Tuesday Poster Session
Category: Colorectal Cancer Prevention
P4807 - Trends in Incidence and Survival of Gastrointestinal Neuroendocrine Tumors in a Large Healthcare Network: A Retrospective Analysis (2012–2024)
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- FC
Fan Cao, BS
Georgetown University School of Medicine
Arlington, DC
Presenting Author(s)
Fan Cao, BS1, Michael Tseng, MD2, Jiling Chou, MA2, Priyanka Kanth, MD2
1Georgetown University School of Medicine, Arlington, DC; 2MedStar Georgetown University Hospital, Washington, DC
Introduction: Neuroendocrine tumors (NETs) are a group of rare, heterogeneous group of tumors that can occur in any part of the body. The overall prevalence of GI neuroendocrine tumors has been rising over the past decade. However, the incidence and survival outcomes remain insufficiently investigated. This study investigates demographic and site-specific incidence trends of GINETs and assesses survival outcomes stratified by tumor characteristics, anatomical location, sex, race, and age.
Methods: A retrospective cohort study was conducted on 2,128 patients diagnosed with GINETs at 10 acute care hospitals in a large health network between November 2012 and September 2024, excluding cases identified via autopsy. Data were stratified by sex, race, age, and tumor types, sites using site-specific ICD codes. Kaplan-Meier survival analysis was performed to evaluate differences in survival across sex, race, and age (< 50, 51-74, >75 years old), benign, malignant, and mixed malignancy GINETs, as well as six anatomical sites. The log-rank test was used to determine statistical significance.
Results: The overall incidence of GINETs increased from 2012 to 2024. Women were found to have higher incidence rates than men (Fig 1). The highest prevalence was seen with White (48%) and Black (43%) patients (Fig 2). Most incidents were found in the 51–74-year age group, accounting for 55% of cases, with a rise in incidence in the < 51-year age