Tuesday Poster Session
Category: Diet, Nutrition, and Obesity
P4828 - Comparative Analysis of Nutritional Strategies and Their Clinical Outcomes in ICU Patients With Gastrointestinal Disorders: An EMR-Based Retrospective Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Samrat Babu Koirala, MD (he/him/his)
University of Central Florida, HCA Healthcare GME
Pensacola, FL
Presenting Author(s)
Samrat Koirala, MD1, Priya Kumari Maheshwari, MD1, Sri Harsha Boppana, MBBS, MD2, Thais M. Schwartz, MPH1, Ali Tariq, MD3
1University of Central Florida, HCA Healthcare GME, Pensacola, FL; 2Nassau University Medical Center, East Meadow, NY; 3HCA FLORIDA WEST HOSPITAL, Pensacola, FL
Introduction: Nutritional support is essential in the management of critically ill patients with gastrointestinal (GI) disorders. However, the optimal modes of nutrition are enteral, parenteral, or a combination which remains unclear in this population. This study aimed to compare clinical outcomes across different nutritional strategies in Intensive Care Unit (ICU) patients with GI diagnoses.
Methods: This retrospective cohort study analyzed Electronic Medical Record (EMR) data from the HCA North Florida Division between January 2016 and January 2024. Adult ICU patients (≥18 years) with a primary or secondary GI diagnosis were included. Patients were categorized by nutritional support type: enteral, parenteral, or combined. Primary outcomes were hospital length of stay (LOS), ICU LOS, and 90-day readmission. Statistical models included negative binomial regression for hospital LOS, generalized linear modeling (gamma distribution) for ICU LOS, and logistic regression for readmission. Models were adjusted for age, sex, BMI, sepsis, chronic kidney disease (CKD), and GI diagnosis subtype.
Results: A total of 2,569 patients met the inclusion criteria and were analyzed (8.8% enteral, 76.4% parenteral, 14.8% combined) (Figure 1). Patients receiving combined enteral/parenteral nutrition had the longest hospital LOS (mean 20.2 days) and ICU LOS (mean 10.2 days). Compared to parenteral support alone, combined nutrition was associated with longer hospital LOS (IRR 1.74, 95% CI: 1.58–1.92; p< 0.001) and ICU LOS (exp(β)=1.45, 95% CI: 1.30–1.63; p< 0.001). Enteral nutrition alone was associated with significantly shorter ICU stays than combined support (exp(β)=0.67, 95% CI: 0.57–0.79; p< 0.001). No significant differences in 90-day readmission were observed between groups. Sepsis and CKD were independently associated with prolonged LOS, while female sex was linked to increased readmission risk (OR 1.21, 95% CI: 1.03–2.75; p=0.0364).
Discussion: Among ICU patients with GI disorders, combined enteral and parenteral nutrition was associated with significantly prolonged hospital and ICU stays, potentially reflecting greater severity of illness. In contrast, enteral nutrition alone was associated with more favorable ICU outcomes, suggesting a potential benefit in carefully selected patients. These findings underscore the importance of tailoring nutritional strategies to patient condition and diagnosis and support the integration of early nutritional decision-making into multidisciplinary critical care planning.
