Tuesday Poster Session
Category: Colorectal Cancer Prevention
P4816 - When Routine Saves Lives: Incidental Finding of Mantle Cell Lymphoma During Screening Colonoscopy
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Agustin Gavidia Rosario, MD
Henry Ford Health
Detroit, MI
Presenting Author(s)
Mohammed Abusuliman, MD1, Agustin Gavidia Rosario, MD2, Omar Abbas, MD2, Taher Jamali, MD1, Remy Arwani, MD1, Jawad Z. Sheqwara, MD1, Sumair Ahmad, MD2
1Henry Ford Hospital, Detroit, MI; 2Henry Ford Health, Detroit, MI
Introduction: Mantle cell lymphoma (MCL) is a rare subtype of non-Hodgkin lymphoma that often involves lymph nodes, spleen, bone marrow, and gastrointestinal (GI) tract. However, primary colonic involvement is extremely uncommon, representing only about 2% of primary GI lymphomas. Because of its rarity and often nonspecific presentation, MCL of the colon may go unrecognized, particularly in asymptomatic individuals. We present a case on MCL in a patient that was completely asymptomatic as he underwent his first screening colonoscopy. This case illustrates the importance of routine screening colonoscopies, even in younger individuals without GI symptoms or family history of colon disease.
Case Description/
Methods: A 45-year-old man with no family history of colon cancer and no significant GI complaints was referred for routine screening colonoscopy. The examination revealed multiple submucosal lesions throughout the colon. Notably, a 5 × 5 cm superficially ulcerated mass was found in the cecum, partially obstructing the ileocecal valve. An 8 mm submucosal nodule was identified in the ileum 5 cm from the valve, along with numerous additional nodules (3–30 mm) across the colon, many with a yellow hue and central umbilication (Figure 1A-1G). No bleeding was observed. Cold forceps biopsies were obtained.
Histopathology revealed a dense lymphoid infiltrate composed of neoplastic B cells expressing CD5, CD20, Cyclin D1, and SOX-11 (Figure 2A-2E), The Ki-67 proliferation index was elevated (40%–50%), and Fluorescence in situ hybridization confirmed t(11;14)(q13;q32) (Figure 2E), TP53 mutation testing was negative, establishing the diagnosis of mantle cell lymphoma. Positron emission tomography (PET) and computed tomography (CT) imaging demonstrated mild diffuse adenopathy, possible gastric involvement, and splenomegaly.
The patient was initiated on alternating cycles of R-CHOP-Zanubrutinib and R-DHAOx and is currently responding well to therapy.
Discussion: This rare case of colonic MCL identified during a routine screening colonoscopy in an asymptomatic, average-risk 45-year-old underscores the critical diagnostic value of early screening. It highlights the need for clinician awareness of atypical presentations of GI lymphomas and supports maintaining a high index of suspicion even in patients without classical risk factors.

Figure: Figure 1: Colonoscopy pictures. 1-A: Ascending colon submucosal nodules, 1-B:
Ascending colon submucosal lesion, 1-C: Enlarged ileocecal valve with mass-like
appearing and fungative mucosa, 1-D: Ileocecal valve under narrow band imaging, 1-E:
Sigmoid and descending colon submucosal nodule with umbilicated center, 1-F:
Submucosal life attempted with saline of transverse colon lesions (failure to lift reflecting
deep submucosal involvement), 1-G: Terminal ileum nodule.
