Tuesday Poster Session
Category: Liver
P6153 - When the Gradient Fails: Unexplained Recurrent Low SAAG Ascites
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Kaushik Puranam, MD
Duke University School of Medicine
Durham, NC
Presenting Author(s)
Kaushik Puranam, MD1, Darshan Kothari, MD2, Michael Dore, MD1
1Duke University School of Medicine, Durham, NC; 2Duke University Health System, Durham, NC
Introduction: In the US, ascites is most commonly due to cirrhosis, but carries a broad differential including heart failure, infection, nephrotic syndrome, and cancer. The serum-to-ascites albumin gradient (SAAG) is a key diagnostic tool to help evaluate the etiology of ascites; a high gradient (≥ 1.1 g/dL) signifies portal hypertension, whereas a low gradient (< 1.1 g/dL) suggests conditions such as peritoneal malignancy or tuberculosis, pancreatitis, serositis or nephrotic syndrome. We present a case of recurrent low SAAG ascites.
Case Description/
Methods: A 79-year male with history significant for HFpEF, CAD, CKD, atrial fibrillation, prior tobacco use, and COPD presented with two months of progressive abdominal distention. Recent ultrasound demonstrated a nodular liver, concerning for cirrhosis. On exam he had abdominal distention with tenderness, bilateral lower extremity edema and no jaundice.
Initial paracentesis revealed hazy orange fluid with a low SAAG and high protein; his course was complicated by a NSTEMI needing cardiac catheterization and stent placement. Despite normal ejection fraction, he continued to accumulate fluid, requiring paracentesis every 5 days. Fluid and serum analysis remained consistent: low SAAG/high protein, negative cytology, and cultures (Table 1). Extensive serologic and ascitic fluid testing, including Hepatitis A, B, C, AFP, ANA, AMA, ASMA, CEA, CA 19-9, A1AT (serum and stool), amylase, urine protein to creatinine ratio, ascitic creatinine, and BNP, was unrevealing. Adenosine deaminase level was mildly elevated, however, QuantiFERON Gold and AFB cultures were negative. MRI of the abdomen showed normal hepatic morphology, and normal hepatic vein portal gradient. The patient subsequently underwent PET/CT and peritoneal biopsy, which were negative for occult malignancy. With no clear etiology found, the patient was discharged with a plan for weekly paracentesis.
Discussion: This case highlights the diagnostic challenges posed by recurrent low SAAG ascites when common etiologies are excluded. Despite exhaustive testing and the involvement of multiple specialties, no definitive diagnosis was found. Such cases underscore the importance of thorough workups while balancing the need to establish a safe outpatient plan.
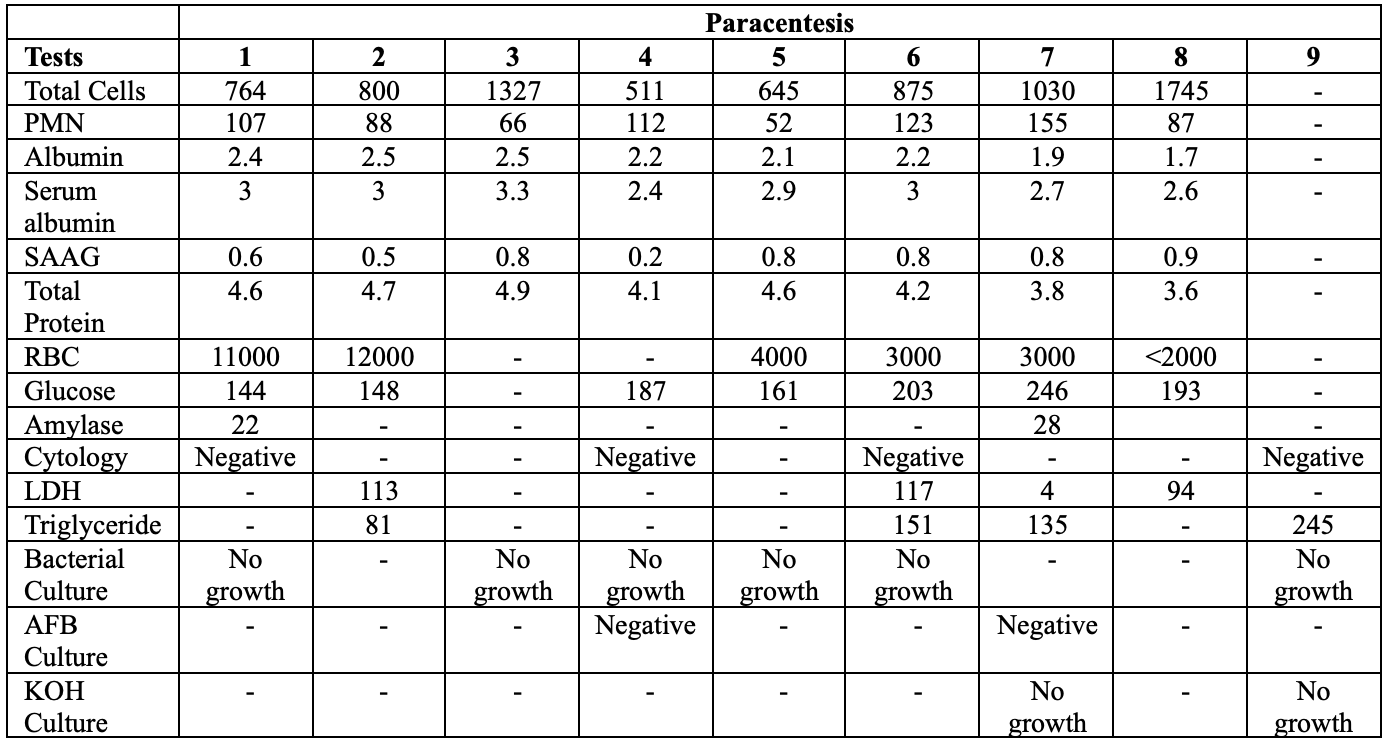
Figure: Table 1. Timeline of Ascitic Fluid Evaluation and Key Results
