Tuesday Poster Session
Category: Colon
P4690 - When Benign Becomes Serious: Colonic Lipoma Causing Intussusception
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- CH
Cody Hu, MD
University of Texas Health San Antonio
San Antonio, TX
Presenting Author(s)
Cody Hu, MD, Andrew Han, MD, Michelle Conde, MD
University of Texas Health San Antonio, San Antonio, TX
Introduction: Colonic lipomas are benign tumors composed of adipose tissue, which are commonly asymptomatic. Here, we present a case of colonic intussusception caused by a giant colonic lipoma and its management.
Case Description/
Methods: A 59-year-old female with hypertension and history of tobacco use presented to the ER for acute sharp abdominal pain at bilateral lower quadrants over the past 8 days. The pain was associated with nausea and hematochezia. On arrival, her vitals were normal, and physical exam was significant for the tenderness to palpation in the left lower quadrant with no rebounding characteristic. Labs revealed normal hemoglobin, lactic acid, and electrolytes. CT abdomen disclosed a left-sided colonic intussusception with a 5 cm ovoid intraluminal fat density mass which was a lead point and represented a colonic lipoma. Surgery and GI were consulted in the ER, and colonoscopy was urgently done on the following day for endoscopic reduction and mucosa evaluation (image 1). Although the colo-colonic intussusception was successfully reduced, patient developed nausea and abdominal pain the day after colonoscopy. Repeated CT demonstrated recurrent colo-colonic intussusception. The patient was subsequently taken for partial colectomy (image 2). Postoperative course was uneventful, and she was discharged following tolerance of an oral diet.
Discussion: Colonic lipomas are often an incidental finding during endoscopic evaluation or imaging studies. The uniform fat density of the lipomas, without any solid component, makes them readily distinguishable on CT and MRI. This feature also underlies the “pillow sign” observed on endoscopy—an indentation on the lesion when pressed with biopsy forceps. It has a 98% specificity, but sensitivity is only limited to 40%. While frequently asymptomatic, giant colonic lipomas—measuring over 4 cm—become symptomatic in approximately 75% of cases. Colonic intussusception is a rare but serious complication of colonic lipomas. In this case, surgery team recommended endoscopic intervention with the hope of achieving therapeutic resection. However, due to the high risk of perforation, absence of pillow sign, and ulceration at the base of stalk, it was not removed with endoscopy. Surgical operation is the first-line treatment option in her circumstance due to the large size. Endoscopic reduction as a bridge to definitive surgical operation to optimize preoperative status highlights the importance of the multidisciplinary approach in managing complicated colonic lipomas.
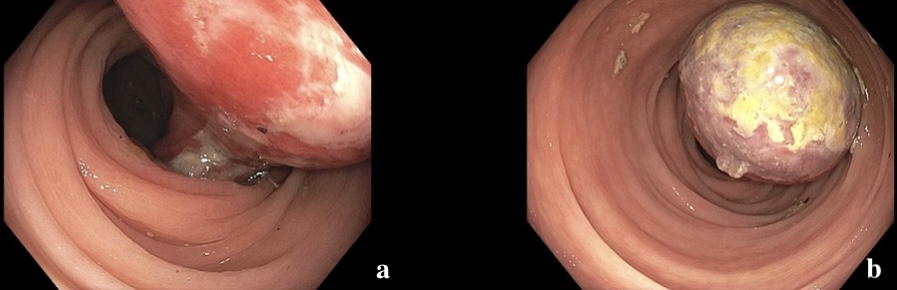
Figure: Image 1: a) A pedunculated, 5 cm mass with surface ulceration and exudates reaching to the base of the stalk. b) The lesion caused nearly complete obstruction of the lumen, but air and liquid were able to pass after reduction of the intussusception. Pillow sign was negative. No evidence of mucosal ischemia. Intra-procedurally, due to the atypical features, including negative pillow and ulceration, it was not removed with endoscopy.

Figure: Image 2: Surgical specimen demonstrating a large submucosal lipoma with surface ulceration and neighboring colonic tissue.
Disclosures:
Cody Hu indicated no relevant financial relationships.
Andrew Han indicated no relevant financial relationships.
Michelle Conde indicated no relevant financial relationships.