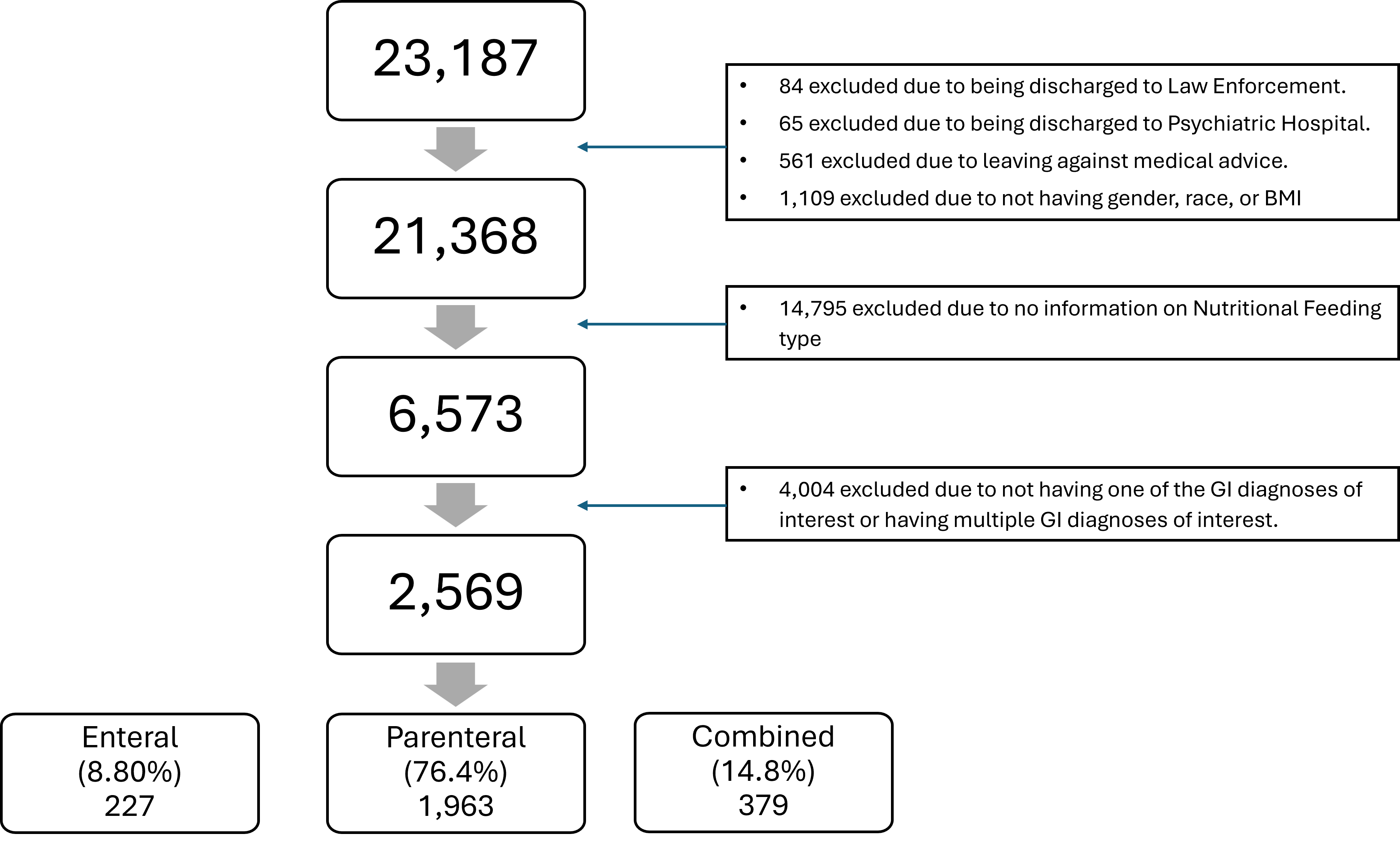
Figure: Figure 1: Flowchart of patient selection and cohort allocation
Disclosures:
Samrat Koirala indicated no relevant financial relationships.
Priya Kumari Maheshwari indicated no relevant financial relationships.
Sri Harsha Boppana indicated no relevant financial relationships.
Thais Schwartz indicated no relevant financial relationships.
Ali Tariq indicated no relevant financial relationships.
Samrat Koirala, MD1, Priya Kumari Maheshwari, MD1, Sri Harsha Boppana, MBBS, MD2, Thais M. Schwartz, MPH1, Ali Tariq, MD3. P4828 - Comparative Analysis of Nutritional Strategies and Their Clinical Outcomes in ICU Patients With Gastrointestinal Disorders: An EMR-Based Retrospective Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Central Florida, HCA Healthcare GME, Pensacola, FL; 2Nassau University Medical Center, East Meadow, NY; 3HCA FLORIDA WEST HOSPITAL, Pensacola, FL
Introduction: Nutritional support is essential in the management of critically ill patients with gastrointestinal (GI) disorders. However, the optimal modes of nutrition are enteral, parenteral, or a combination which remains unclear in this population. This study aimed to compare clinical outcomes across different nutritional strategies in Intensive Care Unit (ICU) patients with GI diagnoses.
Methods: This retrospective cohort study analyzed Electronic Medical Record (EMR) data from the HCA North Florida Division between January 2016 and January 2024. Adult ICU patients (≥18 years) with a primary or secondary GI diagnosis were included. Patients were categorized by nutritional support type: enteral, parenteral, or combined. Primary outcomes were hospital length of stay (LOS), ICU LOS, and 90-day readmission. Statistical models included negative binomial regression for hospital LOS, generalized linear modeling (gamma distribution) for ICU LOS, and logistic regression for readmission. Models were adjusted for age, sex, BMI, sepsis, chronic kidney disease (CKD), and GI diagnosis subtype.
Results: A total of 2,569 patients met the inclusion criteria and were analyzed (8.8% enteral, 76.4% parenteral, 14.8% combined) (Figure 1). Patients receiving combined enteral/parenteral nutrition had the longest hospital LOS (mean 20.2 days) and ICU LOS (mean 10.2 days). Compared to parenteral support alone, combined nutrition was associated with longer hospital LOS (IRR 1.74, 95% CI: 1.58–1.92; p< 0.001) and ICU LOS (exp(β)=1.45, 95% CI: 1.30–1.63; p< 0.001). Enteral nutrition alone was associated with significantly shorter ICU stays than combined support (exp(β)=0.67, 95% CI: 0.57–0.79; p< 0.001). No significant differences in 90-day readmission were observed between groups. Sepsis and CKD were independently associated with prolonged LOS, while female sex was linked to increased readmission risk (OR 1.21, 95% CI: 1.03–2.75; p=0.0364).
