Tuesday Poster Session
Category: Liver
P5981 - Hepar Lobatum Carcinomatosum: Two Cases of Pseudocirrhosis in Metastatic Cancer
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- LS
Laith Sorour, MD
Ascension Saint Francis Hospital
Evanston, IL
Presenting Author(s)
Laith Sorour, MD1, Tasneem Anagreh, MD1, Hieu Truong, MD1, Ben Varghese, MD1, Muhammad Ahsan. Siddiqui, MD1, Bhargav Koyani, MD1, Rajvi Pathak, MBBS2
1Ascension Saint Francis Hospital, Evanston, IL; 2GMERS Medical College and Hospital Sola, Ahmedabad, Gujarat, India
Introduction: Pseudocirrhosis refers to hepatic changes on imaging that resemble cirrhosis, typically occurring in patients with liver metastases undergoing chemotherapy. It is most often described in breast cancer and is commonly associated with platinum agents and taxanes. Pseudocirrhosis may lead to complications of portal hypertension, including ascites, variceal bleeding, and hepatorenal syndrome. We present two cases of rapidly progressive pseudocirrhosis with poor outcomes.
Case Description/
Methods: Case 1: A 79-year-old woman with metastatic colon cancer to the liver and bone, on bevacizumab, 5-fluorouracil, and oxaliplatin, presented with abdominal distention and leg edema. Labs showed hypoalbuminemia, mild hyperbilirubinemia, and INR 2.3. CT revealed stable liver metastases but new nodular liver morphology and large-volume ascites. Imaging three months earlier showed decreased lesion size without cirrhotic features. In the absence of liver disease, findings were attributed to pseudocirrhosis. Her course was complicated by spontaneous bacterial peritonitis, hepatorenal syndrome, and liver failure, leading to death within two weeks.
