Tuesday Poster Session
Category: Diet, Nutrition, and Obesity
P4845 - Long-Term Weight Loss After Endoscopic Sleeve Gastroplasty: The Role of Clinical Follow-Up and Lifestyle Engagement
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- WG
Wissam Ghusn, MD
Boston Medical Center
Boston, MA
Presenting Author(s)
Wissam Ghusn, MD1, Yara Salameh, MD2, Maria Antonia Espinosa, MD3, Jose Villamarin, MD3, Karim Al Annan, MD4, Lea Sayegh, MD5, Kamal Abi Mosleh, MD3, Donna Maria Abboud, MD6, Khushboo Gala, MBBS3, Eric J.. Vargas, MD, MS3, Andrew Storm, MD3
1Boston Medical Center, Boston, MA; 2Mayo Foundation for Medical Education and Research, Rochester, MN; 3Mayo Clinic, Rochester, MN; 4University of Connecticut Health Center, Hartford, CT; 5Yale New Haven Hospital, New Haven, CT; 6Mount Sinai Medical Center, Miami, FL
Introduction: Endoscopic sleeve gastroplasty (ESG) is a minimally invasive bariatric procedure that induces meaningful weight loss in individuals with obesity. Long-term success, however, may depend on sustained behavioral and clinical support. Despite growing utilization, limited data exist on how follow-up intensity and lifestyle interventions impact long-term weight outcomes. This study aimed to evaluate the effects of close clinical follow-up and exercise participation on total body weight loss (TBWL) up to 3 years after ESG.
Methods: We conducted a retrospective cohort study of adults who underwent ESG at a tertiary academic center. Patients with less than 2 years of follow-up were excluded. The cohort was divided into two groups based on the number of post-procedure clinical visits: ≥5 visits versus < 5 visits. Demographic, clinical, and behavioral data, including participation in a structured exercise regimen, were extracted from the electronic health record. The primary aim was to assess the association between TBWL and clinical follow-up frequency. The secondary aim was to evaluate whether exercise engagement contributed to greater TBWL. Between-group comparisons were performed using t-tests and chi-square tests.
Results: Seventy-seven patients met inclusion criteria (mean age 49.6 ± 11.3 years; 81.8% female; 89.6% White) with a follow up period of 29.0 ± 6.0 months. No significant differences in baseline demographics, comorbidities or follow-up periods were observed between groups (Table 1). Patients with ≥5 follow-up visits (n = 35) achieved significantly greater TBWL (−13.7 ± 11.2%) compared to those with < 5 visits (n = 21; −6.7 ± 8.2%; p = 0.01; Figure 1A). Categorical weight loss is presented in Figure 1B. Exercise participation was reported in 69.7% of the cohort. Those who reported engaging in exercise had slightly greater TBWL (−11.0 ± 11.4%) than non-exercisers (−9.3 ± 10.8%), although this difference was not statistically significant (p = 0.55; Figure 1C).
Discussion: In this real-world cohort of ESG patients followed for 2 or more years, close clinical follow-up was associated with significantly greater weight loss. Exercise participation was also linked to improved TBWL, though not statistically significant. These findings emphasize the importance of structured, long-term multidisciplinary care in optimizing ESG outcomes and suggest that close follow-up should be a cornerstone of post-ESG management strategies.
