Tuesday Poster Session
Category: Liver
P6050 - Multilobulated Bilomas as a Late Complication of Remote Cholecystectomy: A Diagnostic Challenge in a Patient With Chronic Abdominal Pain
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Olga Karina Morales, MD
Texas Institute for Graduate Medical Education and Research
San Antonio, TX
Presenting Author(s)
Olga Karina K. Morales, MD1, Ussama Ghumman, MD2, Lisa D. Pedicone, PhD3, Eugenia K. Tsai, MD2, Fred Poordad, MD2, Fabian Rodas, MD2, Eric Lawitz, MD4, Jan Petrasek, MD2, Andres Gomez-Aldana, MD3
1Texas Institute for Graduate Medical Education and Research, San Antonio, TX; 2University of Texas Health San Antonio, San Antonio, TX; 3Texas Liver Institute, Austin, TX; 4Texas Liver Institute, San Antonio, TX
Introduction: Bilomas are localized collections of bile outside the biliary system, resulting from iatrogenic or traumatic bile duct injury. They typically present within days to two weeks following hepatobiliary procedures. Delayed manifestations are rare and underreported. Incidence of delayed bilomas is < 0.1%, with extremely few cases occurring decades after cholecystectomy.
Case Description/
Methods: A 49 yo female with a history of hypertension, hypothyroidism, gastroparesis and peptic ulcer disease, presented with bilateral upper quadrant abdominal pain over several months. She had a remote cholecystectomy >20 years ago. Abdominal pain was associated with nausea but no vomiting, diarrhea, jaundice or food related symptoms. Labs showed WBC 17.05, elevated AST/ALT 58/62, elevated ALP 306 and lipase 43. Contrast CT revealed new, poorly defined hypodense lesions in the right hepatic lobe, measuring 8.9 cm in segments V and VIII concerning for malignancy (Figure 1). MRCP showed T2 hyperintense, lobulated lesions, measuring 14.6 cm (Figure 2). Findings raised concern for lobulated, hepatic cystic lesions with bilomas considered in the differential diagnosis. IR aspirated 15 mL of green bile and cytology showed degenerative debris without malignancy. A biliary drain catheter was placed yielding an initial 250 mL of bile. The catheter remained in place continuously draining for 3 month and posteriorly self-resolved with residual hepatic necrotic tissue.
Discussion: Delayed presentation of bilomas occurring decades after cholecystectomy is exceptionally rare and not initially considered in the differential diagnosis of hepatic cystic lesions. The remote history of cholecystectomy >20 years ago, contributed to the delayed recognition of biloma as a possible etiology. In this case the underlying mechanism for delayed formation remains speculative. Proposed theories include micro rupture of an accessory bile duct or pressure related biliary compromise from conditions such as gastroparesis or peptic ulcer disease. MRCP findings, IR aspiration of bile and exclusion of malignancy, confirmed the diagnosis. While small, asymptomatic bilomas may resolve spontaneously, larger or symptomatic collections typically require IR percutaneous drainage. In refractory cases or those with persistent bile leaks, ERCP with stenting may be indicated. In this case, percutaneous drainage led to symptom resolution and provided definitive diagnosis.

Figure: Figure 1,T2 weighted MRCP sequence showing multilobulated hyperintense fluid collection within hepatic segment V and VIII consistent with biloma.