group in recent years (Fig 3). Among the anatomical sites, tumors of the small intestine were most prevalent (Fig 4). Survival outcomes varied significantly by sex, age, race, tumor types, and sites. Better survival was noted in females, Whites, and younger patients (Fig 5-7). Benign GINETs exhibited the highest survival rates, followed by mixed malignancies, while malignant GINETs had the poorest outcomes (Fig 8). Site-specific analysis revealed rectum tumors with the most favorable survival rates, whereas large intestine GINETs had the worst outcomes (Fig 9).
Discussion: The incidence of GINETs has risen significantly over the past decade, likely due in part to increased screening, with notable variations across demographic groups and anatomical sites. Survival outcomes emphasize the importance of early detection and site-specific management strategies, particularly for pancreatic GINETs, which remain a high-mortality subset. This study highlights the critical need for targeted research and interventions to improve outcomes for diverse populations affected by GINETs.
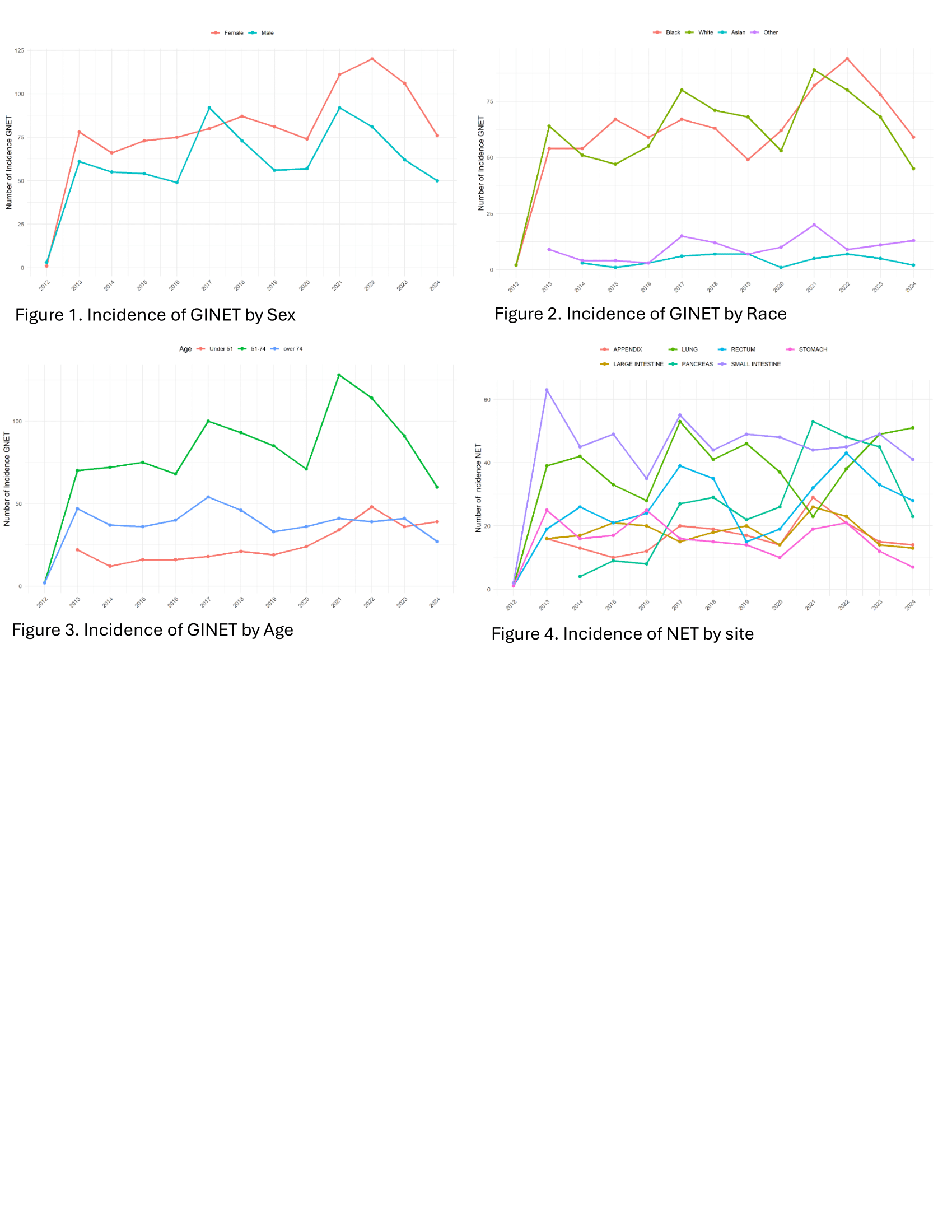
Figure: Figure 1-4 GINET Incidence by Sex, Race, Age, and Tumor site
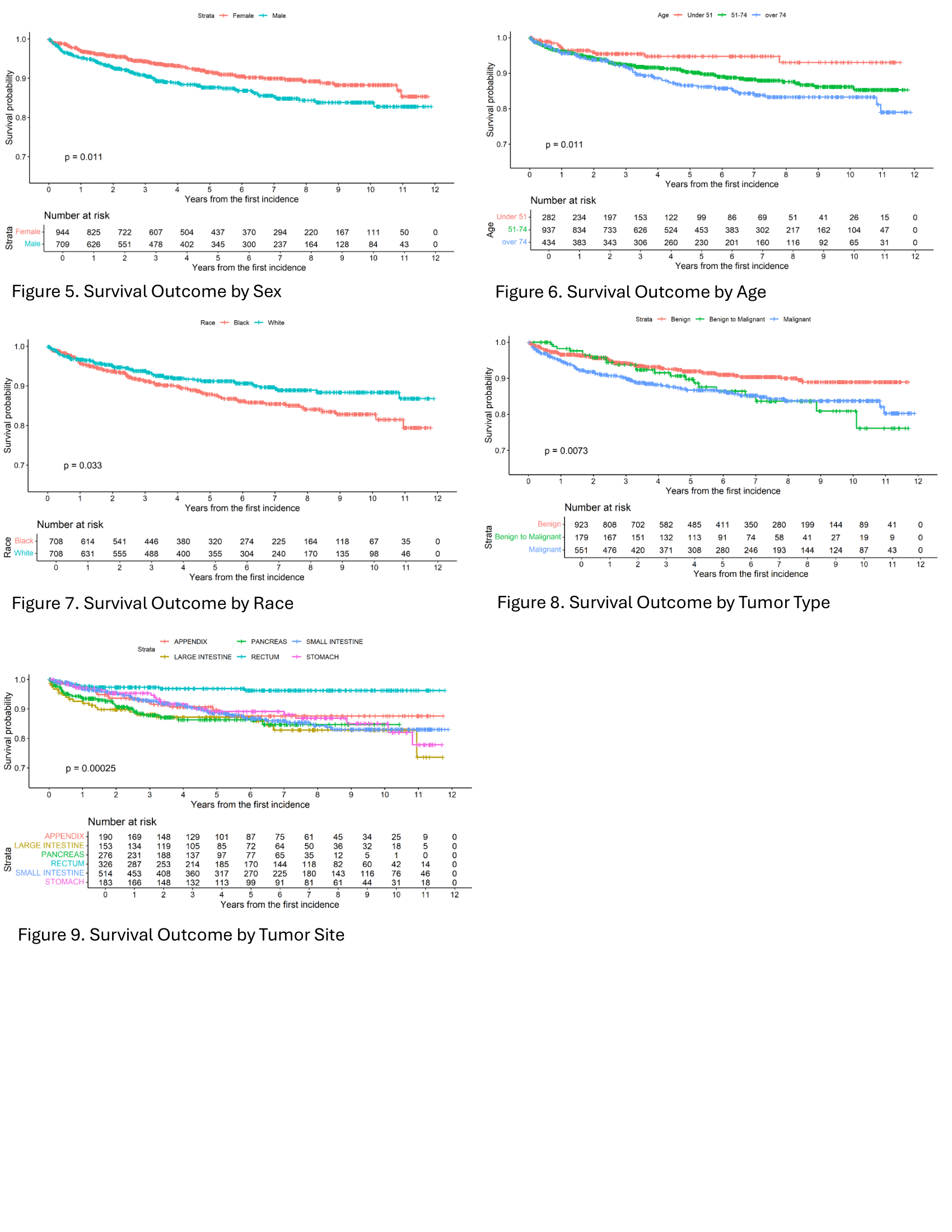
Figure: Figure 5-9 GINET Survival Outcome by Sex, Age, Race, Tumor types, and Tumor sites
Disclosures:
Fan Cao indicated no relevant financial relationships.
Michael Tseng indicated no relevant financial relationships.
Jiling Chou indicated no relevant financial relationships.
Priyanka Kanth indicated no relevant financial relationships.
Fan Cao, BS1, Michael Tseng, MD2, Jiling Chou, MA2, Priyanka Kanth, MD2. P4807 - Trends in Incidence and Survival of Gastrointestinal Neuroendocrine Tumors in a Large Healthcare Network: A Retrospective Analysis (2012–2024), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Georgetown University School of Medicine, Arlington, DC; 2MedStar Georgetown University Hospital, Washington, DC
