Tuesday Poster Session
Category: Liver
Unmasking a Hidden Parasite: Colonic Necrosis and Liver Abscess From <i>Entamoeba histolytica</i>
P5976 - Unmasking a Hidden Parasite: Colonic Necrosis and Liver Abscess From Entamoeba histolytica
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mohamad Omar Diab, MD (he/him/his)
Canyon Vista Medical Center
Sierra Vista, AZ
Presenting Author(s)
Samuel Cheong, DO1, Mohamad Omar Diab, MD2, Maxwell Hart, MD1, Brandon Witten, MD3, Rolando J. Leal, MD4
1University of Arizona College of Medicine, Tucson, AZ; 2Canyon Vista Medical Center, Sierra Vista, AZ; 3Banner - University of Arizona Tucson, Tucson, AZ; 4Banner University Medical Center, Tucson, AZ
Introduction: Entamoeba histolytica (EH) is a parasitic protozoan transmitted via the fecal-oral route, with amebic liver abscess as its most common extraintestinal manifestation. We present a rare case of a perforated EH liver abscess.
Case Description/
Methods: A 63-year-old male with hypertension and recent travel to Mexico presented with an 8-day history of fever, diarrhea, and worsening diffuse abdominal pain. Initial CT of the abdomen and pelvis (A/P) revealed mass-like thickening from the ascending to proximal transverse colon, involving the appendix. The liver appeared normal without focal lesions. Despite bowel rest and empiric broad-spectrum antibiotics, there was no clinical improvement. The patient underwent a right hemicolectomy with end ileostomy. On postoperative day 2, he remained tachycardic with worsening leukocytosis. Repeat CT A/P showed new multiple bi-lobar hepatic abscesses (1–3 cm) and a large peri-colonic abscess (14.5 × 6.9 × 9.8 cm) in the right colon bed. Infectious Disease and Interventional Radiology were consulted. Intravenous Unasyn and Flagyl were initiated, and a CT-guided drain was placed into the peri-colonic abscess. Histopathology of the resected colon specimen confirmed Entamoeba histolytica as the causative organism, leading to colonic necrosis. The patient improved with therapy. Prior to discharge, the peri-colonic drain was removed. He was discharged to a skilled nursing facility with a PICC line for intravenous Unasyn and oral metronidazole and paromomycin.
Discussion: Entamoeba histolytica infection ranges from asymptomatic colonization to life-threatening complications such as amebic liver abscess, intestinal perforation, and sepsis. Our case highlights an unusual presentation of EH with colonic involvement and delayed development of hepatic abscesses following colonic perforation. This emphasizes the need to consider EH in patients with compatible symptoms and travel history to endemic areas. Prompt diagnosis and a multidisciplinary approach - encompassing infectious disease, radiology, and surgery - are crucial to reduce morbidity and mortality. Awareness of such rare presentations is essential for timely management and to prevent further complications.
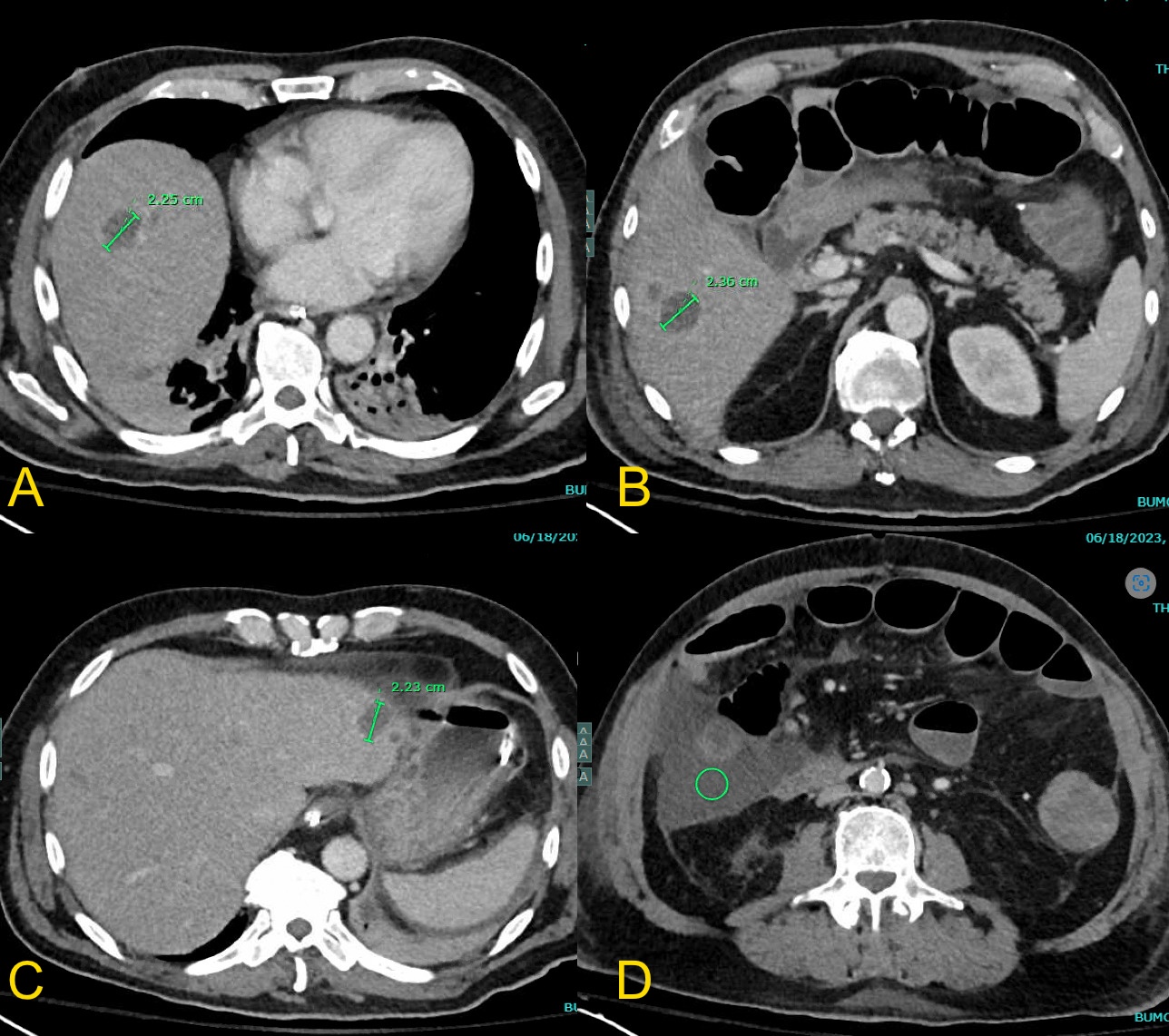
Figure: Figures A, B and C: CT - Abdomen and Pelvis revealing multiple livers abscess.
Figure D: Pericolonic abscess in the right colon bed measuring 14.5 × 6.9 × 9.8 cm.

Figure: Figure A: H&E staining showing necrotic colon tissue with E. histolytica and diffusely ingested with RBC's.