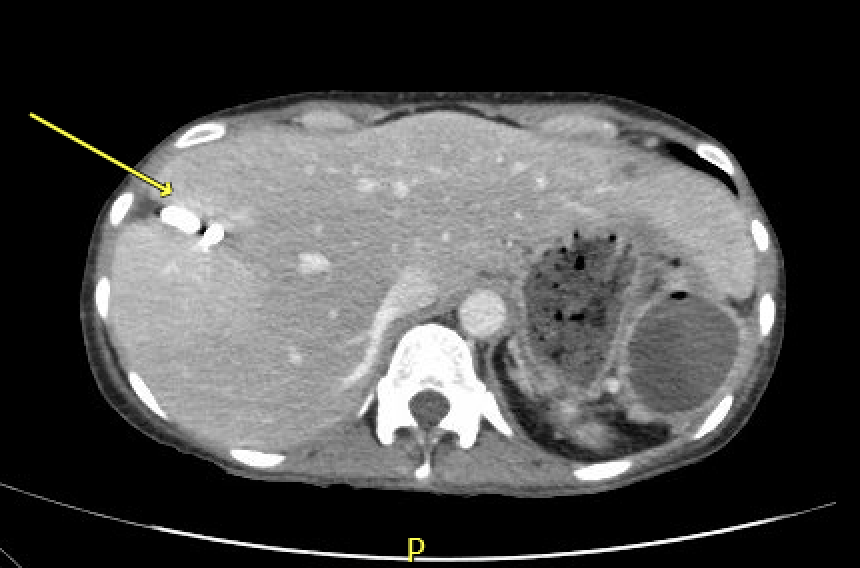
Figure: Figure 2, Abdomen CT w/wo contrast, yellow arrow showing drain in the right hepatic lobe with resolution of the previously visualized biloma.
Disclosures:
Olga Karina Morales indicated no relevant financial relationships.
Ussama Ghumman indicated no relevant financial relationships.
Lisa D. Pedicone indicated no relevant financial relationships.
Eugenia Tsai indicated no relevant financial relationships.
Fred Poordad indicated no relevant financial relationships.
Fabian Rodas indicated no relevant financial relationships.
Eric Lawitz: 89 Bio INC – Consultant, Grant/Research Support, Speakers Bureau. Abbvie – Speakers Bureau. Akero Therapeitics – Grant/Research Support. Alnylam Phamaceuticals INC – Grant/Research Support. Amgen – Grant/Research Support. Aztrazeneca – Consultant, Grant/Research Support. Bioscience – Grant/Research Support. Boehringer Ingelheim – Consultant, Grant/Research Support. Bristol-Myers Squibb – Grant/Research Support. Corcept Therapeutics – Consultant, Grant/Research Support. Cour Pharmaceuticals Inc – Grant/Research Support. Cymabay Therapeutics – Grant/Research Support. Eli Lily and Company – Consultant, Grant/Research Support. Enanta Pharmaceuticals – Grant/Research Support. Enyo Pharma – Grant/Research Support. Exalenz – Grant/Research Support. Galectin Therapeutics – Grant/Research Support. Galmed Pharmaceuticals – Grant/Research Support. Genfit – Grant/Research Support. Gilead Sciences – Grant/Research Support, Speakers Bureau. GlaxoSmithKline – Grant/Research Support. Hanmi Pharmaceuticals – Grant/Research Support. Hightide Biopharma – Grant/Research Support. Intercept Pharmaceuticals – Grant/Research Support, Speakers Bureau. Inventiva – Grant/Research Support. Ipsen – Grant/Research Support. Jansen Pharmaceuticals – Grant/Research Support. Madrigal Pharmaceuticals – Grant/Research Support, Speakers Bureau. Merck & Co – Consultant, Grant/Research Support. NGM Biopharmaceuticals Inc – Grant/Research Support. Northsea Therapeutics – Grant/Research Support. Novartis – Grant/Research Support. Novo Nordisk Inc – Consultant, Grant/Research Support. Organovo – Consultant, Grant/Research Support. Poxel Co – Grant/Research Support. Regeneron – Consultant, Grant/Research Support. Sagimet Biosciences – Consultant, Grant/Research Support. Takeda – Grant/Research Support. Terns pharmaceuticals – Grant/Research Support. Viking Therapeutics – Grant/Research Support. Zydus Pharmaceuticals – Grant/Research Support.
Jan Petrasek indicated no relevant financial relationships.
Andres Gomez-Aldana indicated no relevant financial relationships.
