Tuesday Poster Session
Category: Diet, Nutrition, and Obesity
P4834 - Impact of Obstructive Sleep Apnea Among Morbidly Obese Adults Undergoing Elective Laparoscopic Sleeve Gastrectomy in the United States
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- RV
Renuka Verma, MD (she/her/hers)
Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas
Las Vegas, NV
Presenting Author(s)
Renuka Verma, MD1, Kristie Liao, DO2, Kamleshun Ramphul, MD3, Vignan Manne, MD1
1Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV; 2University of Tennessee Health Science Center, Chattanooga, TN; 3Independent researcher, Las Vegas, NV
Introduction: Laparoscopic sleeve gastrectomy(LSG), a minimally invasive procedure aimed at improving weight, has gained prominence among morbidly obese patients due to its safety profile and long-term effectiveness. While obstructive sleep apnea(OSA) is a common comorbidity prevalent among morbidly obese adults, data exploring its impact on short-term perioperative LSG outcomes remains understudied.
Methods: Pre-tested ICD-10 codes and methodologies(inclusions and exclusions) were applied to identify morbidly obese adults who underwent elective LSG via the National Inpatient Sample(2016-2022). Our sample was divided into OSA and non-OSA patients, and we compared their demographics and complications. We then evaluated the impact of age, sex, comorbidity burden, hospital status, race, and payer form on the composite adverse events among our OSA patients.
Results: We identified 630325 procedures performed between 2016 and 2022, with 35.4%(223185) OSA patients. Although both cohorts mainly were females, a higher proportion of males were seen in the OSA group. Additional differences were noted as OSA patients were older, with a higher prevalence of dyslipidemia, smokers, diabetes, chronic kidney disease, COPD, hypertension, and liver cirrhosis(Table 1a). Around 1.3% of both groups had a history of prior bariatric surgery. OSA was associated with higher odds of acute respiratory failure(ARF), aspiration pneumonia, need for vasopressors, acute kidney injury(AKI), bleeding/transfusion use, deep vein thrombosis (DVT)/thromboembolism, generalized abdominal pain, postprocedural intestinal obstruction, and all-cause mortality(Table 1b). Major adverse cardiac and cerebrovascular events (MACCE) and generalized acute peritonitis were comparable. In addition, the inflation-adjusted hospital charges were higher among patients with OSA($59869 vs. $59144, p< 0.01). Composite adverse events among OSA patients were less likely among females(vs. males), private insurance(vs. Medicare), rural centers (vs. urban teaching and non-teaching), and Hispanics(vs. Whites), but with higher odds among Blacks(vs. Whites), and with increasing age and comorbidity burden(Charlson Comorbidity Index score)(Table 1c).
Discussion: OSA significantly impacts LSG outcomes. These findings support the use of comprehensive preoperative screening and tailored perioperative management in this patient subset.
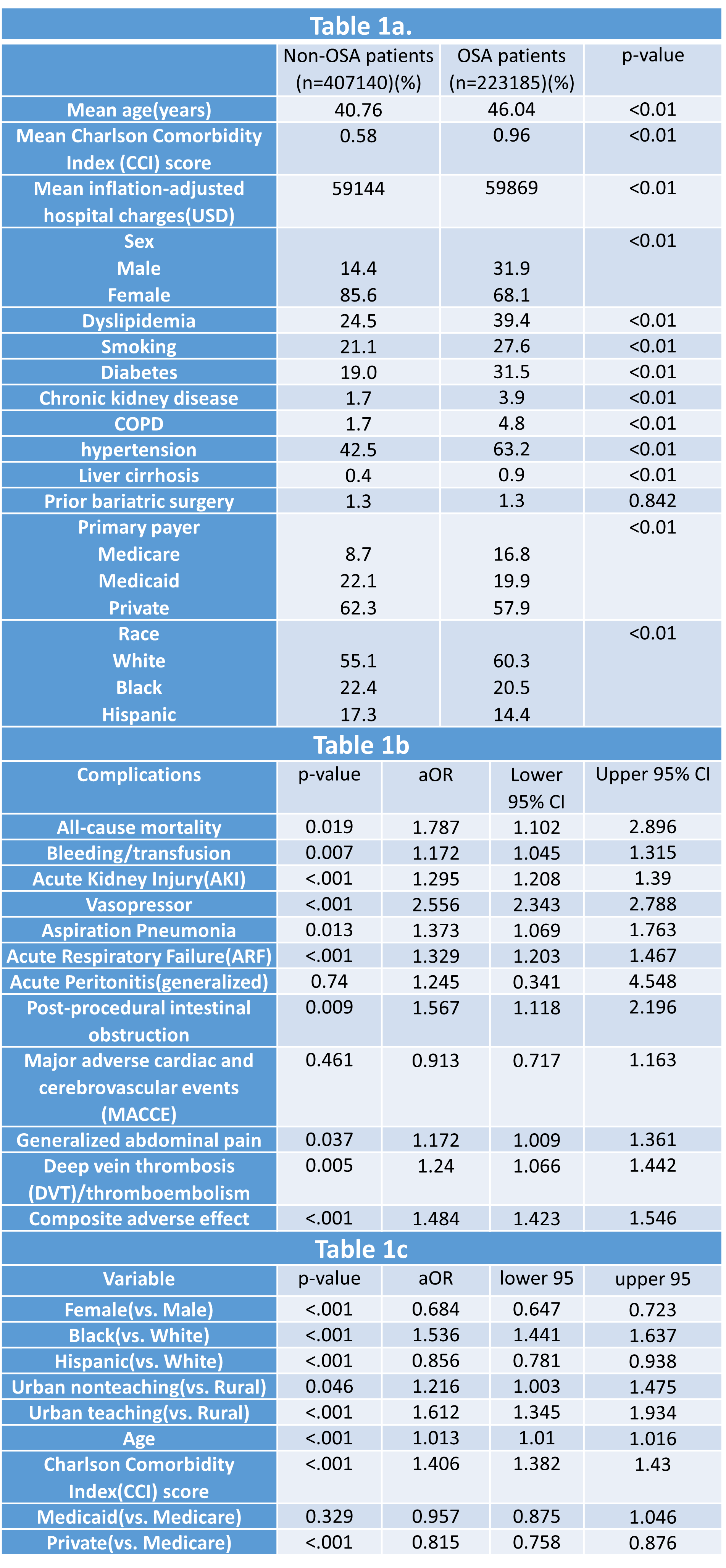
