadda, MD5
1University of Missouri - Kansas City School of Medicine, Kansas City, MO; 2Univeristy of MIssouri- Kansas City, Kansas City, MO; 3Washington University School of Medicine in St. Louis, Saint Louis, MO; 4University of Missouri Kansas City School of Medicine, Saint Luke's Hospital, Kansas City, MO; 5Saint Luke's Health System of Kansas City, Kansas City, MO
Introduction: Dysphagia is the most frequent early adverse event after magnetic sphincter augmentation (MSA) with the LINX® device. The package insert caps post-MSA dilation at 15 mm but it is unclear MSA size and index dilation diameter affects clinical outcomes. We analyzed retrospective data over 10 years to identify predictors of post-MSA dysphagia and compared initial 30 mm dilation (over the wire under fluoroscopic guidance) strategy vs conventional (< 20 mm dilation) through the scope (TTS).
Methods: Adults undergoing MSA for refractory GERD at a single tertiary center (Jan 2014-Jan 2025) were reviewed. Demographics, MSA size, and postoperative endoscopic dilations were recorded. Multivariable logistic regression identified independent risk factors for dilation. Outcomes after first-line 30 mm dilation (inflated to 8 PSI) were compared with < 20 mm TTS dilations. Primary endpoints: repeat dilation and device explantation. Secondary endpoints: complications and time to first dilation. Absolute risk reduction (ARR), number-needed-to-treat (NNT) were calculated.
Results: Of 304 MSA recipients (63% female, mean age 57 ± 14 y), 74 (24.3%) developed dysphagia requiring endoscopic dilation. Older age increased this risk (OR 1.16 per 5 y; 95 % CI 1.03-1.29; p=0.01), each increment in size of MSA reduced it (OR 0.73; 95% CI 0.56-0.98; p = 0.03). 44 patients underwent < 20 mm dilation and 30 underwent 30 mm dilation. Repeat dilation was required in 20/44 (45.5%) vs 9/30 (20%) respectively; ARR 25.5 %, NNT = 4. An initial 30 mm dilation independently lowered the repeat-dilation risk (OR 0.24; 95 % CI 0.07-0.91; p=0.03). Time to index dilation was longer in the 30 mm dilation group. (31.7 ± 24.2 vs 18.1 ± 14.4 months; p = 0.03). Device explantation occurred in 15 patients (4.9%), only 3 had received a 30 mm dilation. No perforations, erosions, or procedure-related hospitalizations were seen in either groups.
Discussion: In this 10-year retrospective cohort, larger MSA size was significantly associated with lower post-MSA dysphagia, and treating dysphagia with a single 30 mm dilation (as opposed to step up dilation per manufacturer’s recommendations) reduced the repeat-procedure rate by 76% without added morbidity (NNT = 4). Our data highlights two modifiable factors that can improve long-term dysphagia outcomes. Prospective multicenter data from physiologic manometric studies (such as EsoFLIP) are needed to validate these findings and refine protocols for endoscopic therapy in post-MSA dysphagia.
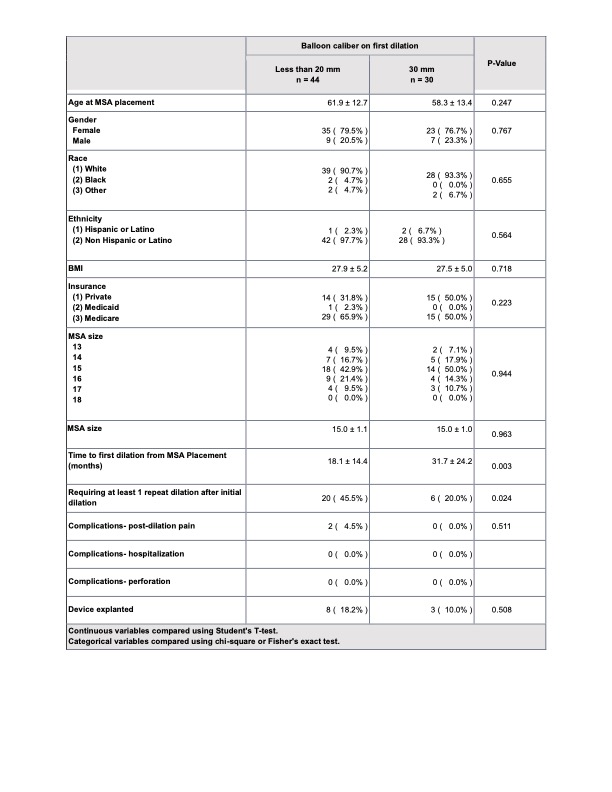
Figure: Table 1- Baseline characteristics of patients undergoing dilations with balloon size < 20mm vs 30mm

Figure: Table 2- Predictors associated with more than one dilation after first esophageal dilation.