Olga Karina K. Morales, MD1, Ussama Ghumman, MD2, Lisa D. Pedicone, PhD3, Eugenia K. Tsai, MD2, Fred Poordad, MD2, Fabian Rodas, MD2, Eric Lawitz, MD4, Jan Petrasek, MD2, Andres Gomez-Aldana, MD3. P6050 - Multilobulated Bilomas as a Late Complication of Remote Cholecystectomy: A Diagnostic Challenge in a Patient With Chronic Abdominal Pain, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Texas Institute for Graduate Medical Education and Research, San Antonio, TX; 2University of Texas Health San Antonio, San Antonio, TX; 3Texas Liver Institute, Austin, TX; 4Texas Liver Institute, San Antonio, TX
Introduction: Bilomas are localized collections of bile outside the biliary system, resulting from iatrogenic or traumatic bile duct injury. They typically present within days to two weeks following hepatobiliary procedures. Delayed manifestations are rare and underreported. Incidence of delayed bilomas is < 0.1%, with extremely few cases occurring decades after cholecystectomy.
Case Description/
Methods: A 49 yo female with a history of hypertension, hypothyroidism, gastroparesis and peptic ulcer disease, presented with bilateral upper quadrant abdominal pain over several months. She had a remote cholecystectomy >20 years ago. Abdominal pain was associated with nausea but no vomiting, diarrhea, jaundice or food related symptoms. Labs showed WBC 17.05, elevated AST/ALT 58/62, elevated ALP 306 and lipase 43. Contrast CT revealed new, poorly defined hypodense lesions in the right hepatic lobe, measuring 8.9 cm in segments V and VIII concerning for malignancy (Figure 1). MRCP showed T2 hyperintense, lobulated lesions, measuring 14.6 cm (Figure 2). Findings raised concern for lobulated, hepatic cystic lesions with bilomas considered in the differential diagnosis. IR aspirated 15 mL of green bile and cytology showed degenerative debris without malignancy. A biliary drain catheter was placed yielding an initial 250 mL of bile. The catheter remained in place continuously draining for 3 month and posteriorly self-resolved with residual hepatic necrotic tissue.
Discussion: Delayed presentation of bilomas occurring decades after cholecystectomy is exceptionally rare and not initially considered in the differential diagnosis of hepatic cystic lesions. The remote history of cholecystectomy >20 years ago, contributed to the delayed recognition of biloma as a possible etiology. In this case the underlying mechanism for delayed formation remains speculative. Proposed theories include micro rupture of an accessory bile duct or pressure related biliary compromise from conditions such as gastroparesis or peptic ulcer disease. MRCP findings, IR aspiration of bile and exclusion of malignancy, confirmed the diagnosis. While small, asymptomatic bilomas may resolve spontaneously, larger or symptomatic collections typically require IR percutaneous drainage. In refractory cases or those with persistent bile leaks, ERCP with stenting may be indicated. In this case, percutaneous drainage led to symptom resolution and provided definitive diagnosis.

Figure: Figure 1,T2 weighted MRCP sequence showing multilobulated hyperintense fluid collection within hepatic segment V and VIII consistent with biloma.
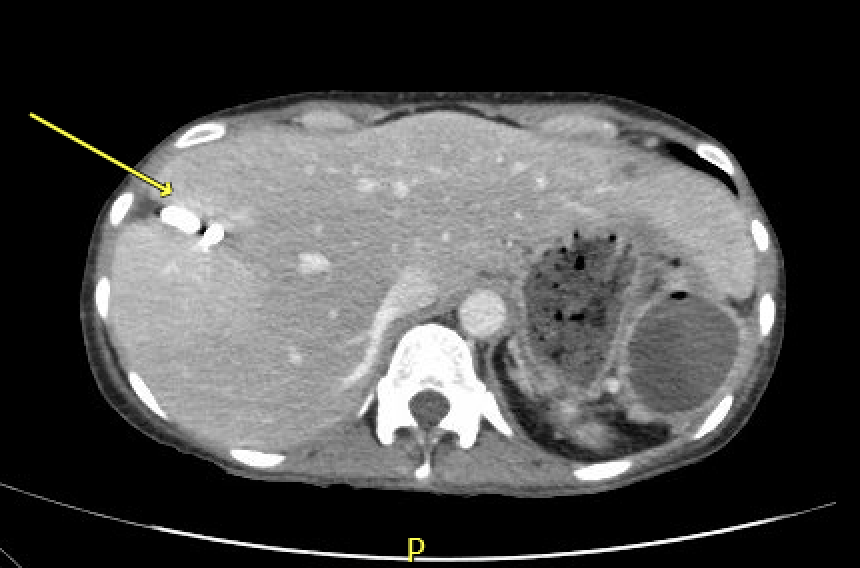
Figure: Figure 2, Abdomen CT w/wo contrast, yellow arrow showing drain in the right hepatic lobe with resolution of the previously visualized biloma.