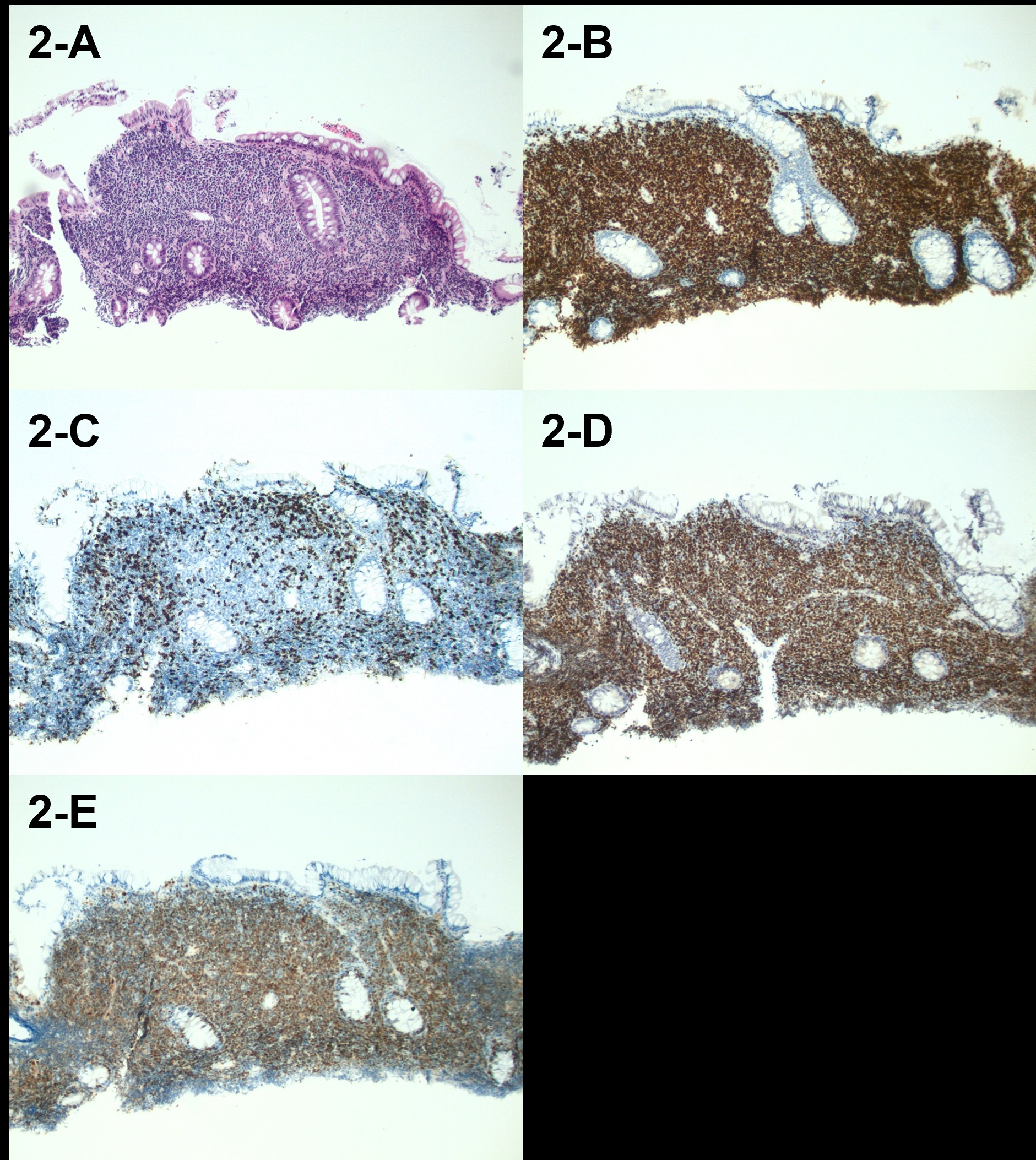
Figure: Figure 2: histopathology pictures, 2-A: H&E stain showing dense lymphoid infiltrate
within the lamina propria that is partially displacing the colonic crypts but not
significantly invading the epithelium.2-B: Immunohistochemical (IHC) stain showing a
positive PAX5 signal in most of the cell infiltrate, confirming a B cell origin of the
neoplasm.2-C: IHC stain showing negative results for CD3 in the lymphoid cell infiltrate,
also supporting a B cell neoplastic origin.2-D: IHC stain showing a strong positive
nuclear signal for the key MCL biomarker SOX11 in the neoplastic B cells infiltrating the
lamina propria.2-E: Fluorescence in situ hybridization stain showing strong cytoplasmic
signal for BCL-1 in the B cells within the lamina propria infiltrate, which is consistent with
cyclin D1 overexpression due to the t(11;14)(q13;q32) translocation, a hallmark genetic
variant in MCL.
Magnification 100X for all panels
Disclosures:
Mohammed Abusuliman indicated no relevant financial relationships.
Agustin Gavidia Rosario indicated no relevant financial relationships.
Omar Abbas indicated no relevant financial relationships.
Taher Jamali indicated no relevant financial relationships.
Remy Arwani indicated no relevant financial relationships.
Jawad Z. Sheqwara indicated no relevant financial relationships.
Sumair Ahmad indicated no relevant financial relationships.