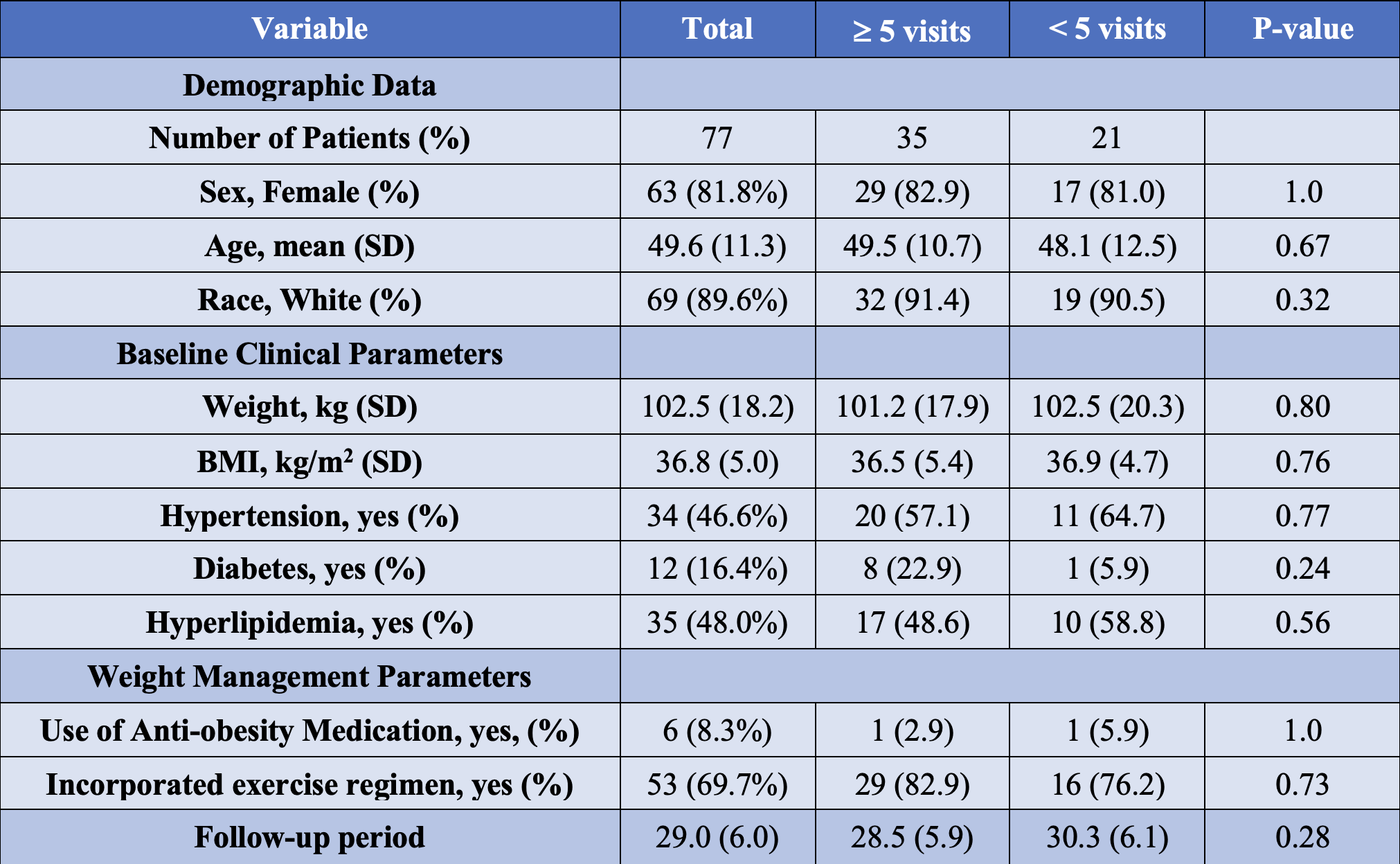
Figure: Table 1: Baseline demographic, clinical, and behavioral characteristics stratified by follow-up visit frequency in a weight management cohort.