Disclosures:
Olga Karina Morales indicated no relevant financial relationships.
Ussama Ghumman indicated no relevant financial relationships.
Lisa D. Pedicone indicated no relevant financial relationships.
Eugenia Tsai indicated no relevant financial relationships.
Fred Poordad indicated no relevant financial relationships.
Fabian Rodas indicated no relevant financial relationships.
Eric Lawitz: 89 Bio INC – Consultant, Grant/Research Support, Speakers Bureau. Abbvie – Speakers Bureau. Akero Therapeitics – Grant/Research Support. Alnylam Phamaceuticals INC – Grant/Research Support. Amgen – Grant/Research Support. Aztrazeneca – Consultant, Grant/Research Support. Bioscience – Grant/Research Support. Boehringer Ingelheim – Consultant, Grant/Research Support. Bristol-Myers Squibb – Grant/Research Support. Corcept Therapeutics – Consultant, Grant/Research Support. Cour Pharmaceuticals Inc – Grant/Research Support. Cymabay Therapeutics – Grant/Research Support. Eli Lily and Company – Consultant, Grant/Research Support. Enanta Pharmaceuticals – Grant/Research Support. Enyo Pharma – Grant/Research Support. Exalenz – Grant/Research Support. Galectin Therapeutics – Grant/Research Support. Galmed Pharmaceuticals – Grant/Research Support. Genfit – Grant/Research Support. Gilead Sciences – Grant/Research Support, Speakers Bureau. GlaxoSmithKline – Grant/Research Support. Hanmi Pharmaceuticals – Grant/Research Support. Hightide Biopharma – Grant/Research Support. Intercept Pharmaceuticals – Grant/Research Support, Speakers Bureau. Inventiva – Grant/Research Support. Ipsen – Grant/Research Support. Jansen Pharmaceuticals – Grant/Research Support. Madrigal Pharmaceuticals – Grant/Research Support, Speakers Bureau. Merck & Co – Consultant, Grant/Research Support. NGM Biopharmaceuticals Inc – Grant/Research Support. Northsea Therapeutics – Grant/Research Support. Novartis – Grant/Research Support. Novo Nordisk Inc – Consultant, Grant/Research Support. Organovo – Consultant, Grant/Research Support. Poxel Co – Grant/Research Support. Regeneron – Consultant, Grant/Research Support. Sagimet Biosciences – Consultant, Grant/Research Support. Takeda – Grant/Research Support. Terns pharmaceuticals – Grant/Research Support. Viking Therapeutics – Grant/Research Support. Zydus Pharmaceuticals – Grant/Research Support.
Jan Petrasek indicated no relevant financial relationships.
Andres Gomez-Aldana indicated no relevant financial relationships.
Olga Karina K. Morales, MD1, Ussama Ghumman, MD2, Lisa D. Pedicone, PhD3, Eugenia K. Tsai, MD2, Fred Poordad, MD2, Fabian Rodas, MD2, Eric Lawitz, MD4, Jan Petrasek, MD2, Andres Gomez-Aldana, MD3. P6050 - Multilobulated Bilomas as a Late Complication of Remote Cholecystectomy: A Diagnostic Challenge in a Patient With Chronic Abdominal Pain, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
