Tuesday Poster Session
Category: Diet, Nutrition, and Obesity
P4829 - Comparing Glucagon-Like Peptide-1 Agonists and Lifestyle Modifications on Weight Loss in a Predominantly Hispanic Population
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Bulent Tolga Delibasi, BA (he/him/his)
University of Texas Health San Antonio
San Antonio, TX
Presenting Author(s)
Jason N.. Chen, MD, Bulent Tolga. Delibasi, BA, Connie Hu, BA, Thomas Tran, BSA, James Wang, MD, Charles Randall, MD
University of Texas Health San Antonio, San Antonio, TX
Introduction: Obesity is increasingly prevalent, affecting approximately 42% of Americans. In Bexar County, which includes San Antonio, the rate is even higher—around 72%. This is concerning because obesity is linked to various forms of metabolic dysfunction, including liver disease. Weight reduction remains a cornerstone of managing metabolic-associated liver conditions. While lifestyle modification has traditionally been the primary approach to weight loss, medications such as glucagon-like peptide-1 (GLP-1) agonists have gained popularity in recent years. This study aims to compare weight loss outcomes from GLP-1 agonists versus lifestyle interventions in a predominantly Hispanic and obese population.
Methods: In this ongoing retrospective chart review, the initial and follow-up body mass index (BMI) of adult patients with Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD) were recorded at intervals ranging from 6 months to 3 years. Data on lifestyle modifications (such as diet and exercise) and the use of GLP-1 agonists were also collected. Descriptive statistics and two-sample t-tests (α = 0.05) were used to analyze differences in BMI based on these independent variables.
Results: Of 141 patients, the average age was 59 years, with 66.7% female and 51.1% Hispanic. 54.6% were initially obese. On average, participants lost 2.5% in BMI with lifestyle changes or GLP-1 use. Specifically, those who used GLP-1 agonists had a significantly greater decrease in BMI (4.3% decrease) compared to those who did lifestyle management only (1.2% decrease) (p = 0.02) (Figure 1). Further, there was no significant difference in weight change between Hispanic and non-Hispanic GLP-1 users (p = 0.24), though non-Hispanics had a greater average BMI reduction (6% vs. 3.4%).
Discussion: GLP-1 receptor agonists were significantly more effective in inducing weight loss compared to lifestyle modifications alone in this predominantly Hispanic patient population. While both interventions led to reductions in BMI, patients using GLP-1 agonists on average lost more than double the amount of weight than those only implementing lifestyle changes. This difference in efficacy supports the growing body of evidence that pharmacologic agents such as GLP-1 receptor agonists can meaningfully augment weight loss beyond lifestyle modifications alone, especially in regards to populations disproportionately experiencing higher levels of obesity and its associated health complications.
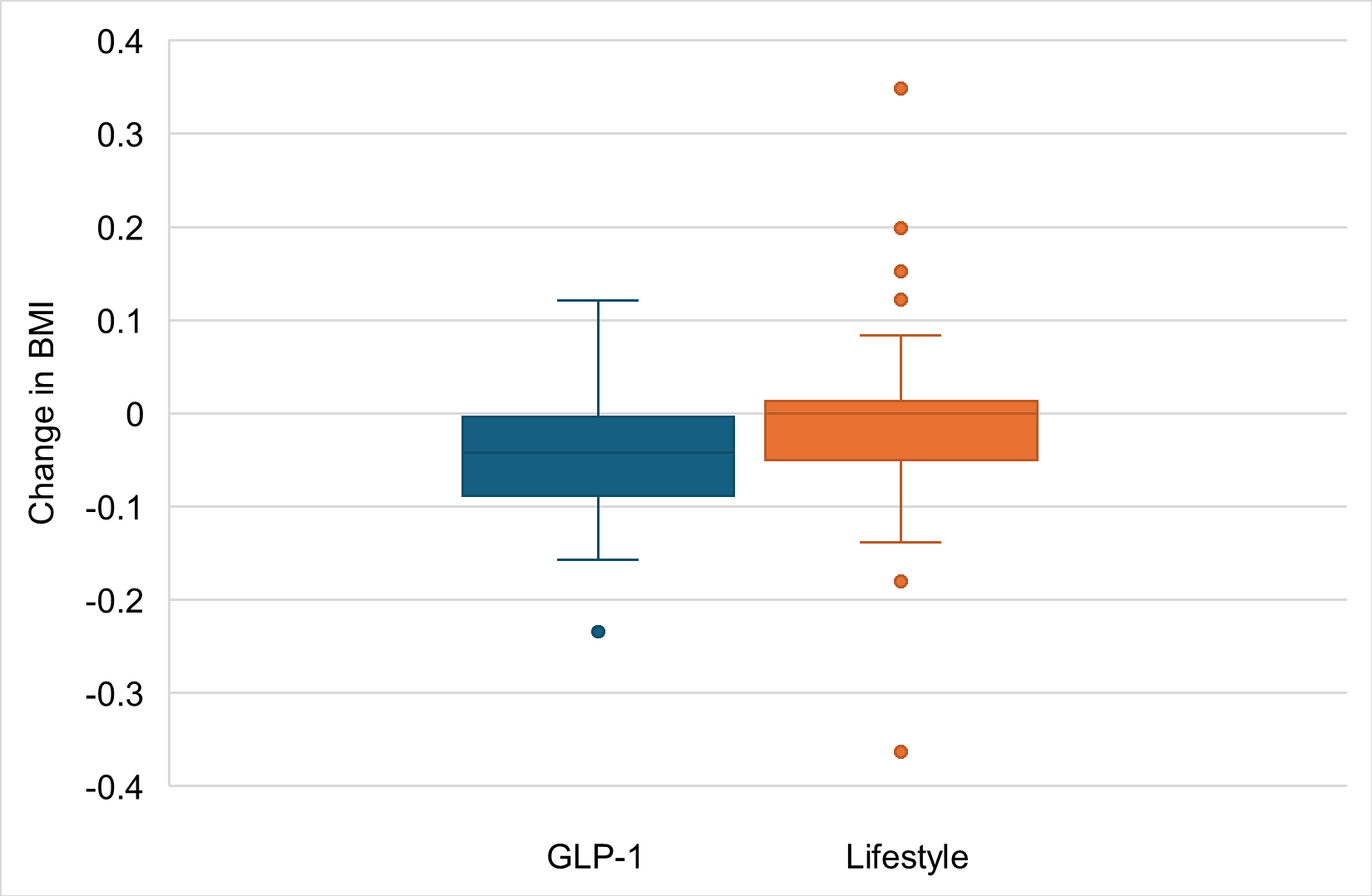
Figure: Figure 1. Change in body mass index (BMI) in patients taking GLP-1 agonists and those engaging in lifestyle changes only.