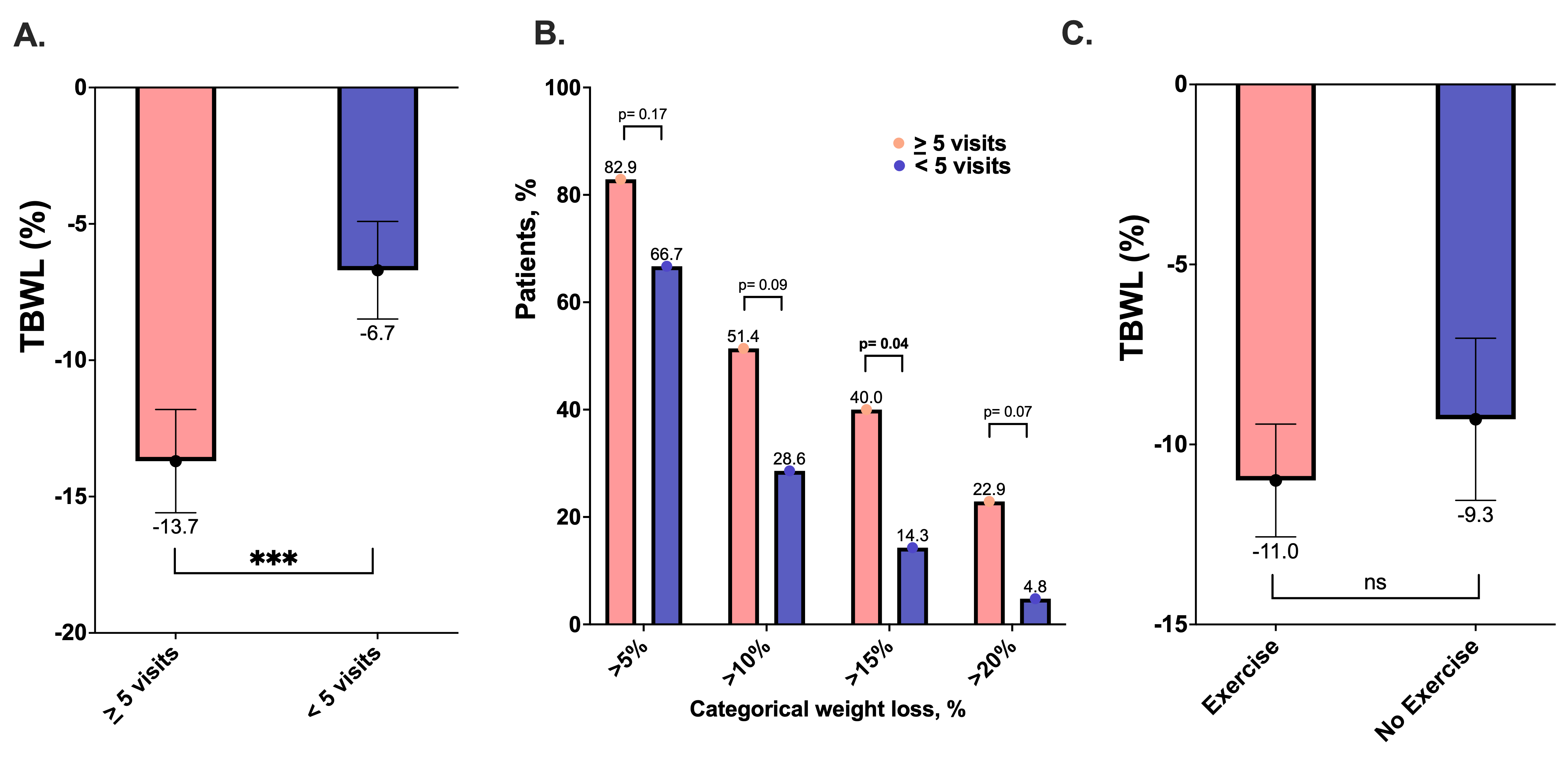
Figure: Figure 1: TBWL% (A) and categorical weight loss % (B) in patient with > 5 vs <5 clinic visits, and with vs without exercise regimen (C). (***: p<0.01; ns: Non-significant)
Disclosures:
Wissam Ghusn indicated no relevant financial relationships.
Yara Salameh indicated no relevant financial relationships.
Maria Antonia Espinosa indicated no relevant financial relationships.
Jose Villamarin indicated no relevant financial relationships.
Karim Al Annan indicated no relevant financial relationships.
Lea Sayegh indicated no relevant financial relationships.
Kamal Abi Mosleh indicated no relevant financial relationships.
Donna Maria Abboud indicated no relevant financial relationships.
Khushboo Gala indicated no relevant financial relationships.
Eric Vargas indicated no relevant financial relationships.
Andrew Storm: Ambu – Consultant. Apollo Endosurgery – Consultant, Grant/Research Support. Boston Scientific – Consultant, Grant/Research Support. Cook – Consultant. Endogenex – Grant/Research Support. Endo-Tagss – Grant/Research Support. Enterasense – Grant/Research Support. Envision Endoscopy – Grant/Research Support. Intuitive – Consultant. Medtronic – Consultant. MGI Medical – Grant/Research Support. Microtech – Consultant. Olympus – Consultant. OnePass – Grant/Research Support. SofTac – Grant/Research Support. Sotelix – Consultant. Steris – Consultant.
