Tuesday Poster Session
Category: Liver
P6049 - An Unusual Case of Autoimmune Hepatitis (AIH)/Primary Sclerosing Cholangitis (PSC) Overlap Syndrome Associated With Minimal Change Disease and Tubulointerstitial Nephritis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Michael Metry, MD
University Hospitals Cleveland Medical Center, Case Western Reserve University
Dayton, OH
Presenting Author(s)
Michael Metry, MD1, Syed Ali, MD2
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Dayton, OH; 2Dayton Gastroenterology, Dayton, OH
Introduction: Renal involvement is uncommon in AIH but, AIH with membranous nephropathy and IgA nephropathy have been reported. AIH/PSC overlap is a rare and incompletely defined entity. Tubulointerstitial nephritis (TIN) is typically drug-induced but can also result from autoimmune processes, such as IgG4-related disease. We present a case of AIH/PSC overlap associated with minimal change disease and TIN, in the absence of IgG4 or other systemic disease.
Case Description/
Methods: A 44-year-old African American woman with a remote history of hepatitis A, presented with persistently elevated liver enzymes and right upper quadrant pain. She was a nonsmoker with minimal alcohol use and a normal physical exam. Labs showed a cholestatic pattern (ALP 440, ALT 80); hepatitis B and C were negative. The only positive immunologic marker was smooth muscle antibody. Imaging showed nodular liver contour and irregular intrahepatic ducts, consistent with PSC. Liver biopsy revealed scattered neutrophils and plasma cells without iron or steatosis, supporting AIH/PSC overlap. She was treated with steroids and azathioprine, though liver enzymes remained elevated.
A year later, she developed lower extremity edema. Labs revealed hypoalbuminemia, nephrotic-range proteinuria, and rising creatinine. Further testing showed elevated p-ANCA, with negative LKM antibodies, SPEP, and IgG4. Renal biopsy revealed lymphoplasmacytic TIN without eosinophils. Electron microscopy revealed diffuse podocytopathy consistent with minimal change disease. Given the lack of eosinophilia or prior drug exposure, azathioprine-induced TIN was deemed unlikely. She improved with high-dose steroids and her renal function remained normal after taper.
Discussion: AIH/PSC overlap is rare and it’s association with renal disease is exceptionally uncommon. Dysregulated adaptive immunity targeting both liver and renal tissue is the most coherent explanation. Given the absence of systemic autoimmune conditions such as SLE or IgG4 related disease, or a drug reaction or malignancy, a possible new extrahepatic manifestation is suggested. A reaction to azathioprine was considered but, without eosinophilia on biopsy and an excellent response to steroids, despite continuation of azathioprine, this was excluded. Extra hepatic manifestations of autoimmune liver diseases should always be kept in mind when managing patients with AIH/PSC. Renal function must be closely monitored. Our patient with minimal change disease/TIN in this setting suggests a potential new association.
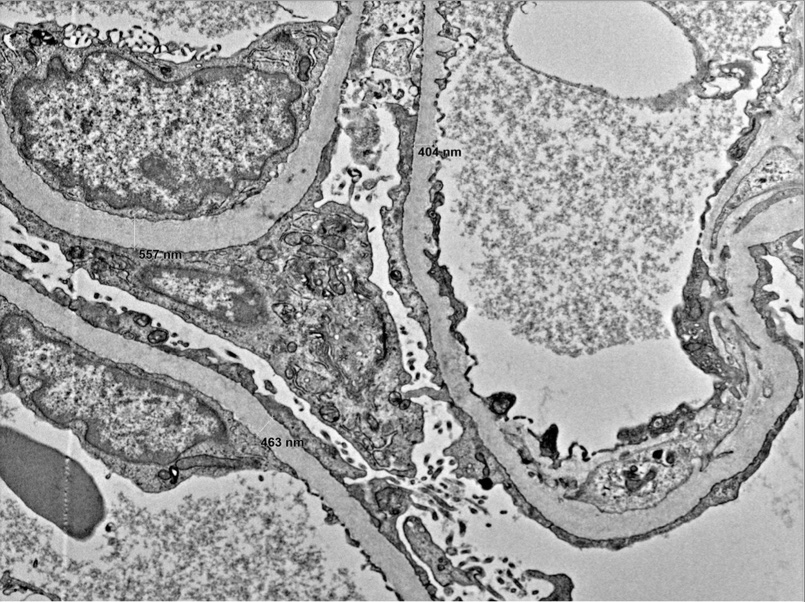
Figure: Electron micrograph of our patients renal biopsy showing diffuse podocytopathy, suggesting minimal change disease.