Disclosures:
Ifrah Fatima indicated no relevant financial relationships.
Mir Zulqarnain indicated no relevant financial relationships.
Noor Hassan indicated no relevant financial relationships.
Mohamed Ahmed indicated no relevant financial relationships.
Abbas Bader indicated no relevant financial relationships.
Sruthi Sripada indicated no relevant financial relationships.
Pallavi Jonnalagadda indicated no relevant financial relationships.
Kensey Gosch indicated no relevant financial relationships.
Todd Moore indicated no relevant financial relationships.
Sreeni Jonnalagadda indicated no relevant financial relationships.
Ifrah Fatima, MD1, Mir Zulqarnain, DO1, Noor Hassan, MD2, Mohamed Ahmed, MD1, Abbas Bader, 1, Sruthi Sripada, 1, Pallavi Jonnalagadda, BSE3, Kensey Gosch, 1, Todd Moore, MD4, Sreeni Jonnalagadda, MD5. P4897 - Breaking the 15-mm Barrier: Liberal Ring Sizing and Index 30-mm Balloon Dilation Minimize Post-Magnetic Sphincter Augmentation Dysphagia in a 10-Year Retrospective Cohort, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Ifrah Fatima, MD1, Mir Zulqarnain, DO1, Noor Hassan, MD2, Mohamed Ahmed, MD1, Abbas Bader, 1, Sruthi Sripada, 1, Pallavi Jonnalagadda, BSE3, Kensey Gosch, 1, Todd Moore, MD4, Sreeni Jonnalagadda, MD5
1University of Missouri - Kansas City School of Medicine, Kansas City, MO; 2Univeristy of MIssouri- Kansas City, Kansas City, MO; 3Washington University School of Medicine in St. Louis, Saint Louis, MO; 4University of Missouri Kansas City School of Medicine, Saint Luke's Hospital, Kansas City, MO; 5Saint Luke's Health System of Kansas City, Kansas City, MO
Introduction: Dysphagia is the most frequent early adverse event after magnetic sphincter augmentation (MSA) with the LINX® device. The package insert caps post-MSA dilation at 15 mm but it is unclear MSA size and index dilation diameter affects clinical outcomes. We analyzed retrospective data over 10 years to identify predictors of post-MSA dysphagia and compared initial 30 mm dilation (over the wire under fluoroscopic guidance) strategy vs conventional (< 20 mm dilation) through the scope (TTS).
Methods: Adults undergoing MSA for refractory GERD at a single tertiary center (Jan 2014-Jan 2025) were reviewed. Demographics, MSA size, and postoperative endoscopic dilations were recorded. Multivariable logistic regression identified independent risk factors for dilation. Outcomes after first-line 30 mm dilation (inflated to 8 PSI) were compared with < 20 mm TTS dilations. Primary endpoints: repeat dilation and device explantation. Secondary endpoints: complications and time to first dilation. Absolute risk reduction (ARR), number-needed-to-treat (NNT) were calculated.
