Tuesday Poster Session
Category: Liver
P6053 - Transient Cortical Blindness in the Setting of Hepatic Encephalopathy: An Unforeseen Outcome Following Transjugular Intrahepatic Portosystemic Shunt Placement
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Gabriella R. Cascio, BS (she/her/hers)
Wayne State University School of Medicine
Detroit, MI
Presenting Author(s)
Award: ACG Presidential Poster Award
Gabriella R. Cascio, BS1, Reena Salgia, MD2, Omar Shamaa, MD2, Jonathan A. Montrose, DO2
1Wayne State University School of Medicine, Detroit, MI; 2Henry Ford Health, Detroit, MI
Introduction: Hepatic encephalopathy (HE) is characterized by an array of neuropsychiatric abnormalities resulting from the accumulation of neurotoxic substances in the bloodstream of patients with liver dysfunction. The incidence of HE after Transjugular Intrahepatic Portosystemic Shunt (TIPS) placement is as high as 20–50%. Here we present a rare case of transient cortical blindness secondary to HE in a patient who underwent TIPS.
Case Description/
Methods: A 63-year-old male with cirrhosis secondary to hepatitis C virus presented to the hospital for new onset melena, hematemesis, and anemia with hemoglobin of 6.3 g/dL. He was transferred to the ICU and underwent an EGD revealing large esophageal varices with overlying fibrin clots. The varices were not amenable to treatment with band ligation, thus a Minnesota tube was placed. Ammonia was 254 μg/dL, for which he was started on lactulose and rifaximin. He underwent TIPS placement with resolution of variceal bleeding. Minnesota tube was removed, followed by extubation and eventual discharge on lactulose and rifaximin.
The patient presented to the hospital one week later due to new onset hepatic encephalopathy, visual blindness, and agitation, despite reported medication adherence. Hepatology and interventional radiology were consulted for consideration of TIPS reversal. Abdominal ultrasound revealed patent TIPS with velocities of 169-206 cm/s. Ophthalmology and neurology were consulted to assess the patient’s new onset cortical blindness. The patient had no response to an optokinetic drum held immediately in front of his eyes at bedside. His eyes were exhibiting esotropia with downward gaze. CT head was obtained showing distended optic nerve sheath complexes and diffuse leukoencephalopathy, both secondary to hyperammonemia. Treatment with lactulose and rifaximin was continued, with improvement of hepatic encephalopathy and complete reversal of blindness within days. His mentation and vision improved with medical management alone, and he was deemed medically stable for discharge.
Discussion: This case highlights cortical blindness as an uncommon but serious complication of HE following TIPS. Awareness of this presentation is essential, as early medical intervention may prevent permanent visual impairment and obviate the need for TIPS revision. Further studies are warranted to understand the pathophysiology and optimal management of this rare complication.
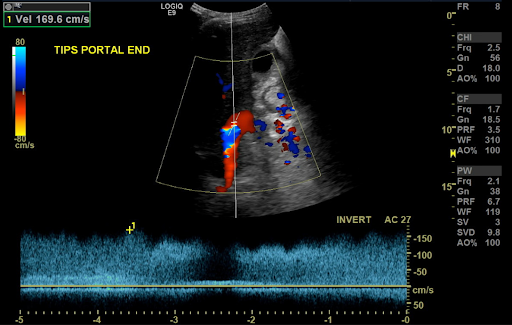
Figure: Abdominal ultrasound with Doppler demonstrating patent TIPS
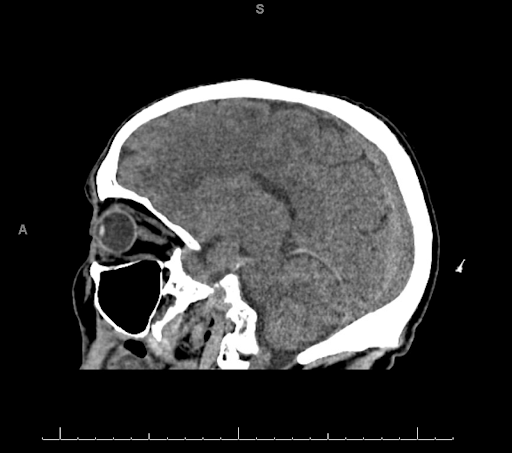
Figure: CT Head demonstrating distended optic nerve sheath complexes and diffuse leukoencephalopathy
Disclosures:
Gabriella Cascio indicated no relevant financial relationships.
Reena Salgia indicated no relevant financial relationships.
Omar Shamaa indicated no relevant financial relationships.
Jonathan Montrose indicated no relevant financial relationships.
