Tuesday Poster Session
Category: Colon
P4712 - A Serious Turn: Bowel Perforation Secondary to Semaglutide-Induced Constipation
- ZS
Zainab Saeed, MD (she/her/hers)
Houston Methodist Hospital
Houston, TX
Presenting Author(s)
1Houston Methodist Hospital, Houston, TX; 2Gujranwala Medical College, Punjab Pakistan, Gujranwala, Punjab, Pakistan; 3HCA Healthcare Kingwood Hospital/University of Houston, Houston, TX; 4HCA Healthcare, Houston, TX
Introduction: GLP-1 receptor agonists (GLP-1 RAs) are gaining popularity among patients and physicians due to their impressive benefits for type II DM and weight loss. Some known gastrointestinal side effects of GLP-1 RA include pancreatitis, biliary disease, abdominal pain, nausea, vomiting, diarrhea, or mild constipation. The risk of severe sequelae such as bowel perforation remains unsubstantiated in available evidence.
Case Description/
Methods:
A 63-year-old lady with a past medical history of type II diabetes mellitus, hyperlipidemia, and diverticulosis presented with chief complaint of two weeks of worsening abdominal pain associated with nausea and vomiting. The patient reported being on Semaglutide for the past 4 months, starting at 0.25mg weekly and currently at 1.7mg weekly.
She reported constipation since starting this medication, with bowel movements occurring once every 4-5 days. However, for the last 4 weeks, she has not had any bowel movements. However, she was able to pass flatus.
On admission, the patient was tachycardiac and hypotensive, with an elevated white blood cell count and lactic acidosis. Physical examination revealed a distended abdomen with absent bowel sounds. A CT scan of the abdomen showed colonic perforation with extravasation of stool, pneumoperitoneum, peritoneal wall thickening, and a large volume of stool burden throughout the entire colon.
The patient underwent an exploratory laparotomy, sigmoid colon resection due to distal mid colon perforation, with Hartmann’s pouch and colostomy creation. Attempts to milk out hard stool intraoperatively were unsuccessful as it caused further mucosal damage to the remaining colon. Patient remained on broad spectrum antibiotics while in hospital and later required IR guided drain placement for intra-abdominal loculated fluid collections. Patient was eventually discharged home.
Discussion: Gastrointestinal side effects of GLP-1 RA are mild and rarely cause medication discontinuation by patients. The current clinical guidelines focus on slow titration of medication and patient education to GI side effects. Even though constipation is a common side effect, the risk of severe sequelae such as bowel perforation is not established. Clinicians must be cognizant of the potential for sever constipation and educate patients about the importance of closely monitoring bowel movements and seeking timely intervention for constipation to prevent catastrophic events, especially in the elderly.
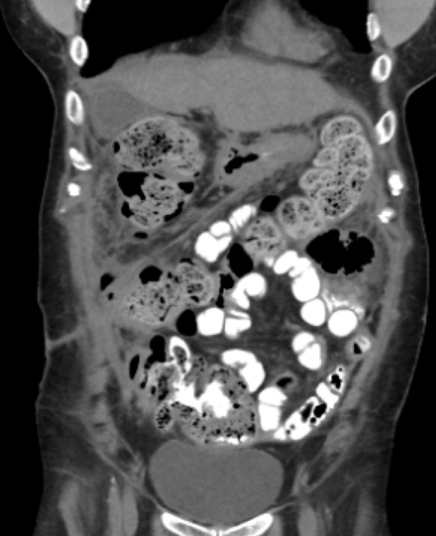
Figure: Large stool burden.
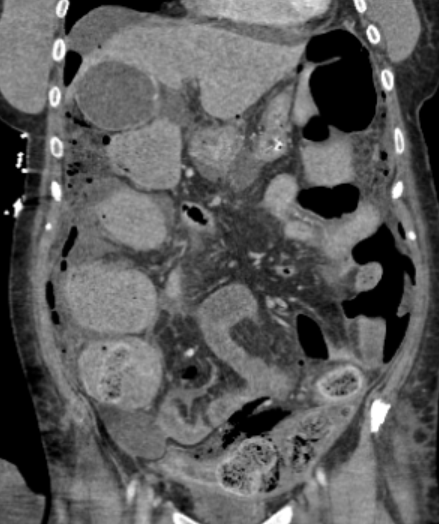
Figure: Pneumoperitoneum.
Disclosures:
Zainab Saeed indicated no relevant financial relationships.
Minahil Batool indicated no relevant financial relationships.
Bilal Ashraf indicated no relevant financial relationships.
Aakriti Soni indicated no relevant financial relationships.
Galvin Dhaliwal indicated no relevant financial relationships.
Pragnesh Patel indicated no relevant financial relationships.
Zainab Saeed, MD1, Minahil Batool, 2, Bilal Ashraf, MD3, Aakriti Soni, MD3, Galvin S. Dhaliwal, MD3, Pragnesh Patel, MD4. P4712 - A Serious Turn: Bowel Perforation Secondary to Semaglutide-Induced Constipation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