Wissam Ghusn, MD1, Yara Salameh, MD2, Maria Antonia Espinosa, MD3, Jose Villamarin, MD3, Karim Al Annan, MD4, Lea Sayegh, MD5, Kamal Abi Mosleh, MD3, Donna Maria Abboud, MD6, Khushboo Gala, MBBS3, Eric J.. Vargas, MD, MS3, Andrew Storm, MD3. P4845 - Long-Term Weight Loss After Endoscopic Sleeve Gastroplasty: The Role of Clinical Follow-Up and Lifestyle Engagement, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Boston Medical Center, Boston, MA; 2Mayo Foundation for Medical Education and Research, Rochester, MN; 3Mayo Clinic, Rochester, MN; 4University of Connecticut Health Center, Hartford, CT; 5Yale New Haven Hospital, New Haven, CT; 6Mount Sinai Medical Center, Miami, FL
Introduction: Endoscopic sleeve gastroplasty (ESG) is a minimally invasive bariatric procedure that induces meaningful weight loss in individuals with obesity. Long-term success, however, may depend on sustained behavioral and clinical support. Despite growing utilization, limited data exist on how follow-up intensity and lifestyle interventions impact long-term weight outcomes. This study aimed to evaluate the effects of close clinical follow-up and exercise participation on total body weight loss (TBWL) up to 3 years after ESG.
Methods: We conducted a retrospective cohort study of adults who underwent ESG at a tertiary academic center. Patients with less than 2 years of follow-up were excluded. The cohort was divided into two groups based on the number of post-procedure clinical visits: ≥5 visits versus < 5 visits. Demographic, clinical, and behavioral data, including participation in a structured exercise regimen, were extracted from the electronic health record. The primary aim was to assess the association between TBWL and clinical follow-up frequency. The secondary aim was to evaluate whether exercise engagement contributed to greater TBWL. Between-group comparisons were performed using t-tests and chi-square tests.