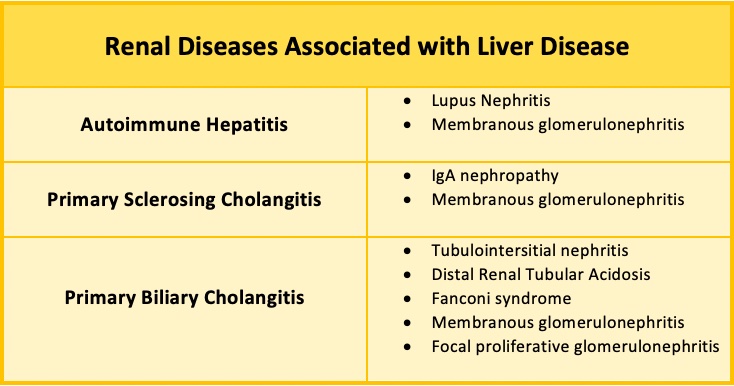
Figure: Table 1. summarizes some of the known renal associations of immune mediated liver disease.
Disclosures:
Michael Metry indicated no relevant financial relationships.
Syed Ali indicated no relevant financial relationships.
Michael Metry, MD1, Syed Ali, MD2. P6049 - An Unusual Case of Autoimmune Hepatitis (AIH)/Primary Sclerosing Cholangitis (PSC) Overlap Syndrome Associated With Minimal Change Disease and Tubulointerstitial Nephritis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Dayton, OH; 2Dayton Gastroenterology, Dayton, OH
Introduction: Renal involvement is uncommon in AIH but, AIH with membranous nephropathy and IgA nephropathy have been reported. AIH/PSC overlap is a rare and incompletely defined entity. Tubulointerstitial nephritis (TIN) is typically drug-induced but can also result from autoimmune processes, such as IgG4-related disease. We present a case of AIH/PSC overlap associated with minimal change disease and TIN, in the absence of IgG4 or other systemic disease.
Case Description/
Methods: A 44-year-old African American woman with a remote history of hepatitis A, presented with persistently elevated liver enzymes and right upper quadrant pain. She was a nonsmoker with minimal alcohol use and a normal physical exam. Labs showed a cholestatic pattern (ALP 440, ALT 80); hepatitis B and C were negative. The only positive immunologic marker was smooth muscle antibody. Imaging showed nodular liver contour and irregular intrahepatic ducts, consistent with PSC. Liver biopsy revealed scattered neutrophils and plasma cells without iron or steatosis, supporting AIH/PSC overlap. She was treated with steroids and azathioprine, though liver enzymes remained elevated.
A year later, she developed lower extremity edema. Labs revealed hypoalbuminemia, nephrotic-range proteinuria, and rising creatinine. Further testing showed elevated p-ANCA, with negative LKM antibodies, SPEP, and IgG4. Renal biopsy revealed lymphoplasmacytic TIN without eosinophils. Electron microscopy revealed diffuse podocytopathy consistent with minimal change disease. Given the lack of eosinophilia or prior drug exposure, azathioprine-induced TIN was deemed unlikely. She improved with high-dose steroids and her renal function remained normal after taper.
