Tuesday Poster Session
Category: Colon
P4634 - Cronkhite–Canada Syndrome, a Diagnosis Challenge and Management With Vedolizumab
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- AN
Aida Nasirishargh, MD
University of California Davis Health
Sacramento, CA
Presenting Author(s)
Aida Nasirishargh, MD1, Robert L. Pecha, MD2, Ashna Aggarwal, MD1, Dongguang Wei, MD1, Kurt Schaberg, MD1, Eric J. Mao, MD3
1University of California Davis Health, Sacramento, CA; 2UC Davis Division of GI and Hepatology, Sacramento, CA; 3UC Davis School of Medicine, Sacramento, CA
Introduction: Cronkhite–Canada syndrome (CCS) is a rare, nonhereditary gastrointestinal (GI) polyposis syndrome characterized by diffuse polyps, diarrhea, malnutrition, and ectodermal symptoms. There is no single confirmatory test for CCS; rather, the diagnosis is based on a combination of clinical, laboratory, endoscopic, radiologic, and histopathologic findings. Here we present a case of CCS that was initially thought to be Crohn’s disease, managed with vedolizumab for lower GI symptoms, and ultimately required total parenteral nutrition (TPN ) due to severe malnutrition.
Case Description/
Methods: A 65-year-old man presented with 2 months of progressive watery diarrhea (10 episodes per day), 25 lb weight loss, early satiety, and postprandial abdominal pain. He reported a persistent “greasy, foul” taste and new-onset nail dystrophy affecting all digits. He had a positive Cologuard test, and fecal calprotectin was elevated at 2,160. Abdominal CT showed mild wall thickening in the descending colon. Colonoscopy revealed cobblestoning and nodular mucosa from the terminal ileum to the rectum. Histology showed chronic inflammation with eosinophilia (Figure 1). Diagnosed with Crohn’s disease, he was started on prednisone and vedolizumab, with initial symptom improvement and weight gain. However, by month 8, he developed worsening anorexia, dysgeusia, and weight loss. His diarrhea had improved to 3-4 times per day. Despite an increase in vedolizumab frequency, the symptoms persisted. Follow-up EGD showed large nodular gastric and duodenal polyps (Figure 2). Biopsies revealed epithelial hyperplasia and mucosal edema. Colonoscopy confirmed widespread inflammatory polyps with rectal sparing. In a multidisciplinary review with input from GI, pathology, radiology, and colorectal surgery, the clinical picture was deemed more consistent with CCS rather than Crohn’s disease. Vedolizumab was continued due to partial symptomatic relief. Endoscopic or surgical gastrostomy was deferred due to extensive gastric involvement and malnutrition. He was hospitalized for anasarca and hypoalbuminemia (albumin 2.3 g/dL), and initiated on TPN.
Discussion: This case highlights the diagnostic complexity and clinical severity of CCS that can closely mimic Inflammatory Bowel Disease. Despite a partial response to vedolizumab, the progression of the disease led to severe malnutrition requiring TPN. Early recognition and multidisciplinary management are critical in CCS to avoid complications and improve outcomes in this debilitating condition.