Disclosures:
Jason Chen indicated no relevant financial relationships.
Bulent Delibasi indicated no relevant financial relationships.
Connie Hu indicated no relevant financial relationships.
Thomas Tran indicated no relevant financial relationships.
James Wang indicated no relevant financial relationships.
Charles Randall indicated no relevant financial relationships.
Jason N.. Chen, MD, Bulent Tolga. Delibasi, BA, Connie Hu, BA, Thomas Tran, BSA, James Wang, MD, Charles Randall, MD. P4829 - Comparing Glucagon-Like Peptide-1 Agonists and Lifestyle Modifications on Weight Loss in a Predominantly Hispanic Population, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Texas Health San Antonio, San Antonio, TX
Introduction: Obesity is increasingly prevalent, affecting approximately 42% of Americans. In Bexar County, which includes San Antonio, the rate is even higher—around 72%. This is concerning because obesity is linked to various forms of metabolic dysfunction, including liver disease. Weight reduction remains a cornerstone of managing metabolic-associated liver conditions. While lifestyle modification has traditionally been the primary approach to weight loss, medications such as glucagon-like peptide-1 (GLP-1) agonists have gained popularity in recent years. This study aims to compare weight loss outcomes from GLP-1 agonists versus lifestyle interventions in a predominantly Hispanic and obese population.
Methods: In this ongoing retrospective chart review, the initial and follow-up body mass index (BMI) of adult patients with Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD) were recorded at intervals ranging from 6 months to 3 years. Data on lifestyle modifications (such as diet and exercise) and the use of GLP-1 agonists were also collected. Descriptive statistics and two-sample t-tests (α = 0.05) were used to analyze differences in BMI based on these independent variables.
Results: Of 141 patients, the average age was 59 years, with 66.7% female and 51.1% Hispanic. 54.6% were initially obese. On average, participants lost 2.5% in BMI with lifestyle changes or GLP-1 use. Specifically, those who used GLP-1 agonists had a significantly greater decrease in BMI (4.3% decrease) compared to those who did lifestyle management only (1.2% decrease) (p = 0.02) (Figure 1). Further, there was no significant difference in weight change between Hispanic and non-Hispanic GLP-1 users (p = 0.24), though non-Hispanics had a greater average BMI reduction (6% vs. 3.4%).
Discussion: GLP-1 receptor agonists were significantly more effective in inducing weight loss compared to lifestyle modifications alone in this predominantly Hispanic patient population. While both interventions led to reductions in BMI, patients using GLP-1 agonists on average lost more than double the amount of weight than those only implementing lifestyle changes. This difference in efficacy supports the growing body of evidence that pharmacologic agents such as GLP-1 receptor agonists can meaningfully augment weight loss beyond lifestyle modifications alone, especially in regards to populations disproportionately experiencing higher levels of obesity and its associated health complications.