Discussion: AIH/PSC overlap is rare and it’s association with renal disease is exceptionally uncommon. Dysregulated adaptive immunity targeting both liver and renal tissue is the most coherent explanation. Given the absence of systemic autoimmune conditions such as SLE or IgG4 related disease, or a drug reaction or malignancy, a possible new extrahepatic manifestation is suggested. A reaction to azathioprine was considered but, without eosinophilia on biopsy and an excellent response to steroids, despite continuation of azathioprine, this was excluded. Extra hepatic manifestations of autoimmune liver diseases should always be kept in mind when managing patients with AIH/PSC. Renal function must be closely monitored. Our patient with minimal change disease/TIN in this setting suggests a potential new association.
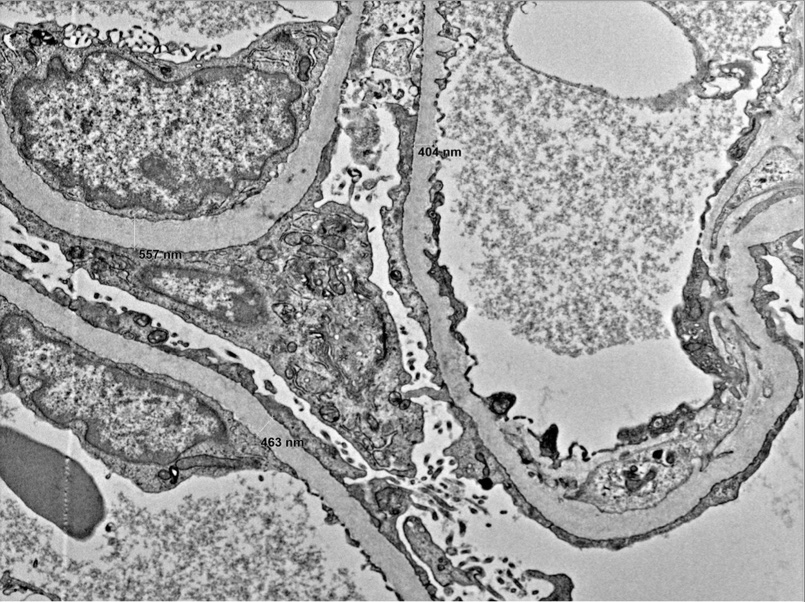
Figure: Electron micrograph of our patients renal biopsy showing diffuse podocytopathy, suggesting minimal change disease.
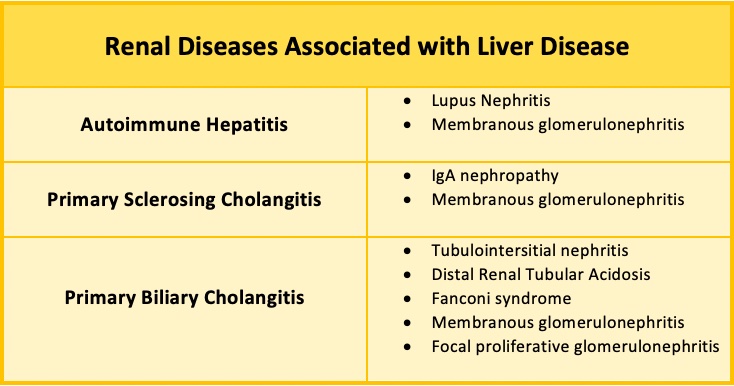
Figure: Table 1. summarizes some of the known renal associations of immune mediated liver disease.
Disclosures:
Michael Metry indicated no relevant financial relationships.
Syed Ali indicated no relevant financial relationships.
Michael Metry, MD1, Syed Ali, MD2. P6049 - An Unusual Case of Autoimmune Hepatitis (AIH)/Primary Sclerosing Cholangitis (PSC) Overlap Syndrome Associated With Minimal Change Disease and Tubulointerstitial Nephritis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
