Tuesday Poster Session
Category: Colorectal Cancer Prevention
P4744 - Assessing Patient Preferences for Blood-Based Lung Cancer and Colorectal Cancer Screening Tests: Insights from a Conjoint Analysis with over 1,700 People in the US
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Jan Ballesteros, PhD
Cedars-Sinai Medical Center
Los Angeles, CA
Presenting Author(s)
Jan Ballesteros, PhD, Ayako Ikenouchi, MD, So Yung Choi, MS, Allistair Clark, MA, Brennan Spiegel, MD, MSHS, Christopher Almario, MD, MSHPM
Cedars-Sinai Medical Center, Los Angeles, CA
Introduction: Over 80% of people who smoke nicotine are not up-to-date with lung cancer screening, and more than 40% of eligible adults are not current with colorectal cancer (CRC) screening. Blood-based tests for both cancers offer a promising alternative to existing options. In this study, we used conjoint analysis to assess preferences for blood-based lung and CRC screening tests compared to traditional methods (e.g., low-dose CT [LDCT] for lung cancer; fecal immunochemical test [FIT], multitarget stool DNA [mt-sDNA], and colonoscopy for CRC).
Methods: We conducted a choice-based conjoint survey of US adults aged 50–75 years who were eligible but not up-to-date for lung and CRC screening per USPSTF guidelines. In the conjoint exercises, participants evaluated side-by-side hypothetical lung cancer and CRC screening test combinations that varied by modality, frequency, accuracy, and other features. We used hierarchical Bayes regression to estimate individual part-worth utilities, which were then used to conduct simulations assessing respondents’ preferred lung cancer and CRC screening test combinations: blood tests for both cancers, blood test for one and traditional for the other, or traditional tests for both. Multivariable logistic regression adjusted for confounding and identified factors associated with preferring blood-based screening for both cancers.