Figure: Table 1a- Baseline demographics and comorbidities among OSA vs non-OSA cases
Table 1b - Adverse events seen in OSA patients (Vs non-OSA as reference)
Table 1c- Variables including composite adverse events among OSA patients
Disclosures:
Renuka Verma indicated no relevant financial relationships.
Kristie Liao indicated no relevant financial relationships.
Kamleshun Ramphul indicated no relevant financial relationships.
Vignan Manne indicated no relevant financial relationships.
Renuka Verma, MD1, Kristie Liao, DO2, Kamleshun Ramphul, MD3, Vignan Manne, MD1. P4834 - Impact of Obstructive Sleep Apnea Among Morbidly Obese Adults Undergoing Elective Laparoscopic Sleeve Gastrectomy in the United States, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV; 2University of Tennessee Health Science Center, Chattanooga, TN; 3Independent researcher, Las Vegas, NV
Introduction: Laparoscopic sleeve gastrectomy(LSG), a minimally invasive procedure aimed at improving weight, has gained prominence among morbidly obese patients due to its safety profile and long-term effectiveness. While obstructive sleep apnea(OSA) is a common comorbidity prevalent among morbidly obese adults, data exploring its impact on short-term perioperative LSG outcomes remains understudied.
Methods: Pre-tested ICD-10 codes and methodologies(inclusions and exclusions) were applied to identify morbidly obese adults who underwent elective LSG via the National Inpatient Sample(2016-2022). Our sample was divided into OSA and non-OSA patients, and we compared their demographics and complications. We then evaluated the impact of age, sex, comorbidity burden, hospital status, race, and payer form on the composite adverse events among our OSA patients.
Results: We identified 630325 procedures performed between 2016 and 2022, with 35.4%(223185) OSA patients. Although both cohorts mainly were females, a higher proportion of males were seen in the OSA group. Additional differences were noted as OSA patients were older, with a higher prevalence of dyslipidemia, smokers, diabetes, chronic kidney disease, COPD, hypertension, and liver cirrhosis(Table 1a). Around 1.3% of both groups had a history of prior bariatric surgery. OSA was associated with higher odds of acute respiratory failure(ARF), aspiration pneumonia, need for vasopressors, acute kidney injury(AKI), bleeding/transfusion use, deep vein thrombosis (DVT)/thromboembolism, generalized abdominal pain, postprocedural intestinal obstruction, and all-cause mortality(Table 1b). Major adverse cardiac and cerebrovascular events (MACCE) and generalized acute peritonitis were comparable. In addition, the inflation-adjusted hospital charges were higher among patients with OSA($59869 vs. $59144, p< 0.01). Composite adverse events among OSA patients were less likely among females(vs. males), private insurance(vs. Medicare), rural centers (vs. urban teaching and non-teaching), and Hispanics(vs. Whites), but with higher odds among Blacks(vs. Whites), and with increasing age and comorbidity burden(Charlson Comorbidity Index score)(Table 1c).