Mohammed Abusuliman, MD1, Agustin Gavidia Rosario, MD2, Omar Abbas, MD2, Taher Jamali, MD1, Remy Arwani, MD1, Jawad Z. Sheqwara, MD1, Sumair Ahmad, MD2. P4816 - When Routine Saves Lives: Incidental Finding of Mantle Cell Lymphoma During Screening Colonoscopy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Henry Ford Hospital, Detroit, MI; 2Henry Ford Health, Detroit, MI
Introduction: Mantle cell lymphoma (MCL) is a rare subtype of non-Hodgkin lymphoma that often involves lymph nodes, spleen, bone marrow, and gastrointestinal (GI) tract. However, primary colonic involvement is extremely uncommon, representing only about 2% of primary GI lymphomas. Because of its rarity and often nonspecific presentation, MCL of the colon may go unrecognized, particularly in asymptomatic individuals. We present a case on MCL in a patient that was completely asymptomatic as he underwent his first screening colonoscopy. This case illustrates the importance of routine screening colonoscopies, even in younger individuals without GI symptoms or family history of colon disease.
Case Description/
Methods: A 45-year-old man with no family history of colon cancer and no significant GI complaints was referred for routine screening colonoscopy. The examination revealed multiple submucosal lesions throughout the colon. Notably, a 5 × 5 cm superficially ulcerated mass was found in the cecum, partially obstructing the ileocecal valve. An 8 mm submucosal nodule was identified in the ileum 5 cm from the valve, along with numerous additional nodules (3–30 mm) across the colon, many with a yellow hue and central umbilication (Figure 1A-1G). No bleeding was observed. Cold forceps biopsies were obtained.
Histopathology revealed a dense lymphoid infiltrate composed of neoplastic B cells expressing CD5, CD20, Cyclin D1, and SOX-11 (Figure 2A-2E), The Ki-67 proliferation index was elevated (40%–50%), and Fluorescence in situ hybridization confirmed t(11;14)(q13;q32) (Figure 2E), TP53 mutation testing was negative, establishing the diagnosis of mantle cell lymphoma. Positron emission tomography (PET) and computed tomography (CT) imaging demonstrated mild diffuse adenopathy, possible gastric involvement, and splenomegaly.
The patient was initiated on alternating cycles of R-CHOP-Zanubrutinib and R-DHAOx and is currently responding well to therapy.
Discussion: This rare case of colonic MCL identified during a routine screening colonoscopy in an asymptomatic, average-risk 45-year-old underscores the critical diagnostic value of early screening. It highlights the need for clinician awareness of atypical presentations of GI lymphomas and supports maintaining a high index of suspicion even in patients without classical risk factors.

Figure: Figure 1: Colonoscopy pictures. 1-A: Ascending colon submucosal nodules, 1-B:
Ascending colon submucosal lesion, 1-C: Enlarged ileocecal valve with mass-like
appearing and fungative mucosa, 1-D: Ileocecal valve under narrow band imaging, 1-E:
Sigmoid and descending colon submucosal nodule with umbilicated center, 1-F:
Submucosal life attempted with saline of transverse colon lesions (failure to lift reflecting
deep submucosal involvement), 1-G: Terminal ileum nodule.