Results: Seventy-seven patients met inclusion criteria (mean age 49.6 ± 11.3 years; 81.8% female; 89.6% White) with a follow up period of 29.0 ± 6.0 months. No significant differences in baseline demographics, comorbidities or follow-up periods were observed between groups (Table 1). Patients with ≥5 follow-up visits (n = 35) achieved significantly greater TBWL (−13.7 ± 11.2%) compared to those with < 5 visits (n = 21; −6.7 ± 8.2%; p = 0.01; Figure 1A). Categorical weight loss is presented in Figure 1B. Exercise participation was reported in 69.7% of the cohort. Those who reported engaging in exercise had slightly greater TBWL (−11.0 ± 11.4%) than non-exercisers (−9.3 ± 10.8%), although this difference was not statistically significant (p = 0.55; Figure 1C).
Discussion: In this real-world cohort of ESG patients followed for 2 or more years, close clinical follow-up was associated with significantly greater weight loss. Exercise participation was also linked to improved TBWL, though not statistically significant. These findings emphasize the importance of structured, long-term multidisciplinary care in optimizing ESG outcomes and suggest that close follow-up should be a cornerstone of post-ESG management strategies.
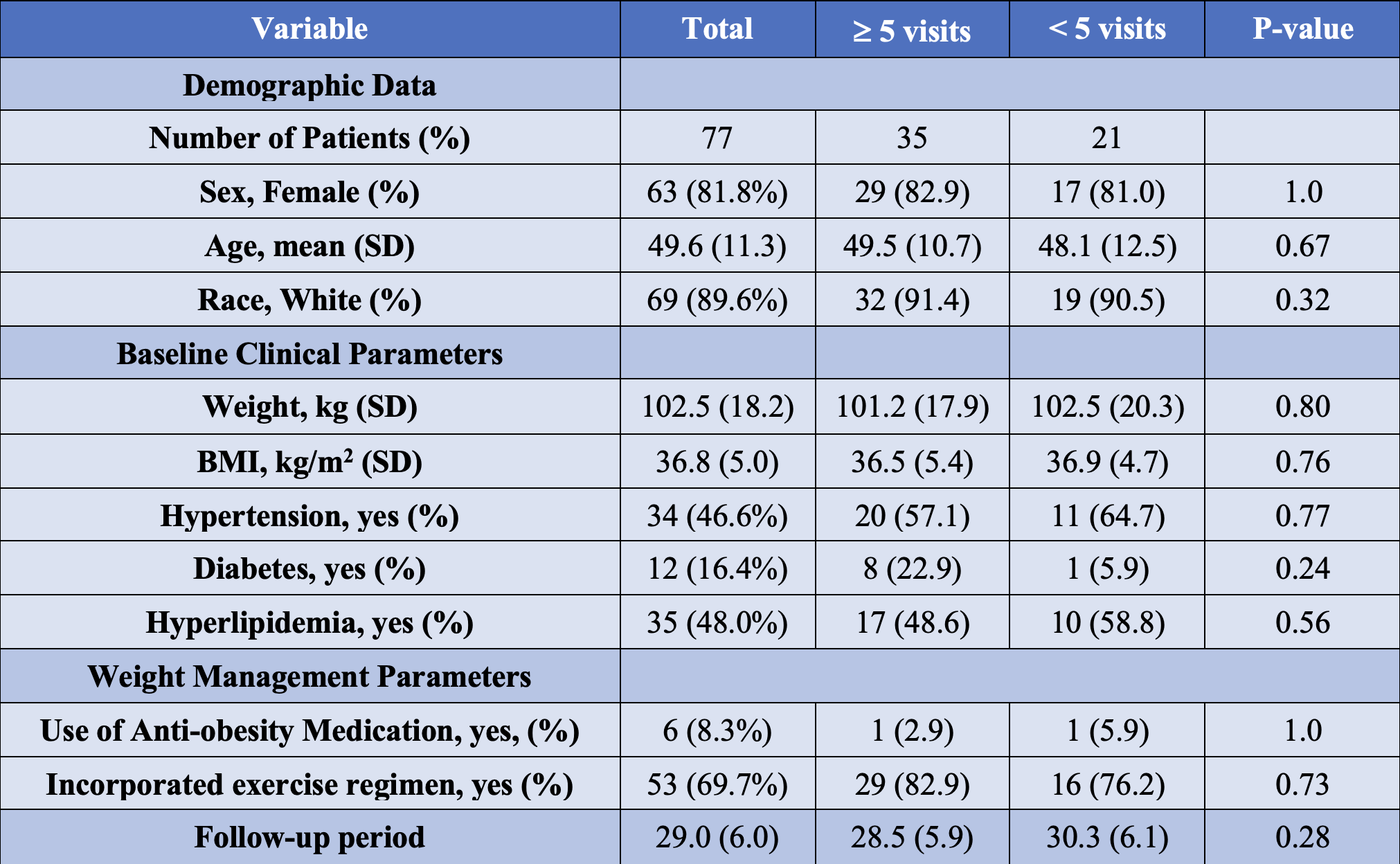
Figure: Table 1: Baseline demographic, clinical, and behavioral characteristics stratified by follow-up visit frequency in a weight management cohort.
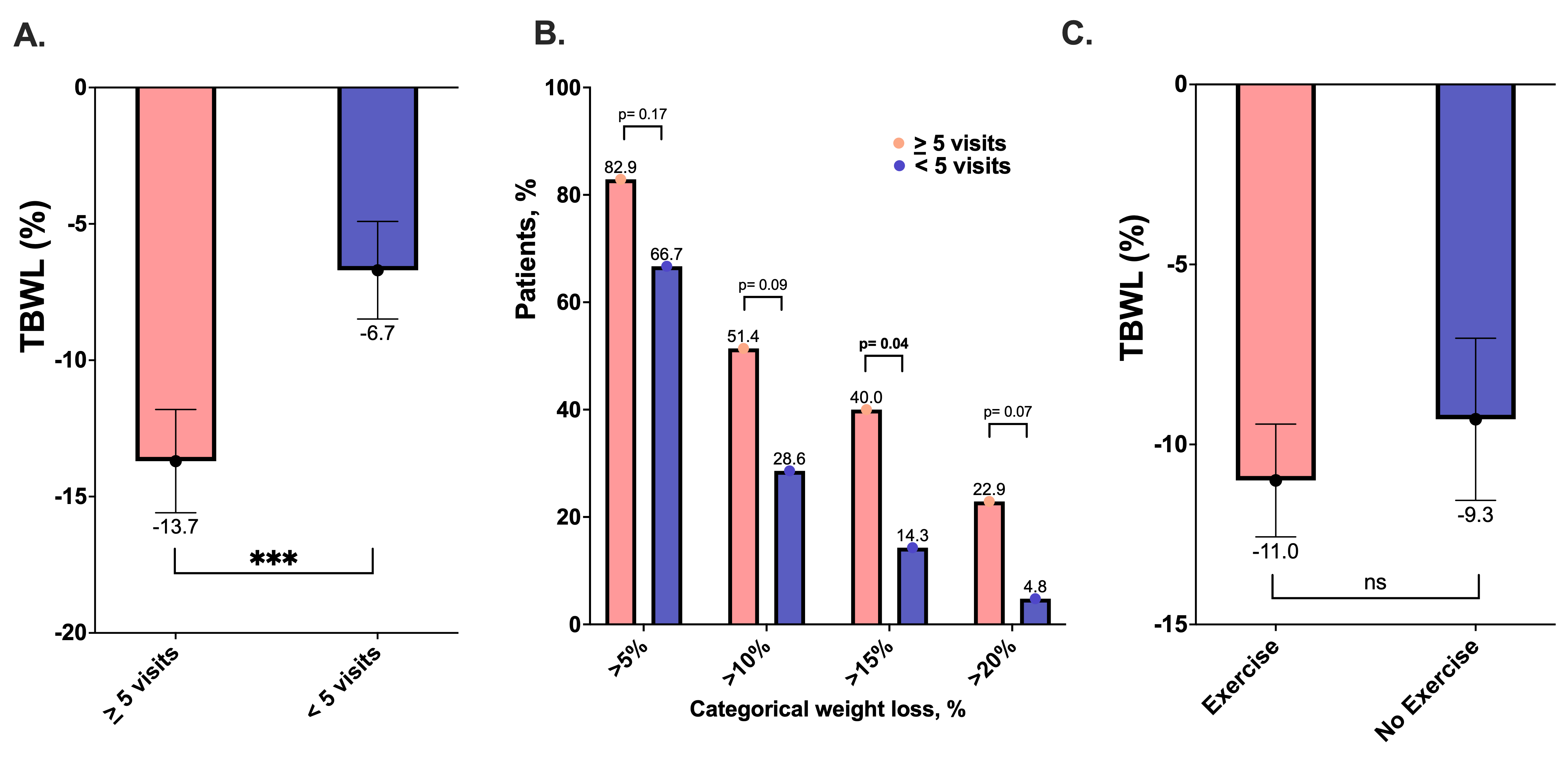