Gabriella R. Cascio, BS1, Reena Salgia, MD2, Omar Shamaa, MD2, Jonathan A. Montrose, DO2. P6053 - Transient Cortical Blindness in the Setting of Hepatic Encephalopathy: An Unforeseen Outcome Following Transjugular Intrahepatic Portosystemic Shunt Placement, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Gabriella R. Cascio, BS1, Reena Salgia, MD2, Omar Shamaa, MD2, Jonathan A. Montrose, DO2
1Wayne State University School of Medicine, Detroit, MI; 2Henry Ford Health, Detroit, MI
Introduction: Hepatic encephalopathy (HE) is characterized by an array of neuropsychiatric abnormalities resulting from the accumulation of neurotoxic substances in the bloodstream of patients with liver dysfunction. The incidence of HE after Transjugular Intrahepatic Portosystemic Shunt (TIPS) placement is as high as 20–50%. Here we present a rare case of transient cortical blindness secondary to HE in a patient who underwent TIPS.
Case Description/
Methods: A 63-year-old male with cirrhosis secondary to hepatitis C virus presented to the hospital for new onset melena, hematemesis, and anemia with hemoglobin of 6.3 g/dL. He was transferred to the ICU and underwent an EGD revealing large esophageal varices with overlying fibrin clots. The varices were not amenable to treatment with band ligation, thus a Minnesota tube was placed. Ammonia was 254 μg/dL, for which he was started on lactulose and rifaximin. He underwent TIPS placement with resolution of variceal bleeding. Minnesota tube was removed, followed by extubation and eventual discharge on lactulose and rifaximin.
The patient presented to the hospital one week later due to new onset hepatic encephalopathy, visual blindness, and agitation, despite reported medication adherence. Hepatology and interventional radiology were consulted for consideration of TIPS reversal. Abdominal ultrasound revealed patent TIPS with velocities of 169-206 cm/s. Ophthalmology and neurology were consulted to assess the patient’s new onset cortical blindness. The patient had no response to an optokinetic drum held immediately in front of his eyes at bedside. His eyes were exhibiting esotropia with downward gaze. CT head was obtained showing distended optic nerve sheath complexes and diffuse leukoencephalopathy, both secondary to hyperammonemia. Treatment with lactulose and rifaximin was continued, with improvement of hepatic encephalopathy and complete reversal of blindness within days. His mentation and vision improved with medical management alone, and he was deemed medically stable for discharge.
Discussion: This case highlights cortical blindness as an uncommon but serious complication of HE following TIPS. Awareness of this presentation is essential, as early medical intervention may prevent permanent visual impairment and obviate the need for TIPS revision. Further studies are warranted to understand the pathophysiology and optimal management of this rare complication.
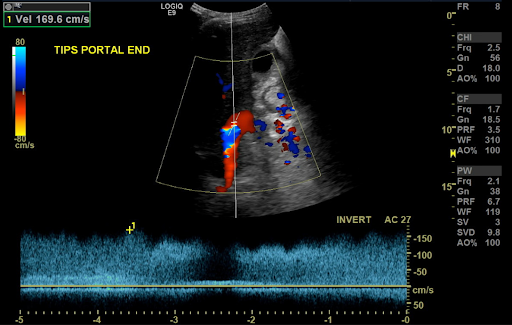
Figure: Abdominal ultrasound with Doppler demonstrating patent TIPS
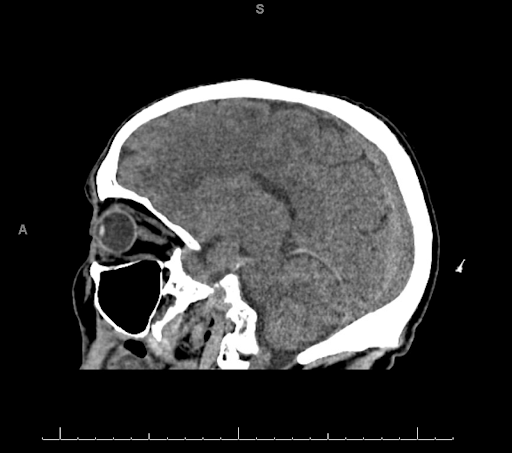
Figure: CT Head demonstrating distended optic nerve sheath complexes and diffuse leukoencephalopathy
Disclosures:
Gabriella Cascio indicated no relevant financial relationships.
Reena Salgia indicated no relevant financial relationships.
Omar Shamaa indicated no relevant financial relationships.
Jonathan Montrose indicated no relevant financial relationships.
Gabriella R. Cascio, BS1, Reena Salgia, MD2, Omar Shamaa, MD2, Jonathan A. Montrose, DO2. P6053 - Transient Cortical Blindness in the Setting of Hepatic Encephalopathy: An Unforeseen Outcome Following Transjugular Intrahepatic Portosystemic Shunt Placement, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