Case 2: A 72-year-old woman with ER/PR-positive metastatic breast cancer and recurrent liver metastases had received multiple therapies, including doxorubicin, cyclophosphamide, paclitaxel, gemcitabine, and fam-trastuzumab deruxtecan. She presented with fatigue, fever, and abdominal pain. Labs showed pancytopenia, hypoalbuminemia, elevated bilirubin, and INR 1.6. Imaging showed new cirrhotic features, portal colopathy, and ascites not present five months earlier. She improved briefly with antibiotics and vasopressors but was readmitted with worsening symptoms. Paracentesis revealed sterile transudate. She deteriorated due to shock and multiorgan failure.
Discussion: Pseudocirrhosis is an underrecognized complication of cancer therapy. It may result from chemotherapy-induced liver injury, tumor regression with fibrotic remodeling, or sinusoidal obstruction. It mimics cirrhosis radiologically and clinically, though it often progresses more rapidly and lacks the traditional etiologies of chronic liver disease. Early recognition is critical, as discontinuing the offending agents may reverse changes in some cases. These cases highlight the risk of rapid deterioration. Management should follow cirrhosis guidelines, including variceal screening and ascites control. Further research is needed to define drug-specific risks and develop monitoring strategies for high-risk patients.
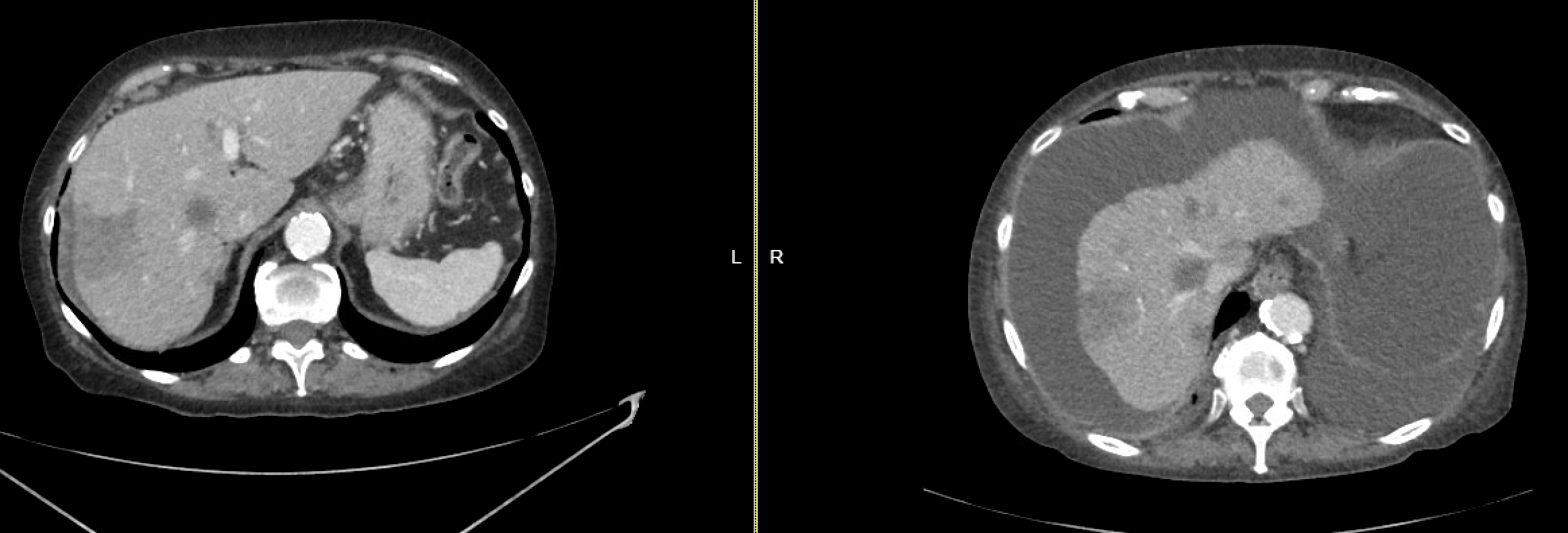
Figure: Case 1: Liver changes over 3 months
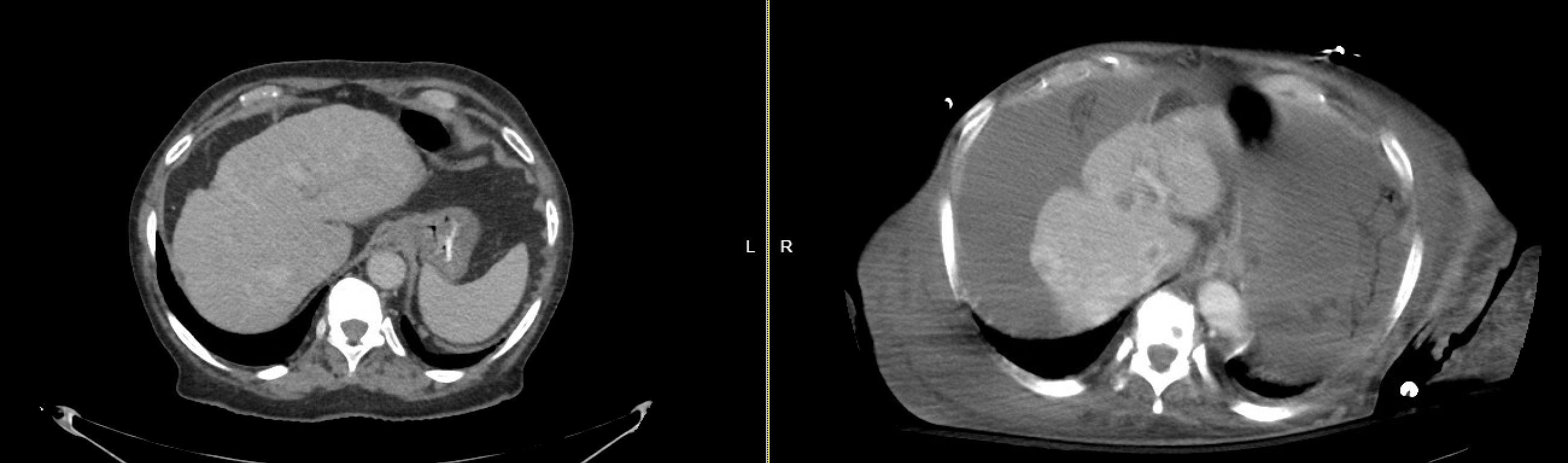
Figure: Case 2: Liver changes over 5 months
Disclosures:
Laith Sorour indicated no relevant financial relationships.
Tasneem Anagreh indicated no relevant financial relationships.
Hieu Truong indicated no relevant financial relationships.
Ben Varghese indicated no relevant financial relationships.
Muhammad Siddiqui indicated no relevant financial relationships.
Bhargav Koyani indicated no relevant financial relationships.
Rajvi Pathak indicated no relevant financial relationships.