Results: Of 304 MSA recipients (63% female, mean age 57 ± 14 y), 74 (24.3%) developed dysphagia requiring endoscopic dilation. Older age increased this risk (OR 1.16 per 5 y; 95 % CI 1.03-1.29; p=0.01), each increment in size of MSA reduced it (OR 0.73; 95% CI 0.56-0.98; p = 0.03). 44 patients underwent < 20 mm dilation and 30 underwent 30 mm dilation. Repeat dilation was required in 20/44 (45.5%) vs 9/30 (20%) respectively; ARR 25.5 %, NNT = 4. An initial 30 mm dilation independently lowered the repeat-dilation risk (OR 0.24; 95 % CI 0.07-0.91; p=0.03). Time to index dilation was longer in the 30 mm dilation group. (31.7 ± 24.2 vs 18.1 ± 14.4 months; p = 0.03). Device explantation occurred in 15 patients (4.9%), only 3 had received a 30 mm dilation. No perforations, erosions, or procedure-related hospitalizations were seen in either groups.
Discussion: In this 10-year retrospective cohort, larger MSA size was significantly associated with lower post-MSA dysphagia, and treating dysphagia with a single 30 mm dilation (as opposed to step up dilation per manufacturer’s recommendations) reduced the repeat-procedure rate by 76% without added morbidity (NNT = 4). Our data highlights two modifiable factors that can improve long-term dysphagia outcomes. Prospective multicenter data from physiologic manometric studies (such as EsoFLIP) are needed to validate these findings and refine protocols for endoscopic therapy in post-MSA dysphagia.
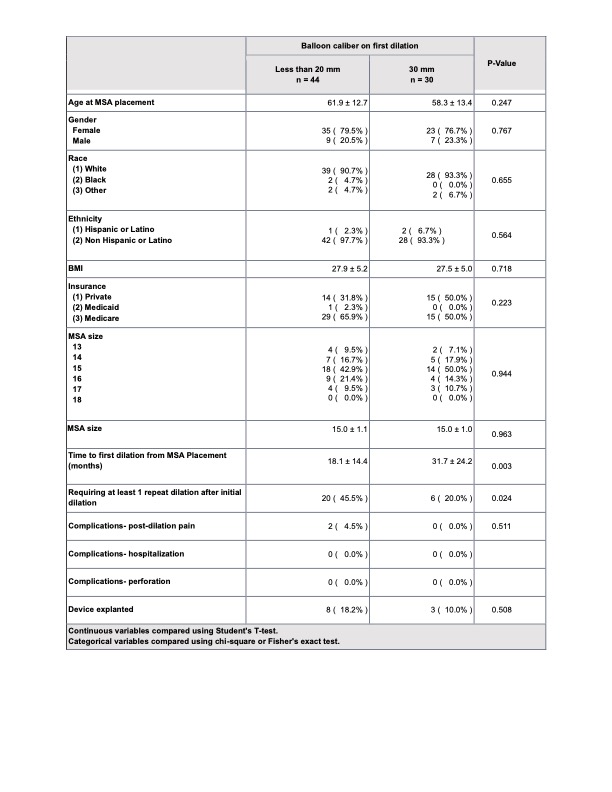
Figure: Table 1- Baseline characteristics of patients undergoing dilations with balloon size < 20mm vs 30mm

Figure: Table 2- Predictors associated with more than one dilation after first esophageal dilation.
Disclosures:
Ifrah Fatima indicated no relevant financial relationships.
Mir Zulqarnain indicated no relevant financial relationships.
Noor Hassan indicated no relevant financial relationships.
Mohamed Ahmed indicated no relevant financial relationships.
Abbas Bader indicated no relevant financial relationships.
Sruthi Sripada indicated no relevant financial relationships.
Pallavi Jonnalagadda indicated no relevant financial relationships.
Kensey Gosch indicated no relevant financial relationships.
Todd Moore indicated no relevant financial relationships.
Sreeni Jonnalagadda indicated no relevant financial relationships.
Ifrah Fatima, MD1, Mir Zulqarnain, DO1, Noor Hassan, MD2, Mohamed Ahmed, MD1, Abbas Bader, 1, Sruthi Sripada, 1, Pallavi Jonnalagadda, BSE3, Kensey Gosch, 1, Todd Moore, MD4, Sreeni Jonnalagadda, MD5. P4897 - Breaking the 15-mm Barrier: Liberal Ring Sizing and Index 30-mm Balloon Dilation Minimize Post-Magnetic Sphincter Augmentation Dysphagia in a 10-Year Retrospective Cohort, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