Figure B: RBC's ingested within the E. histolytica involving necrosis.
Figure C: Zoomed out histology slide of the necrosis.
Figure D: Gangrenous transmural necrosis with E. histolytica
Disclosures:
Samuel Cheong indicated no relevant financial relationships.
Mohamad Omar Diab indicated no relevant financial relationships.
Maxwell Hart indicated no relevant financial relationships.
Brandon Witten indicated no relevant financial relationships.
Rolando Leal indicated no relevant financial relationships.
Samuel Cheong, DO1, Mohamad Omar Diab, MD2, Maxwell Hart, MD1, Brandon Witten, MD3, Rolando J. Leal, MD4. P5976 - Unmasking a Hidden Parasite: Colonic Necrosis and Liver Abscess From <i>Entamoeba histolytica</i>, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Arizona College of Medicine, Tucson, AZ; 2Canyon Vista Medical Center, Sierra Vista, AZ; 3Banner - University of Arizona Tucson, Tucson, AZ; 4Banner University Medical Center, Tucson, AZ
Introduction: Entamoeba histolytica (EH) is a parasitic protozoan transmitted via the fecal-oral route, with amebic liver abscess as its most common extraintestinal manifestation. We present a rare case of a perforated EH liver abscess.
Case Description/
Methods: A 63-year-old male with hypertension and recent travel to Mexico presented with an 8-day history of fever, diarrhea, and worsening diffuse abdominal pain. Initial CT of the abdomen and pelvis (A/P) revealed mass-like thickening from the ascending to proximal transverse colon, involving the appendix. The liver appeared normal without focal lesions. Despite bowel rest and empiric broad-spectrum antibiotics, there was no clinical improvement. The patient underwent a right hemicolectomy with end ileostomy. On postoperative day 2, he remained tachycardic with worsening leukocytosis. Repeat CT A/P showed new multiple bi-lobar hepatic abscesses (1–3 cm) and a large peri-colonic abscess (14.5 × 6.9 × 9.8 cm) in the right colon bed. Infectious Disease and Interventional Radiology were consulted. Intravenous Unasyn and Flagyl were initiated, and a CT-guided drain was placed into the peri-colonic abscess. Histopathology of the resected colon specimen confirmed Entamoeba histolytica as the causative organism, leading to colonic necrosis. The patient improved with therapy. Prior to discharge, the peri-colonic drain was removed. He was discharged to a skilled nursing facility with a PICC line for intravenous Unasyn and oral metronidazole and paromomycin.
Discussion: Entamoeba histolytica infection ranges from asymptomatic colonization to life-threatening complications such as amebic liver abscess, intestinal perforation, and sepsis. Our case highlights an unusual presentation of EH with colonic involvement and delayed development of hepatic abscesses following colonic perforation. This emphasizes the need to consider EH in patients with compatible symptoms and travel history to endemic areas. Prompt diagnosis and a multidisciplinary approach - encompassing infectious disease, radiology, and surgery - are crucial to reduce morbidity and mortality. Awareness of such rare presentations is essential for timely management and to prevent further complications.