Laith Sorour, MD1, Tasneem Anagreh, MD1, Hieu Truong, MD1, Ben Varghese, MD1, Muhammad Ahsan. Siddiqui, MD1, Bhargav Koyani, MD1, Rajvi Pathak, MBBS2. P5981 - Hepar Lobatum Carcinomatosum: Two Cases of Pseudocirrhosis in Metastatic Cancer, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Ascension Saint Francis Hospital, Evanston, IL; 2GMERS Medical College and Hospital Sola, Ahmedabad, Gujarat, India
Introduction: Pseudocirrhosis refers to hepatic changes on imaging that resemble cirrhosis, typically occurring in patients with liver metastases undergoing chemotherapy. It is most often described in breast cancer and is commonly associated with platinum agents and taxanes. Pseudocirrhosis may lead to complications of portal hypertension, including ascites, variceal bleeding, and hepatorenal syndrome. We present two cases of rapidly progressive pseudocirrhosis with poor outcomes.
Case Description/
Methods: Case 1: A 79-year-old woman with metastatic colon cancer to the liver and bone, on bevacizumab, 5-fluorouracil, and oxaliplatin, presented with abdominal distention and leg edema. Labs showed hypoalbuminemia, mild hyperbilirubinemia, and INR 2.3. CT revealed stable liver metastases but new nodular liver morphology and large-volume ascites. Imaging three months earlier showed decreased lesion size without cirrhotic features. In the absence of liver disease, findings were attributed to pseudocirrhosis. Her course was complicated by spontaneous bacterial peritonitis, hepatorenal syndrome, and liver failure, leading to death within two weeks.
Case 2: A 72-year-old woman with ER/PR-positive metastatic breast cancer and recurrent liver metastases had received multiple therapies, including doxorubicin, cyclophosphamide, paclitaxel, gemcitabine, and fam-trastuzumab deruxtecan. She presented with fatigue, fever, and abdominal pain. Labs showed pancytopenia, hypoalbuminemia, elevated bilirubin, and INR 