Results: A total of 1,741 participants completed the survey. As shown in the Figure, 43.9% of respondents preferred to do blood tests every 3 (Q3) years for both cancers, while 28.6% favored traditional options. Another 21.9% preferred a lung cancer blood test Q3 years with a traditional CRC test; 5.6% chose annual lung LDCT with a CRC blood test Q3 years. Regression results (Table) showed that non-married individuals, those with comorbidities, and those who do not exercise regularly were more likely to prefer blood tests to screen for both cancers (all p< 0.05). In contrast, non-Hispanic Black individuals with higher income, and those with a usual source of care were less likely to choose blood testing (all p< 0.05).
Discussion: Among a national sample of individuals not up-to-date with lung and CRC screening, nearly half preferred blood tests for both cancers over traditional methods. These findings suggest that blood-based screening is broadly acceptable and may help address barriers to participation in cancer screening programs.
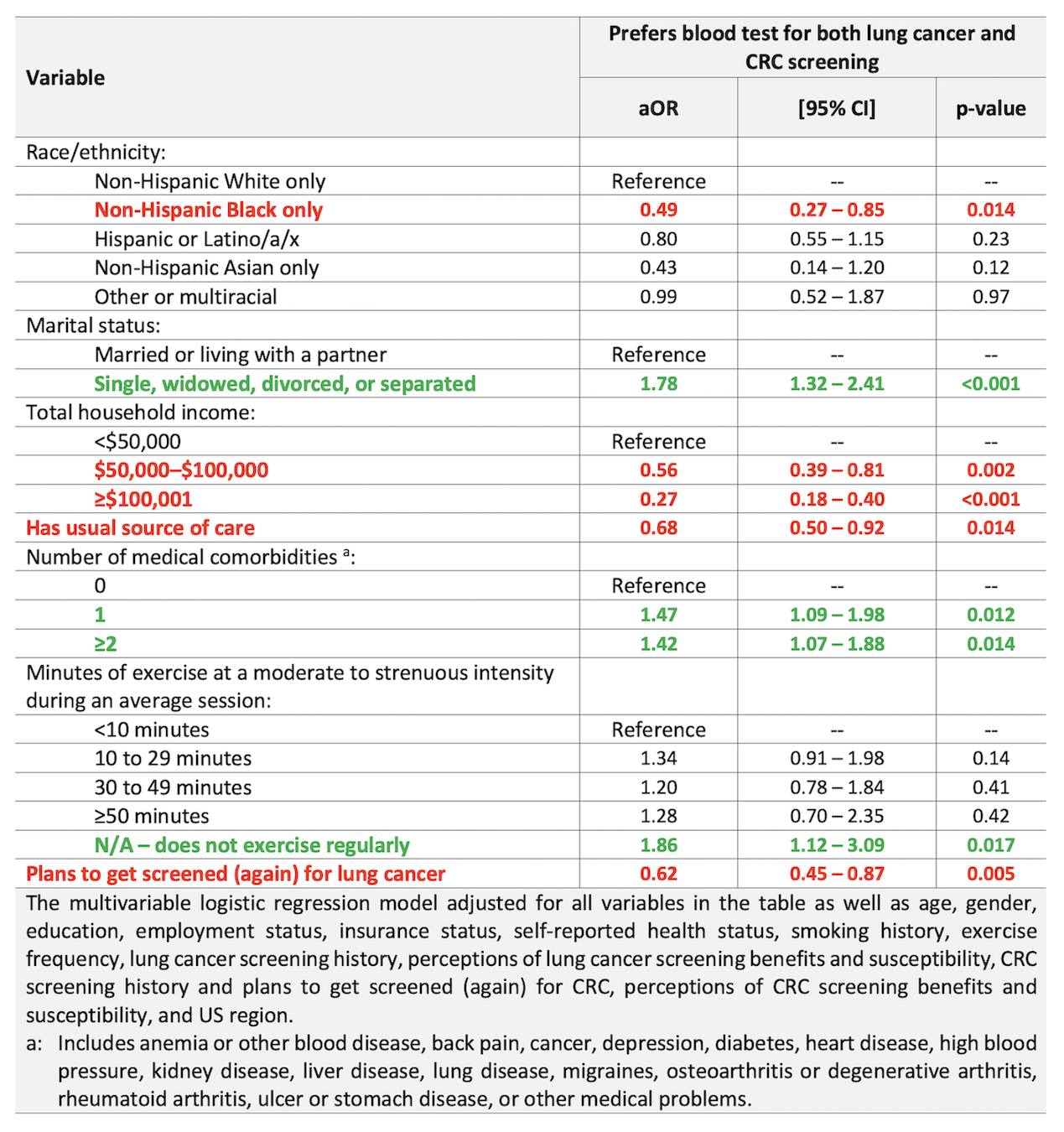
Figure: FIGURE. Data from simulations using conjoint analysis data assessing the proportion of respondents who would prefer each lung cancer and CRC screening test combination (ie, blood tests for both cancers, blood test for one and traditional for the other, or traditional tests for both) (N=1,741).
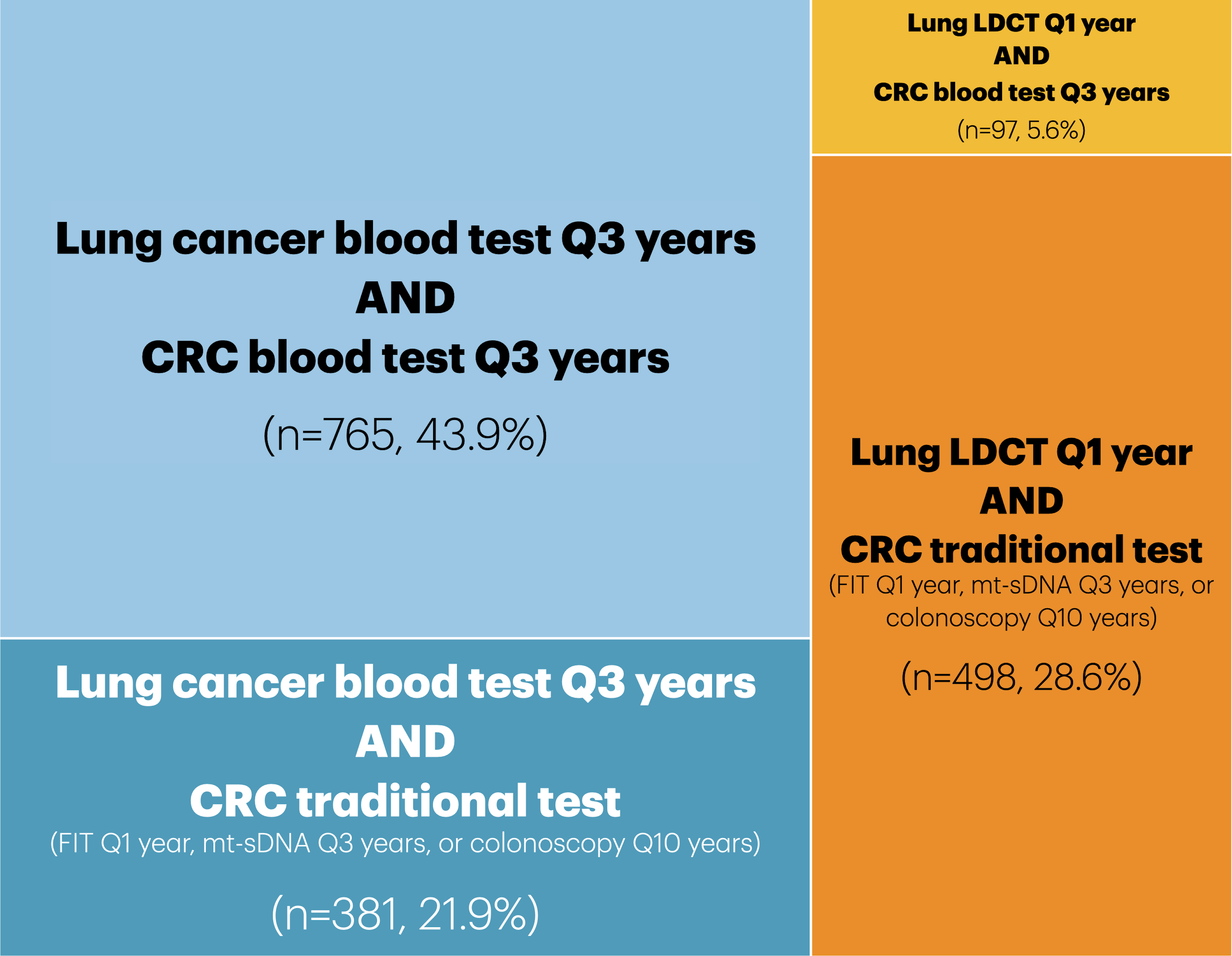
Figure: TABLE. Regression analysis on preferring a blood test for both lung cancer and CRC screening.
Disclosures:
Jan Ballesteros indicated no relevant financial relationships.
Ayako Ikenouchi indicated no relevant financial relationships.
So Yung Choi indicated no relevant financial relationships.
Allistair Clark indicated no relevant financial relationships.
Brennan Spiegel: Exact Sciences – Consultant. Freenome – Consultant. Guardant Health – Consultant.
Christopher Almario: Exact Sciences – Consultant. Freenome – Grant/Research Support. Guardant Health – Grant/Research Support.
Jan Ballesteros, PhD, Ayako Ikenouchi, MD, So Yung Choi, MS, Allistair Clark, MA, Brennan Spiegel, MD, MSHS, Christopher Almario, MD, MSHPM. P4744 - Assessing Patient Preferences for Blood-Based Lung Cancer and Colorectal Cancer Screening Tests: Insights from a Conjoint Analysis with over 1,700 People in the US, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Cedars-Sinai Medical Center, Los Angeles, CA