Cody Hu, MD, Andrew Han, MD, Michelle Conde, MD. P4690 - When Benign Becomes Serious: Colonic Lipoma Causing Intussusception, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Texas Health San Antonio, San Antonio, TX
Introduction: Colonic lipomas are benign tumors composed of adipose tissue, which are commonly asymptomatic. Here, we present a case of colonic intussusception caused by a giant colonic lipoma and its management.
Case Description/
Methods: A 59-year-old female with hypertension and history of tobacco use presented to the ER for acute sharp abdominal pain at bilateral lower quadrants over the past 8 days. The pain was associated with nausea and hematochezia. On arrival, her vitals were normal, and physical exam was significant for the tenderness to palpation in the left lower quadrant with no rebounding characteristic. Labs revealed normal hemoglobin, lactic acid, and electrolytes. CT abdomen disclosed a left-sided colonic intussusception with a 5 cm ovoid intraluminal fat density mass which was a lead point and represented a colonic lipoma. Surgery and GI were consulted in the ER, and colonoscopy was urgently done on the following day for endoscopic reduction and mucosa evaluation (image 1). Although the colo-colonic intussusception was successfully reduced, patient developed nausea and abdominal pain the day after colonoscopy. Repeated CT demonstrated recurrent colo-colonic intussusception. The patient was subsequently taken for partial colectomy (image 2). Postoperative course was uneventful, and she was discharged following tolerance of an oral diet.
Discussion: Colonic lipomas are often an incidental finding during endoscopic evaluation or imaging studies. The uniform fat density of the lipomas, without any solid component, makes them readily distinguishable on CT and MRI. This feature also underlies the “pillow sign” observed on endoscopy—an indentation on the lesion when pressed with biopsy forceps. It has a 98% specificity, but sensitivity is only limited to 40%. While frequently asymptomatic, giant colonic lipomas—measuring over 4 cm—become symptomatic in approximately 75% of cases. Colonic intussusception is a rare but serious complication of colonic lipomas. In this case, surgery team recommended endoscopic intervention with the hope of achieving therapeutic resection. However, due to the high risk of perforation, absence of pillow sign, and ulceration at the base of stalk, it was not removed with endoscopy. Surgical operation is the first-line treatment option in her circumstance due to the large size. Endoscopic reduction as a bridge to definitive surgical operation to optimize preoperative status highlights the importance of the multidisciplinary approach in managing complicated colonic lipomas.
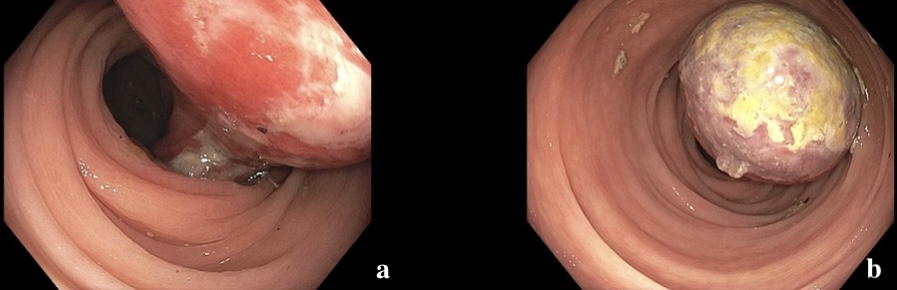
Figure: Image 1: a) A pedunculated, 5 cm mass with surface ulceration and exudates reaching to the base of the stalk. b) The lesion caused nearly complete obstruction of the lumen, but air and liquid were able to pass after reduction of the intussusception. Pillow sign was negative. No evidence of mucosal ischemia. Intra-procedurally, due to the atypical features, including negative pillow and ulceration, it was not removed with endoscopy.

Figure: Image 2: Surgical specimen demonstrating a large submucosal lipoma with surface ulceration and neighboring colonic tissue.
Disclosures:
Cody Hu indicated no relevant financial relationships.
Andrew Han indicated no relevant financial relationships.
Michelle Conde indicated no relevant financial relationships.
Cody Hu, MD, Andrew Han, MD, Michelle Conde, MD. P4690 - When Benign Becomes Serious: Colonic Lipoma Causing Intussusception, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