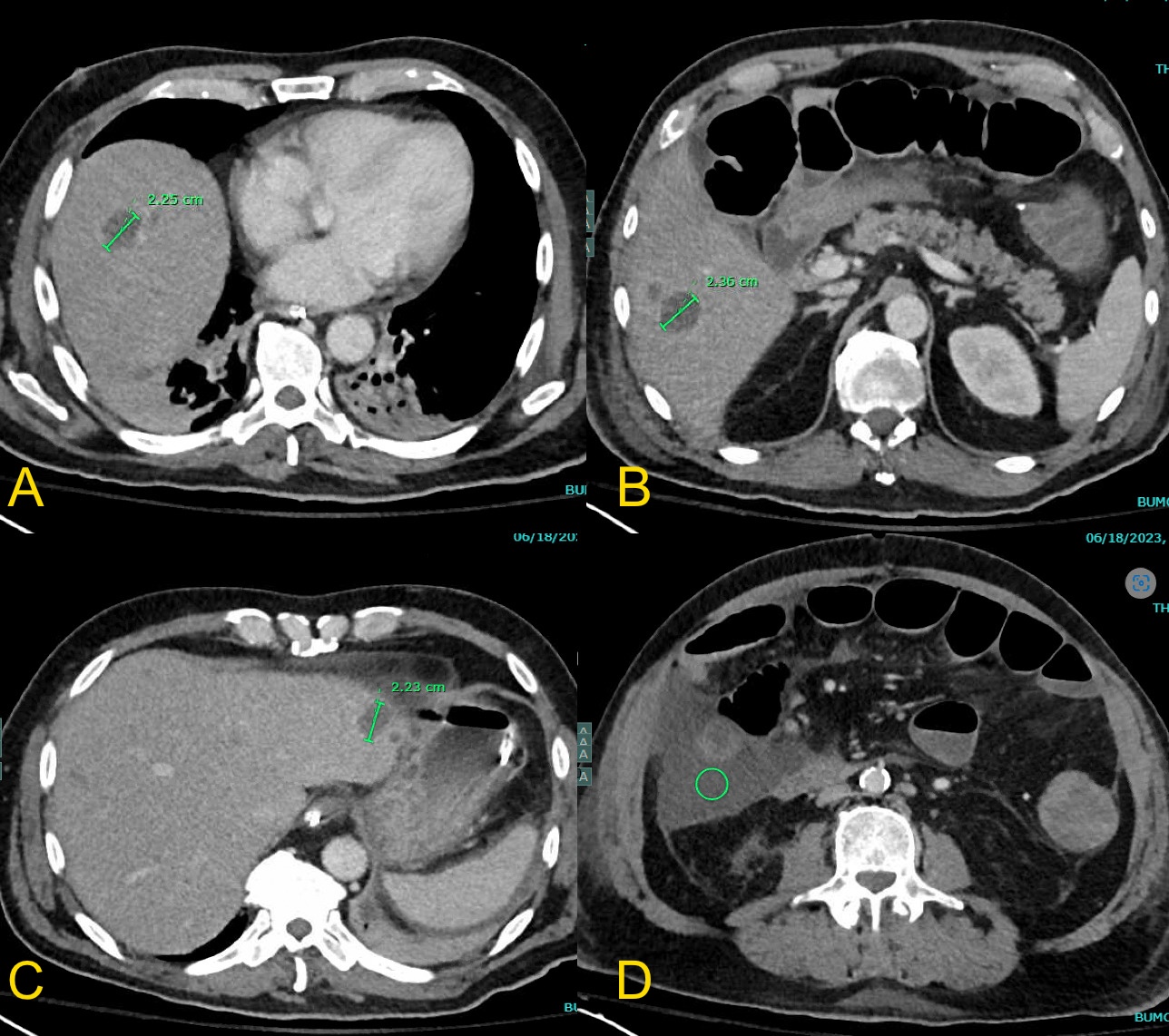
Figure: Figures A, B and C: CT - Abdomen and Pelvis revealing multiple livers abscess.
Figure D: Pericolonic abscess in the right colon bed measuring 14.5 × 6.9 × 9.8 cm.

Figure: Figure A: H&E staining showing necrotic colon tissue with E. histolytica and diffusely ingested with RBC's.
Figure B: RBC's ingested within the E. histolytica involving necrosis.
Figure C: Zoomed out histology slide of the necrosis.
Figure D: Gangrenous transmural necrosis with E. histolytica
Disclosures:
Samuel Cheong indicated no relevant financial relationships.
Mohamad Omar Diab indicated no relevant financial relationships.
Maxwell Hart indicated no relevant financial relationships.
Brandon Witten indicated no relevant financial relationships.
Rolando Leal indicated no relevant financial relationships.
Samuel Cheong, DO1, Mohamad Omar Diab, MD2, Maxwell Hart, MD1, Brandon Witten, MD3, Rolando J. Leal, MD4. P5976 - Unmasking a Hidden Parasite: Colonic Necrosis and Liver Abscess From <i>Entamoeba histolytica</i>, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