Introduction: Over 80% of people who smoke nicotine are not up-to-date with lung cancer screening, and more than 40% of eligible adults are not current with colorectal cancer (CRC) screening. Blood-based tests for both cancers offer a promising alternative to existing options. In this study, we used conjoint analysis to assess preferences for blood-based lung and CRC screening tests compared to traditional methods (e.g., low-dose CT [LDCT] for lung cancer; fecal immunochemical test [FIT], multitarget stool DNA [mt-sDNA], and colonoscopy for CRC).
Methods: We conducted a choice-based conjoint survey of US adults aged 50–75 years who were eligible but not up-to-date for lung and CRC screening per USPSTF guidelines. In the conjoint exercises, participants evaluated side-by-side hypothetical lung cancer and CRC screening test combinations that varied by modality, frequency, accuracy, and other features. We used hierarchical Bayes regression to estimate individual part-worth utilities, which were then used to conduct simulations assessing respondents’ preferred lung cancer and CRC screening test combinations: blood tests for both cancers, blood test for one and traditional for the other, or traditional tests for both. Multivariable logistic regression adjusted for confounding and identified factors associated with preferring blood-based screening for both cancers.
Results: A total of 1,741 participants completed the survey. As shown in the Figure, 43.9% of respondents preferred to do blood tests every 3 (Q3) years for both cancers, while 28.6% favored traditional options. Another 21.9% preferred a lung cancer blood test Q3 years with a traditional CRC test; 5.6% chose annual lung LDCT with a CRC blood test Q3 years. Regression results (Table) showed that non-married individuals, those with comorbidities, and those who do not exercise regularly were more likely to prefer blood tests to screen for both cancers (all p< 0.05). In contrast, non-Hispanic Black individuals with higher income, and those with a usual source of care were less likely to choose blood testing (all p< 0.05).