Introduction: Neuroendocrine tumors (NETs) are a group of rare, heterogeneous group of tumors that can occur in any part of the body. The overall prevalence of GI neuroendocrine tumors has been rising over the past decade. However, the incidence and survival outcomes remain insufficiently investigated. This study investigates demographic and site-specific incidence trends of GINETs and assesses survival outcomes stratified by tumor characteristics, anatomical location, sex, race, and age.
Methods: A retrospective cohort study was conducted on 2,128 patients diagnosed with GINETs at 10 acute care hospitals in a large health network between November 2012 and September 2024, excluding cases identified via autopsy. Data were stratified by sex, race, age, and tumor types, sites using site-specific ICD codes. Kaplan-Meier survival analysis was performed to evaluate differences in survival across sex, race, and age (< 50, 51-74, >75 years old), benign, malignant, and mixed malignancy GINETs, as well as six anatomical sites. The log-rank test was used to determine statistical significance.
Results: The overall incidence of GINETs increased from 2012 to 2024. Women were found to have higher incidence rates than men (Fig 1). The highest prevalence was seen with White (48%) and Black (43%) patients (Fig 2). Most incidents were found in the 51–74-year age group, accounting for 55% of cases, with a rise in incidence in the < 51-year age group in recent years (Fig 3). Among the anatomical sites, tumors of the small intestine were most prevalent (Fig 4). Survival outcomes varied significantly by sex, age, race, tumor types, and sites. Better survival was noted in females, Whites, and younger patients (Fig 5-7). Benign GINETs exhibited the highest survival rates, followed by mixed malignancies, while malignant GINETs had the poorest outcomes (Fig 8). Site-specific analysis revealed rectum tumors with the most favorable survival rates, whereas large intestine GINETs had the worst outcomes (Fig 9).