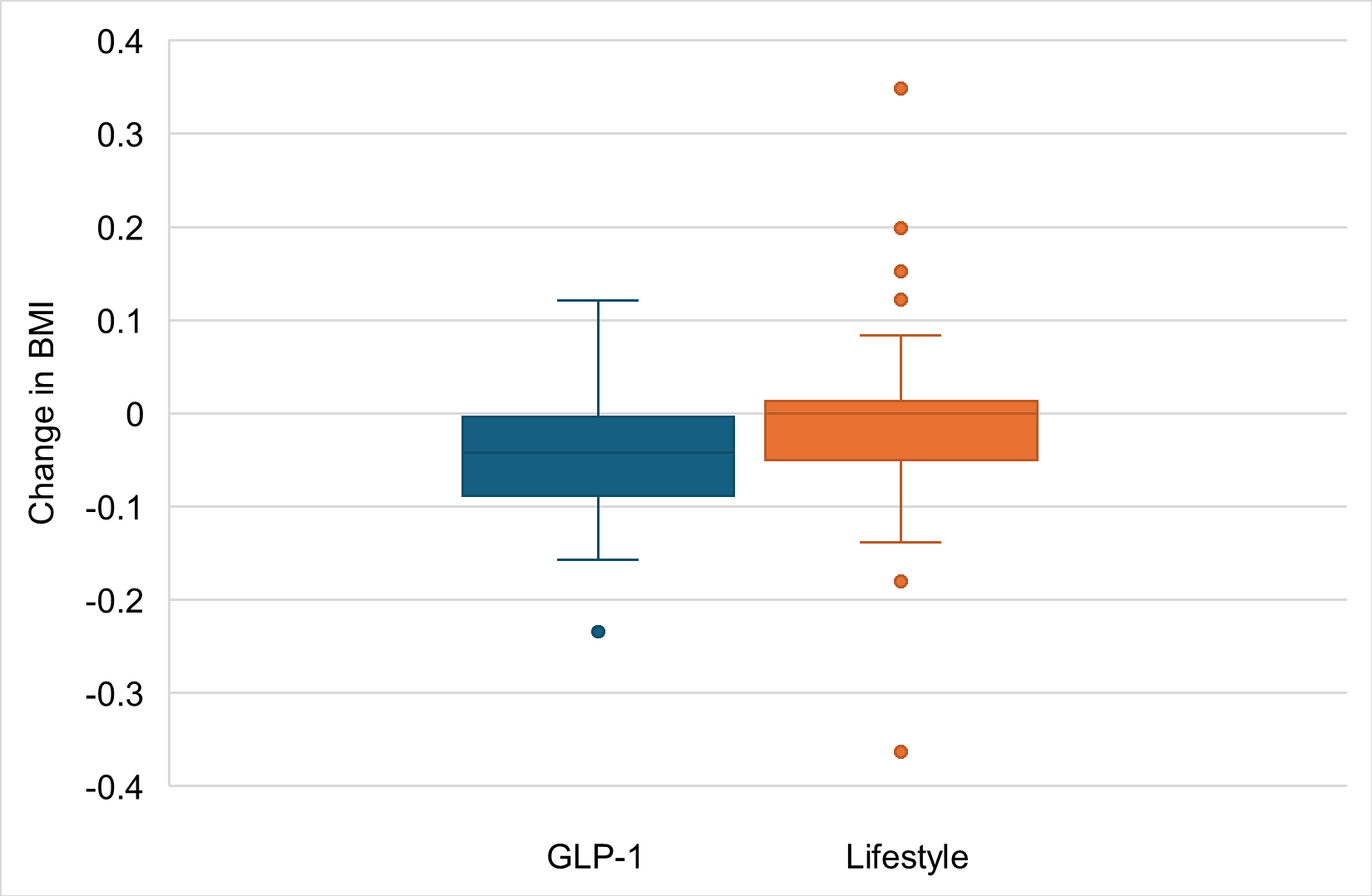
Figure: Figure 1. Change in body mass index (BMI) in patients taking GLP-1 agonists and those engaging in lifestyle changes only.
Disclosures:
Jason Chen indicated no relevant financial relationships.
Bulent Delibasi indicated no relevant financial relationships.
Connie Hu indicated no relevant financial relationships.
Thomas Tran indicated no relevant financial relationships.
James Wang indicated no relevant financial relationships.
Charles Randall indicated no relevant financial relationships.
Jason N.. Chen, MD, Bulent Tolga. Delibasi, BA, Connie Hu, BA, Thomas Tran, BSA, James Wang, MD, Charles Randall, MD. P4829 - Comparing Glucagon-Like Peptide-1 Agonists and Lifestyle Modifications on Weight Loss in a Predominantly Hispanic Population, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