Discussion: Among a national sample of individuals not up-to-date with lung and CRC screening, nearly half preferred blood tests for both cancers over traditional methods. These findings suggest that blood-based screening is broadly acceptable and may help address barriers to participation in cancer screening programs.
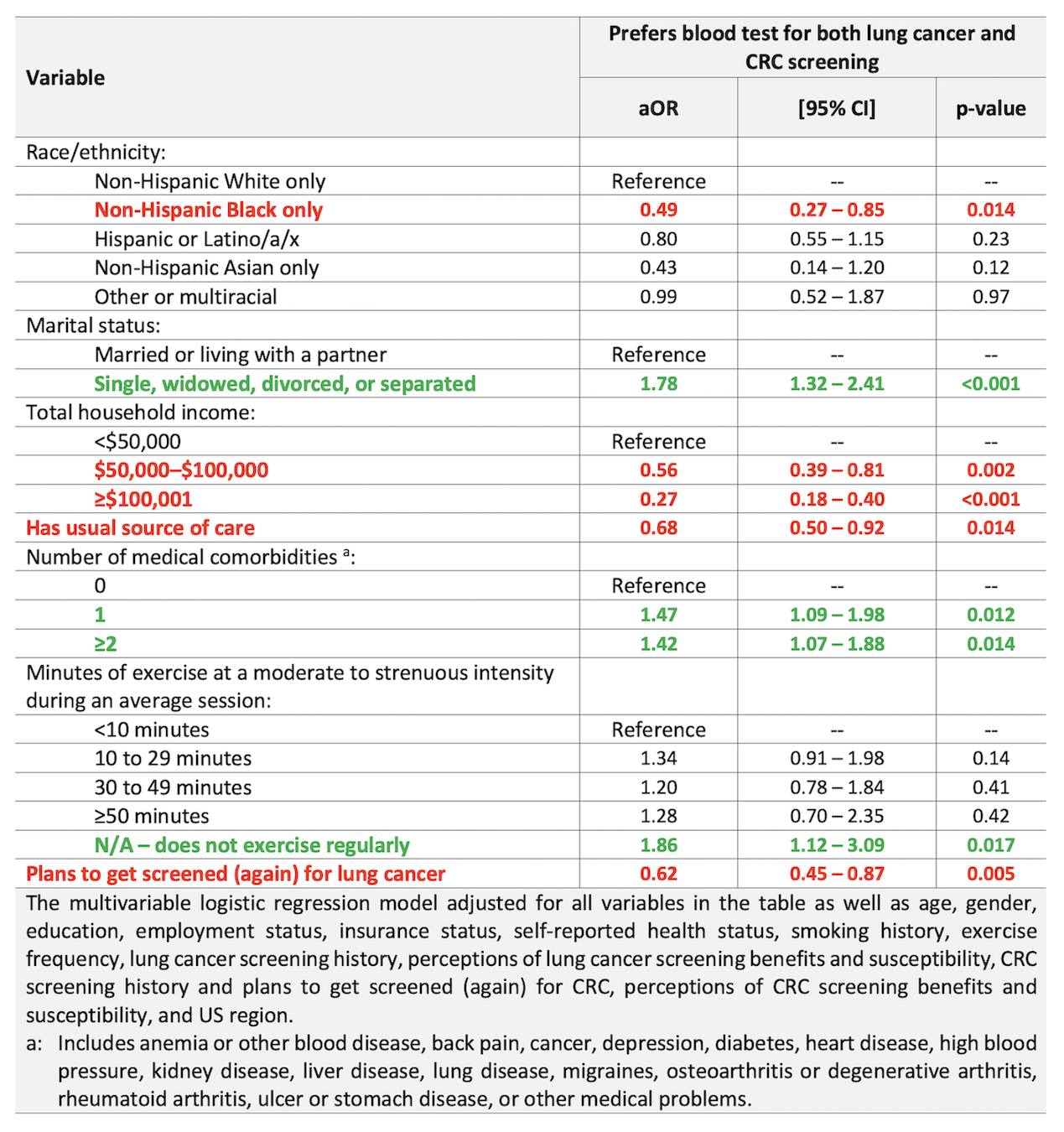
Figure: FIGURE. Data from simulations using conjoint analysis data assessing the proportion of respondents who would prefer each lung cancer and CRC screening test combination (ie, blood tests for both cancers, blood test for one and traditional for the other, or traditional tests for both) (N=1,741).