Discussion: The incidence of GINETs has risen significantly over the past decade, likely due in part to increased screening, with notable variations across demographic groups and anatomical sites. Survival outcomes emphasize the importance of early detection and site-specific management strategies, particularly for pancreatic GINETs, which remain a high-mortality subset. This study highlights the critical need for targeted research and interventions to improve outcomes for diverse populations affected by GINETs.
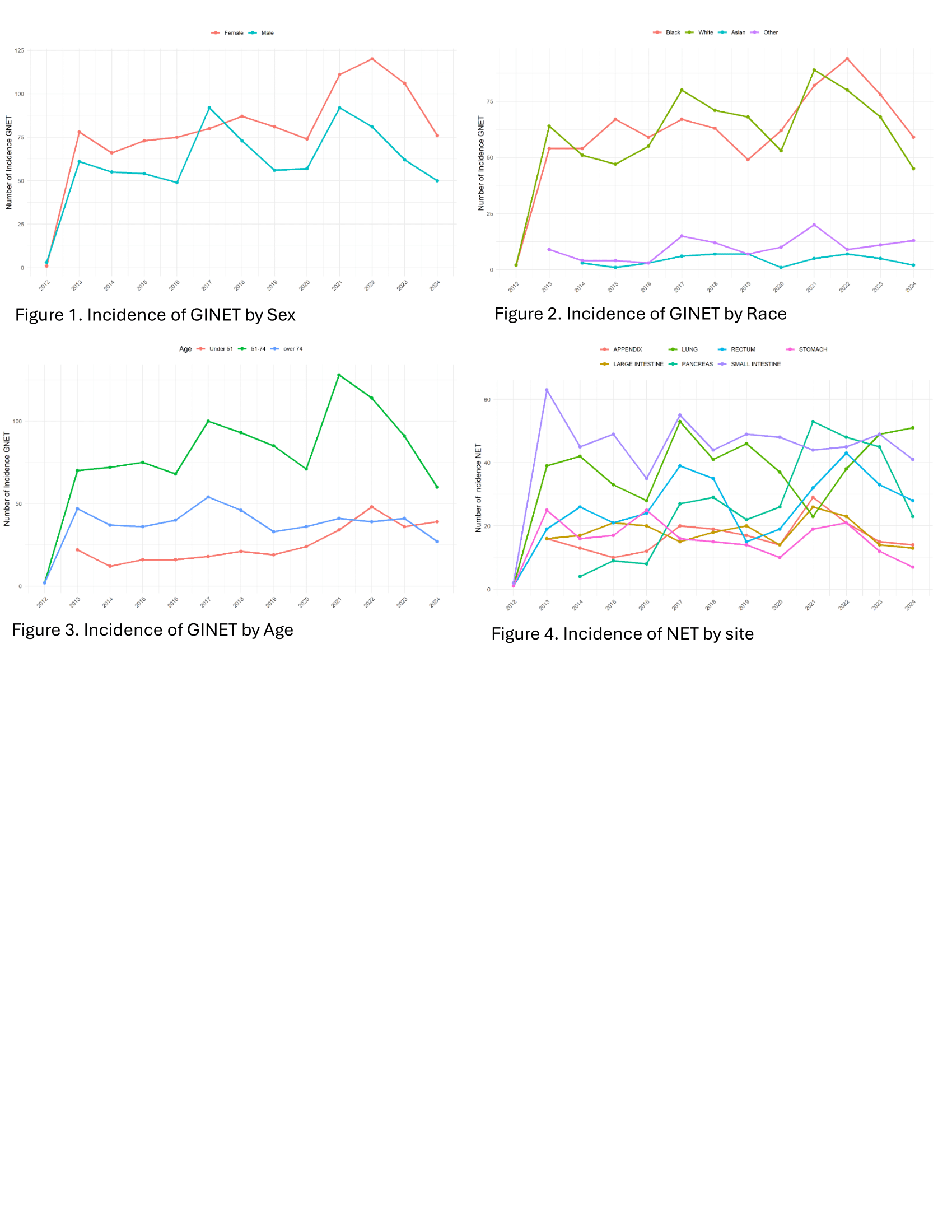
Figure: Figure 1-4 GINET Incidence by Sex, Race, Age, and Tumor site