Discussion: OSA significantly impacts LSG outcomes. These findings support the use of comprehensive preoperative screening and tailored perioperative management in this patient subset.
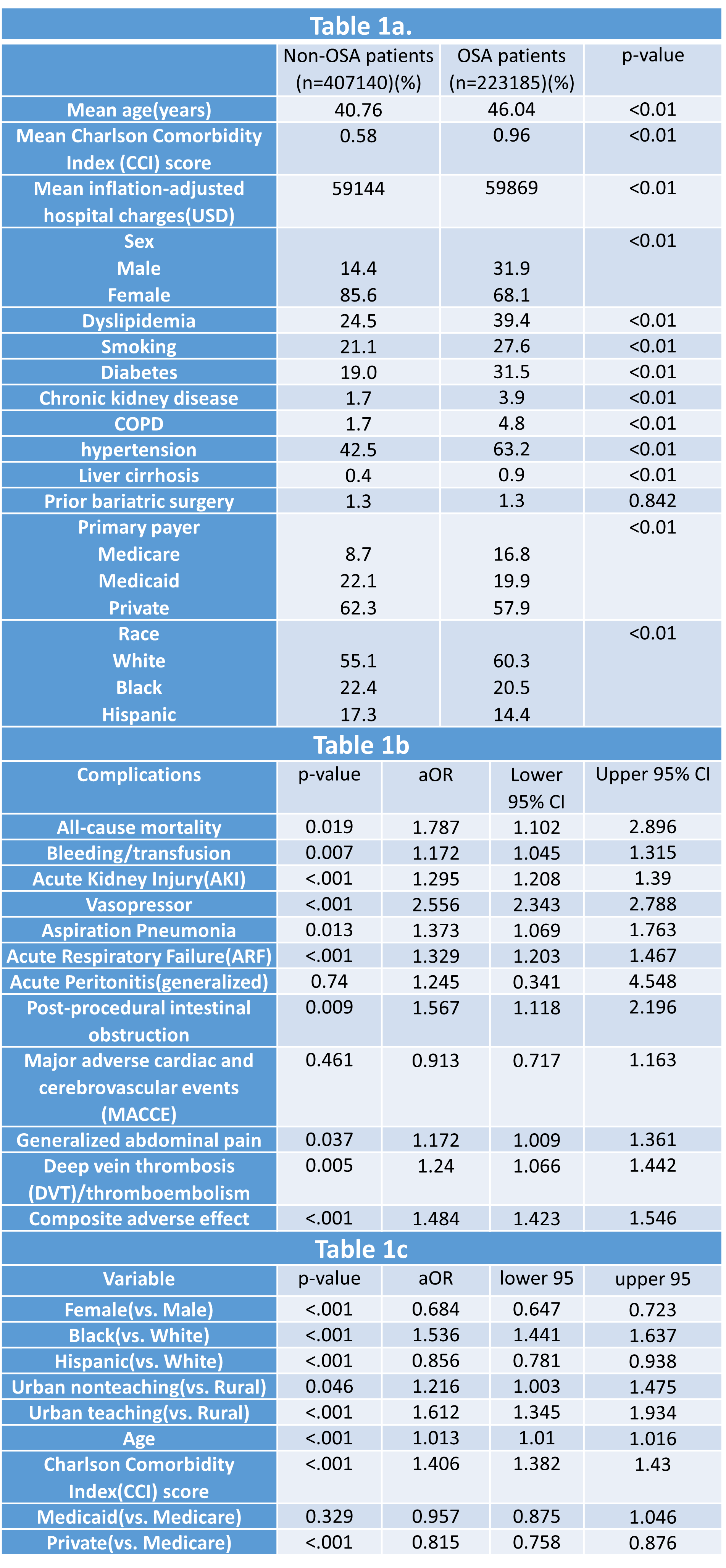
Figure: Table 1a- Baseline demographics and comorbidities among OSA vs non-OSA cases
Table 1b - Adverse events seen in OSA patients (Vs non-OSA as reference)
Table 1c- Variables including composite adverse events among OSA patients
Disclosures:
Renuka Verma indicated no relevant financial relationships.
Kristie Liao indicated no relevant financial relationships.
Kamleshun Ramphul indicated no relevant financial relationships.
Vignan Manne indicated no relevant financial relationships.
Renuka Verma, MD1, Kristie Liao, DO2, Kamleshun Ramphul, MD3, Vignan Manne, MD1. P4834 - Impact of Obstructive Sleep Apnea Among Morbidly Obese Adults Undergoing Elective Laparoscopic Sleeve Gastrectomy in the United States, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