Figure: Figure 1: TBWL% (A) and categorical weight loss % (B) in patient with > 5 vs <5 clinic visits, and with vs without exercise regimen (C). (***: p<0.01; ns: Non-significant)
Disclosures:
Wissam Ghusn indicated no relevant financial relationships.
Yara Salameh indicated no relevant financial relationships.
Maria Antonia Espinosa indicated no relevant financial relationships.
Jose Villamarin indicated no relevant financial relationships.
Karim Al Annan indicated no relevant financial relationships.
Lea Sayegh indicated no relevant financial relationships.
Kamal Abi Mosleh indicated no relevant financial relationships.
Donna Maria Abboud indicated no relevant financial relationships.
Khushboo Gala indicated no relevant financial relationships.
Eric Vargas indicated no relevant financial relationships.
Andrew Storm: Ambu – Consultant. Apollo Endosurgery – Consultant, Grant/Research Support. Boston Scientific – Consultant, Grant/Research Support. Cook – Consultant. Endogenex – Grant/Research Support. Endo-Tagss – Grant/Research Support. Enterasense – Grant/Research Support. Envision Endoscopy – Grant/Research Support. Intuitive – Consultant. Medtronic – Consultant. MGI Medical – Grant/Research Support. Microtech – Consultant. Olympus – Consultant. OnePass – Grant/Research Support. SofTac – Grant/Research Support. Sotelix – Consultant. Steris – Consultant.
Wissam Ghusn, MD1, Yara Salameh, MD2, Maria Antonia Espinosa, MD3, Jose Villamarin, MD3, Karim Al Annan, MD4, Lea Sayegh, MD5, Kamal Abi Mosleh, MD3, Donna Maria Abboud, MD6, Khushboo Gala, MBBS3, Eric J.. Vargas, MD, MS3, Andrew Storm, MD3. P4845 - Long-Term Weight Loss After Endoscopic Sleeve Gastroplasty: The Role of Clinical Follow-Up and Lifestyle Engagement, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