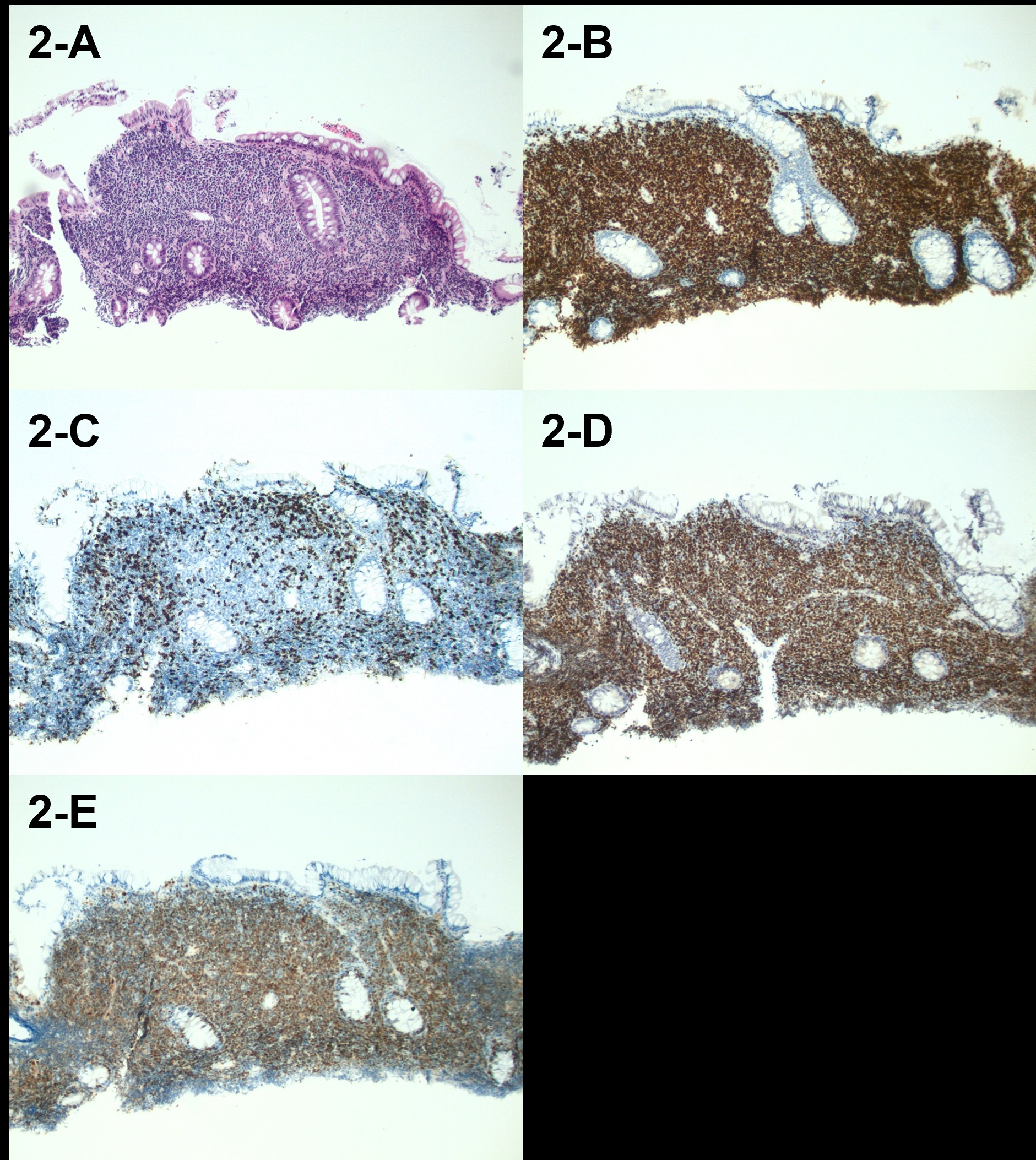
Figure: Figure 2: histopathology pictures, 2-A: H&E stain showing dense lymphoid infiltrate
within the lamina propria that is partially displacing the colonic crypts but not
significantly invading the epithelium.2-B: Immunohistochemical (IHC) stain showing a
positive PAX5 signal in most of the cell infiltrate, confirming a B cell origin of the
neoplasm.2-C: IHC stain showing negative results for CD3 in the lymphoid cell infiltrate,
also supporting a B cell neoplastic origin.2-D: IHC stain showing a strong positive
nuclear signal for the key MCL biomarker SOX11 in the neoplastic B cells infiltrating the
lamina propria.2-E: Fluorescence in situ hybridization stain showing strong cytoplasmic
signal for BCL-1 in the B cells within the lamina propria infiltrate, which is consistent with
cyclin D1 overexpression due to the t(11;14)(q13;q32) translocation, a hallmark genetic
variant in MCL.
Magnification 100X for all panels
Disclosures:
Mohammed Abusuliman indicated no relevant financial relationships.
Agustin Gavidia Rosario indicated no relevant financial relationships.
Omar Abbas indicated no relevant financial relationships.
Taher Jamali indicated no relevant financial relationships.
Remy Arwani indicated no relevant financial relationships.
Jawad Z. Sheqwara indicated no relevant financial relationships.
Sumair Ahmad indicated no relevant financial relationships.
Mohammed Abusuliman, MD1, Agustin Gavidia Rosario, MD2, Omar Abbas, MD2, Taher Jamali, MD1, Remy Arwani, MD1, Jawad Z. Sheqwara, MD1, Sumair Ahmad, MD2. P4816 - When Routine Saves Lives: Incidental Finding of Mantle Cell Lymphoma During Screening Colonoscopy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