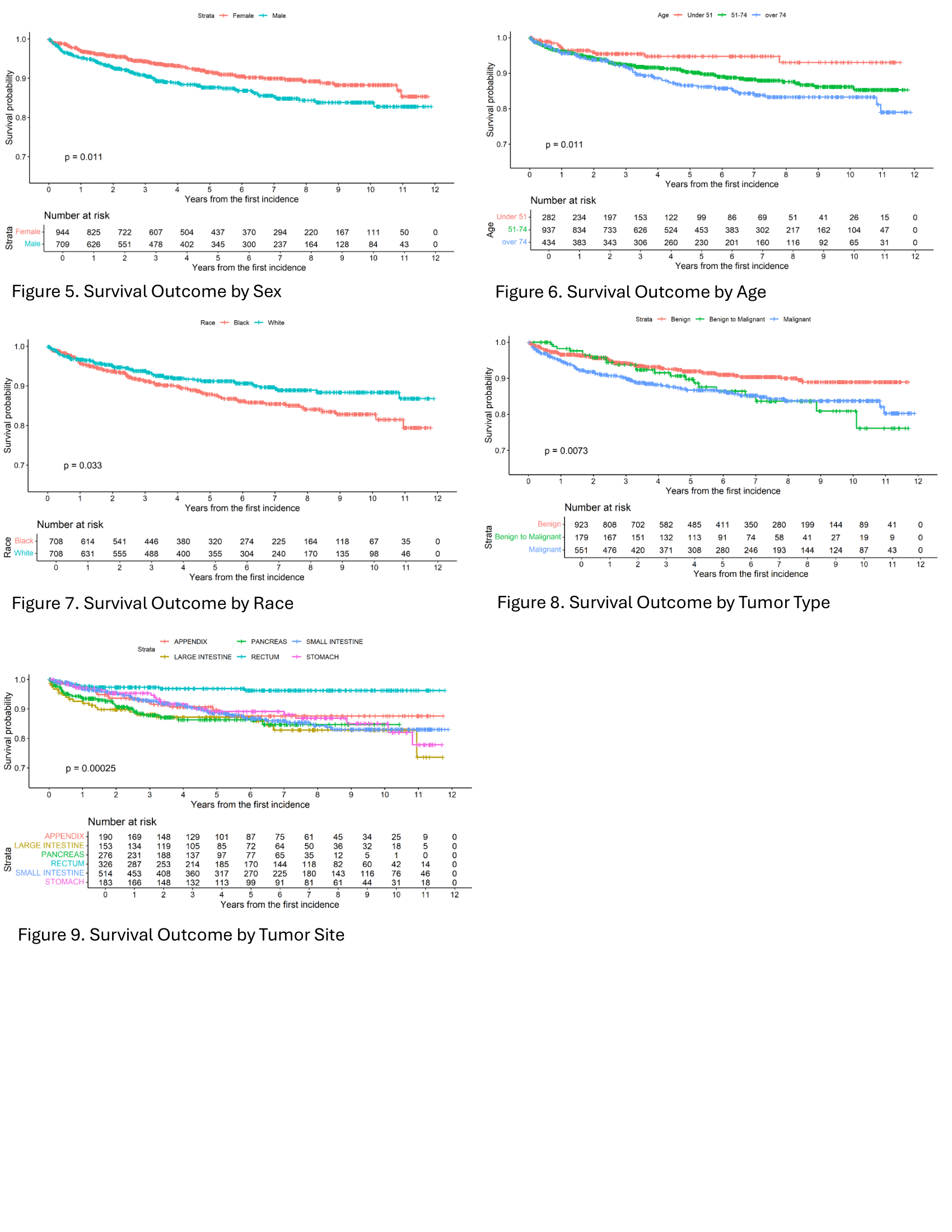
Figure: Figure 5-9 GINET Survival Outcome by Sex, Age, Race, Tumor types, and Tumor sites
Disclosures:
Fan Cao indicated no relevant financial relationships.
Michael Tseng indicated no relevant financial relationships.
Jiling Chou indicated no relevant financial relationships.
Priyanka Kanth indicated no relevant financial relationships.
Fan Cao, BS1, Michael Tseng, MD2, Jiling Chou, MA2, Priyanka Kanth, MD2. P4807 - Trends in Incidence and Survival of Gastrointestinal Neuroendocrine Tumors in a Large Healthcare Network: A Retrospective Analysis (2012–2024), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