1.6. Imaging showed new cirrhotic features, portal colopathy, and ascites not present five months earlier. She improved briefly with antibiotics and vasopressors but was readmitted with worsening symptoms. Paracentesis revealed sterile transudate. She deteriorated due to shock and multiorgan failure.
Discussion: Pseudocirrhosis is an underrecognized complication of cancer therapy. It may result from chemotherapy-induced liver injury, tumor regression with fibrotic remodeling, or sinusoidal obstruction. It mimics cirrhosis radiologically and clinically, though it often progresses more rapidly and lacks the traditional etiologies of chronic liver disease. Early recognition is critical, as discontinuing the offending agents may reverse changes in some cases. These cases highlight the risk of rapid deterioration. Management should follow cirrhosis guidelines, including variceal screening and ascites control. Further research is needed to define drug-specific risks and develop monitoring strategies for high-risk patients.
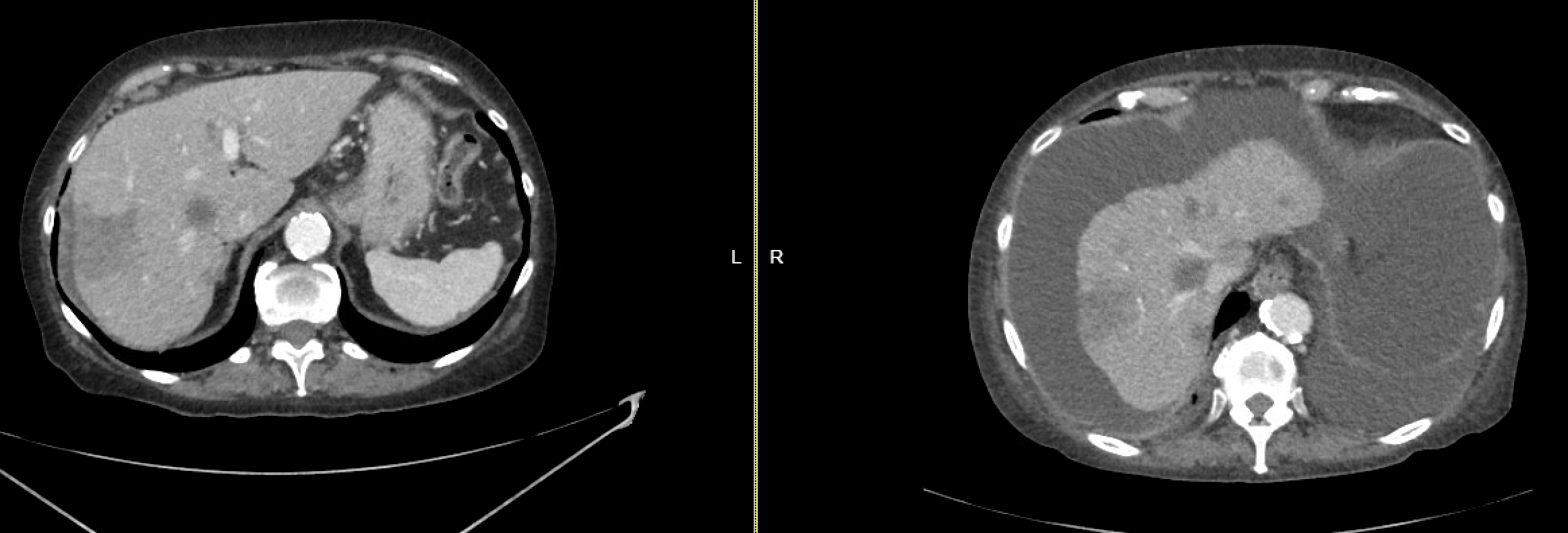
Figure: Case 1: Liver changes over 3 months
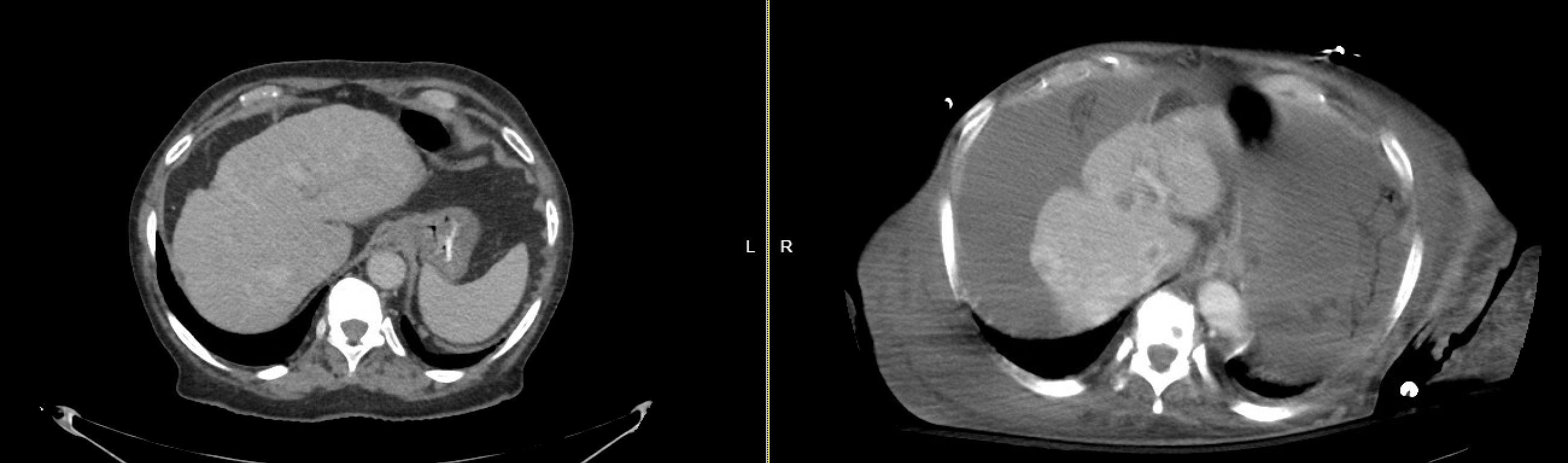
Figure: Case 2: Liver changes over 5 months
Disclosures:
Laith Sorour indicated no relevant financial relationships.
Tasneem Anagreh indicated no relevant financial relationships.
Hieu Truong indicated no relevant financial relationships.
Ben Varghese indicated no relevant financial relationships.
Muhammad Siddiqui indicated no relevant financial relationships.
Bhargav Koyani indicated no relevant financial relationships.
Rajvi Pathak indicated no relevant financial relationships.
Laith Sorour, MD1, Tasneem Anagreh, MD1, Hieu Truong, MD1, Ben Varghese, MD1, Muhammad Ahsan. Siddiqui, MD1, Bhargav Koyani, MD1, Rajvi Pathak, MBBS2. P5981 - Hepar Lobatum Carcinomatosum: Two Cases of Pseudocirrhosis in Metastatic Cancer, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