Discussion: Among ICU patients with GI disorders, combined enteral and parenteral nutrition was associated with significantly prolonged hospital and ICU stays, potentially reflecting greater severity of illness. In contrast, enteral nutrition alone was associated with more favorable ICU outcomes, suggesting a potential benefit in carefully selected patients. These findings underscore the importance of tailoring nutritional strategies to patient condition and diagnosis and support the integration of early nutritional decision-making into multidisciplinary critical care planning.
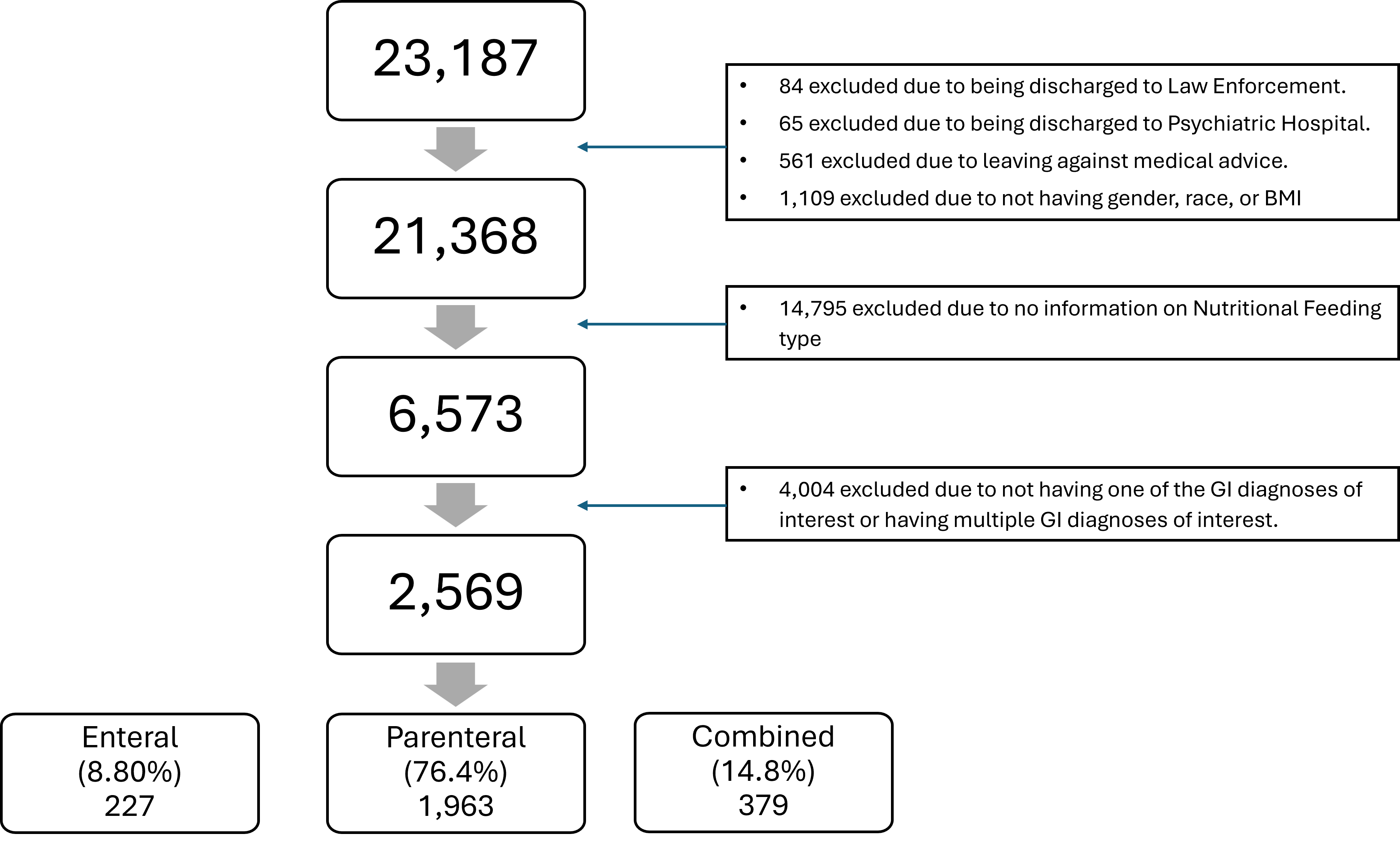
Figure: Figure 1: Flowchart of patient selection and cohort allocation
Disclosures:
Samrat Koirala indicated no relevant financial relationships.
Priya Kumari Maheshwari indicated no relevant financial relationships.
Sri Harsha Boppana indicated no relevant financial relationships.
Thais Schwartz indicated no relevant financial relationships.
Ali Tariq indicated no relevant financial relationships.
Samrat Koirala, MD1, Priya Kumari Maheshwari, MD1, Sri Harsha Boppana, MBBS, MD2, Thais M. Schwartz, MPH1, Ali Tariq, MD3. P4828 - Comparative Analysis of Nutritional Strategies and Their Clinical Outcomes in ICU Patients With Gastrointestinal Disorders: An EMR-Based Retrospective Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