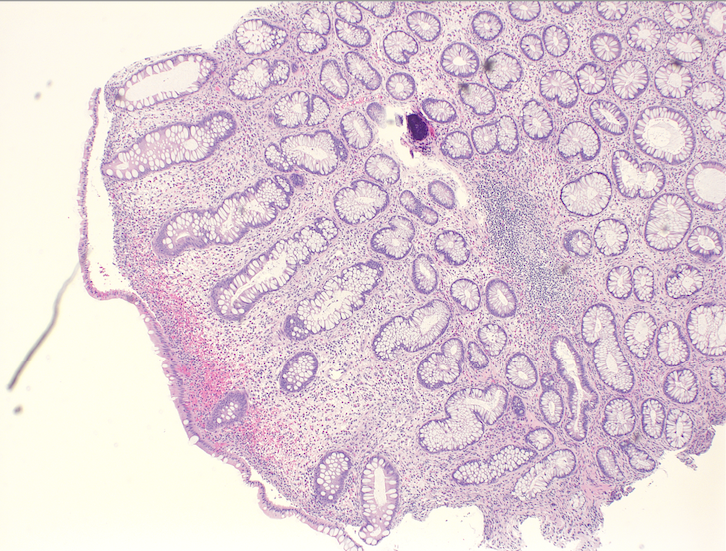
Figure: Figure 1. The sigmoid colon shows tortuous glands with lamina propria edema and eosinophils
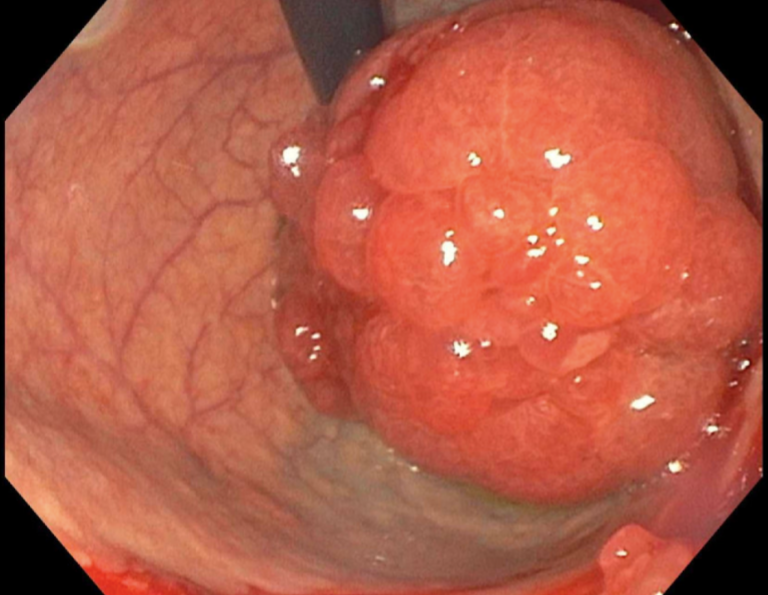
Figure: Figure 2. Mass and nodular mucosa of duodenal bulb
Disclosures:
Aida Nasirishargh indicated no relevant financial relationships.
Robert Pecha indicated no relevant financial relationships.
Ashna Aggarwal indicated no relevant financial relationships.
Dongguang Wei indicated no relevant financial relationships.
Kurt Schaberg indicated no relevant financial relationships.
Eric Mao indicated no relevant financial relationships.
Aida Nasirishargh, MD1, Robert L. Pecha, MD2, Ashna Aggarwal, MD1, Dongguang Wei, MD1, Kurt Schaberg, MD1, Eric J. Mao, MD3. P4634 - Cronkhite–Canada Syndrome, a Diagnosis Challenge and Management With Vedolizumab, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of California Davis Health, Sacramento, CA; 2UC Davis Division of GI and Hepatology, Sacramento, CA; 3UC Davis School of Medicine, Sacramento, CA
Introduction: Cronkhite–Canada syndrome (CCS) is a rare, nonhereditary gastrointestinal (GI) polyposis syndrome characterized by diffuse polyps, diarrhea, malnutrition, and ectodermal symptoms. There is no single confirmatory test for CCS; rather, the diagnosis is based on a combination of clinical, laboratory, endoscopic, radiologic, and histopathologic findings. Here we present a case of CCS that was initially thought to be Crohn’s disease, managed with vedolizumab for lower GI symptoms, and ultimately required total parenteral nutrition (TPN ) due to severe malnutrition.
Case Description/
Methods: A 65-year-old man presented with 2 months of progressive watery diarrhea (10 episodes per day), 25 lb weight loss, early satiety, and postprandial abdominal pain. He reported a persistent “greasy, foul” taste and new-onset nail dystrophy affecting all digits. He had a positive Cologuard test, and fecal calprotectin was elevated at 2,160. Abdominal CT showed mild wall thickening in the descending colon. Colonoscopy revealed cobblestoning and nodular mucosa from the terminal ileum to the rectum. Histology showed chronic inflammation with eosinophilia (Figure 1). Diagnosed with Crohn’s disease, he was started on prednisone and vedolizumab, with initial symptom improvement and weight gain. However, by month 8, he developed worsening anorexia, dysgeusia, and weight loss. His diarrhea had improved to 3-4 times per day. Despite an increase in vedolizumab frequency, the symptoms persisted. Follow-up EGD showed large nodular gastric and duodenal polyps (Figure 2). Biopsies revealed epithelial hyperplasia and mucosal edema. Colonoscopy confirmed widespread inflammatory polyps with rectal sparing. In a multidisciplinary review with input from GI, pathology, radiology, and colorectal surgery, the clinical picture was deemed more consistent with CCS rather than Crohn’s disease. Vedolizumab was continued due to partial symptomatic relief. Endoscopic or surgical gastrostomy was deferred due to extensive gastric involvement and malnutrition. He was hospitalized for anasarca and hypoalbuminemia (albumin 2.3 g/dL), and initiated on TPN.