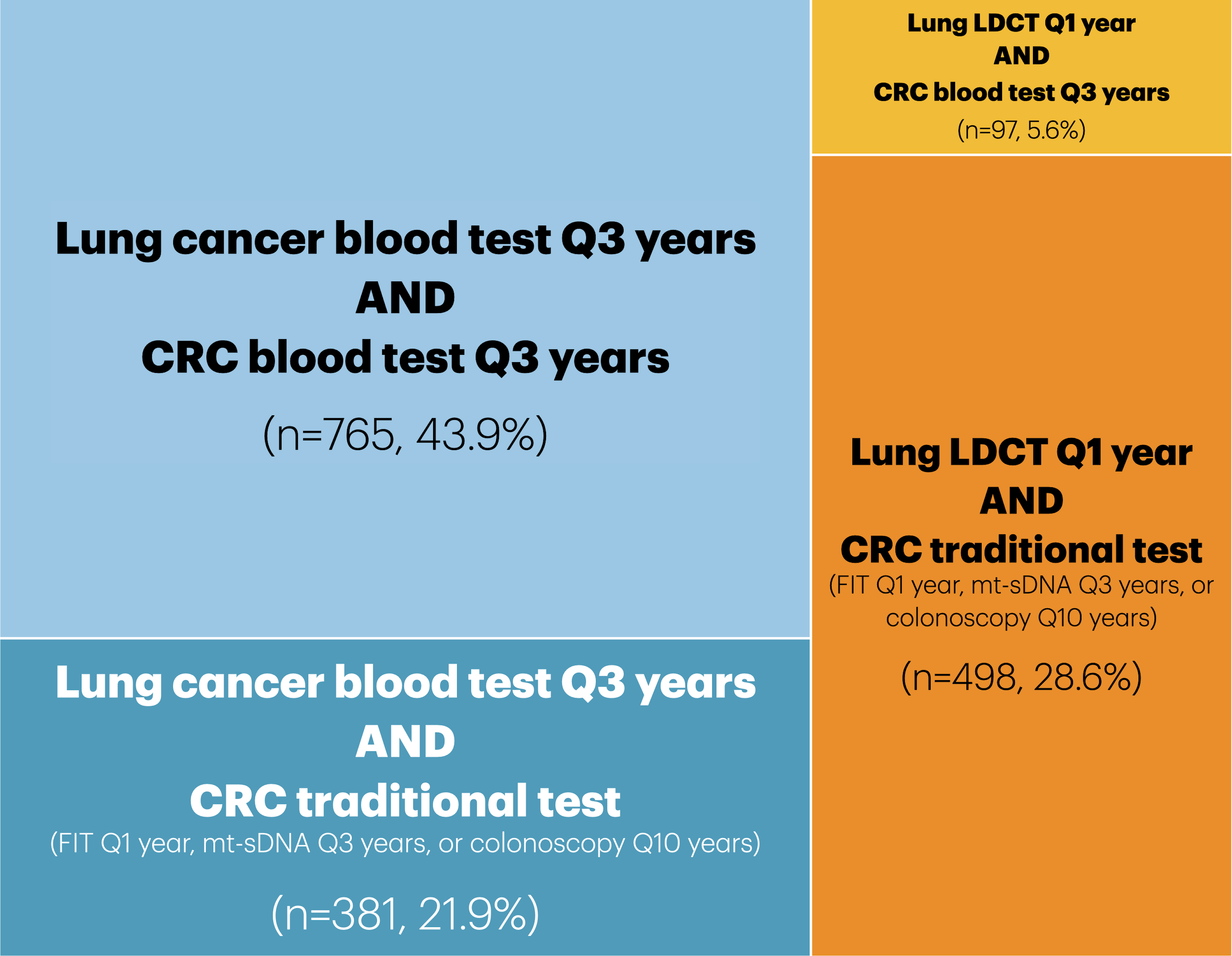
Figure: TABLE. Regression analysis on preferring a blood test for both lung cancer and CRC screening.
Disclosures:
Jan Ballesteros indicated no relevant financial relationships.
Ayako Ikenouchi indicated no relevant financial relationships.
So Yung Choi indicated no relevant financial relationships.
Allistair Clark indicated no relevant financial relationships.
Brennan Spiegel: Exact Sciences – Consultant. Freenome – Consultant. Guardant Health – Consultant.
Christopher Almario: Exact Sciences – Consultant. Freenome – Grant/Research Support. Guardant Health – Grant/Research Support.
Jan Ballesteros, PhD, Ayako Ikenouchi, MD, So Yung Choi, MS, Allistair Clark, MA, Brennan Spiegel, MD, MSHS, Christopher Almario, MD, MSHPM. P4744 - Assessing Patient Preferences for Blood-Based Lung Cancer and Colorectal Cancer Screening Tests: Insights from a Conjoint Analysis with over 1,700 People in the US, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