Discussion: This case highlights the diagnostic complexity and clinical severity of CCS that can closely mimic Inflammatory Bowel Disease. Despite a partial response to vedolizumab, the progression of the disease led to severe malnutrition requiring TPN. Early recognition and multidisciplinary management are critical in CCS to avoid complications and improve outcomes in this debilitating condition.
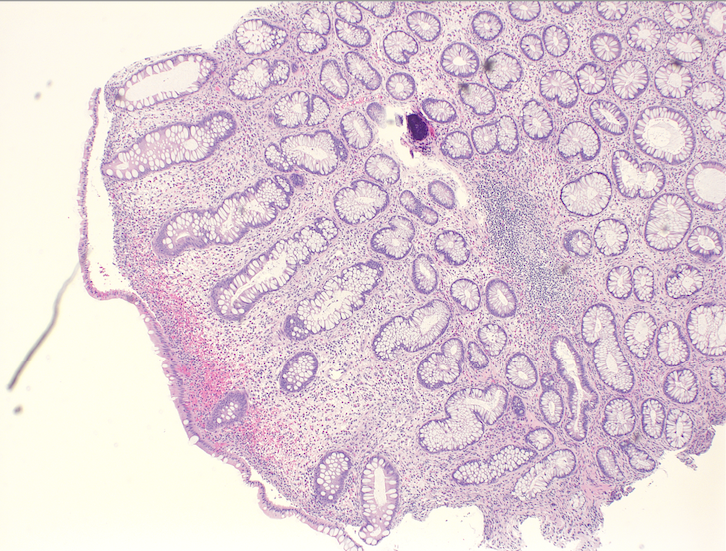
Figure: Figure 1. The sigmoid colon shows tortuous glands with lamina propria edema and eosinophils
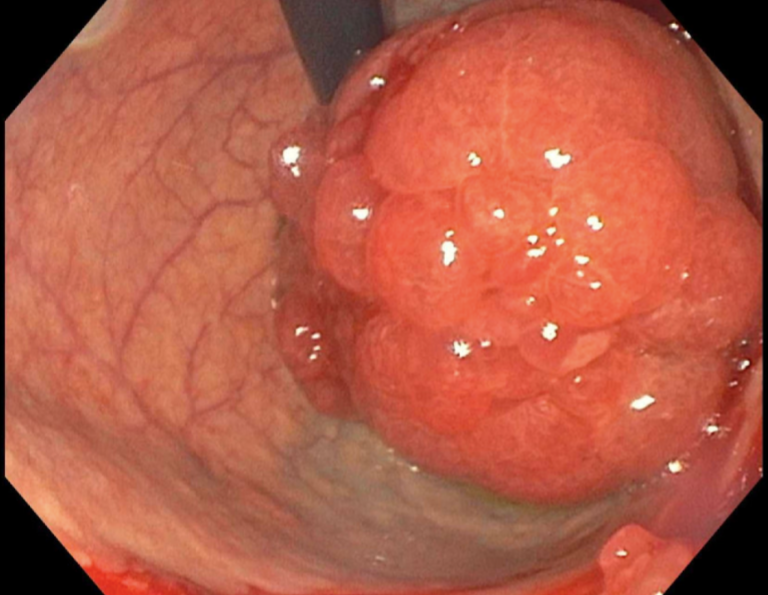
Figure: Figure 2. Mass and nodular mucosa of duodenal bulb
Disclosures:
Aida Nasirishargh indicated no relevant financial relationships.
Robert Pecha indicated no relevant financial relationships.
Ashna Aggarwal indicated no relevant financial relationships.
Dongguang Wei indicated no relevant financial relationships.
Kurt Schaberg indicated no relevant financial relationships.
Eric Mao indicated no relevant financial relationships.
Aida Nasirishargh, MD1, Robert L. Pecha, MD2, Ashna Aggarwal, MD1, Dongguang Wei, MD1, Kurt Schaberg, MD1, Eric J. Mao, MD3. P4634 - Cronkhite–Canada Syndrome, a Diagnosis Challenge and Management With Vedolizumab, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