Disclosures:
Kaushik Puranam indicated no relevant financial relationships.
Darshan Kothari indicated no relevant financial relationships.
Michael Dore indicated no relevant financial relationships.
Kaushik Puranam, MD1, Darshan Kothari, MD2, Michael Dore, MD1. P6153 - When the Gradient Fails: Unexplained Recurrent Low SAAG Ascites, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Duke University School of Medicine, Durham, NC; 2Duke University Health System, Durham, NC
Introduction: In the US, ascites is most commonly due to cirrhosis, but carries a broad differential including heart failure, infection, nephrotic syndrome, and cancer. The serum-to-ascites albumin gradient (SAAG) is a key diagnostic tool to help evaluate the etiology of ascites; a high gradient (≥ 1.1 g/dL) signifies portal hypertension, whereas a low gradient (< 1.1 g/dL) suggests conditions such as peritoneal malignancy or tuberculosis, pancreatitis, serositis or nephrotic syndrome. We present a case of recurrent low SAAG ascites.
Case Description/
Methods: A 79-year male with history significant for HFpEF, CAD, CKD, atrial fibrillation, prior tobacco use, and COPD presented with two months of progressive abdominal distention. Recent ultrasound demonstrated a nodular liver, concerning for cirrhosis. On exam he had abdominal distention with tenderness, bilateral lower extremity edema and no jaundice.
Initial paracentesis revealed hazy orange fluid with a low SAAG and high protein; his course was complicated by a NSTEMI needing cardiac catheterization and stent placement. Despite normal ejection fraction, he continued to accumulate fluid, requiring paracentesis every 5 days. Fluid and serum analysis remained consistent: low SAAG/high protein, negative cytology, and cultures (Table 1). Extensive serologic and ascitic fluid testing, including Hepatitis A, B, C, AFP, ANA, AMA, ASMA, CEA, CA 19-9, A1AT (serum and stool), amylase, urine protein to creatinine ratio, ascitic creatinine, and BNP, was unrevealing. Adenosine deaminase level was mildly elevated, however, QuantiFERON Gold and AFB cultures were negative. MRI of the abdomen showed normal hepatic morphology, and normal hepatic vein portal gradient. The patient subsequently underwent PET/CT and peritoneal biopsy, which were negative for occult malignancy. With no clear etiology found, the patient was discharged with a plan for weekly paracentesis.
Discussion: This case highlights the diagnostic challenges posed by recurrent low SAAG ascites when common etiologies are excluded. Despite exhaustive testing and the involvement of multiple specialties, no definitive diagnosis was found. Such cases underscore the importance of thorough workups while balancing the need to establish a safe outpatient plan.
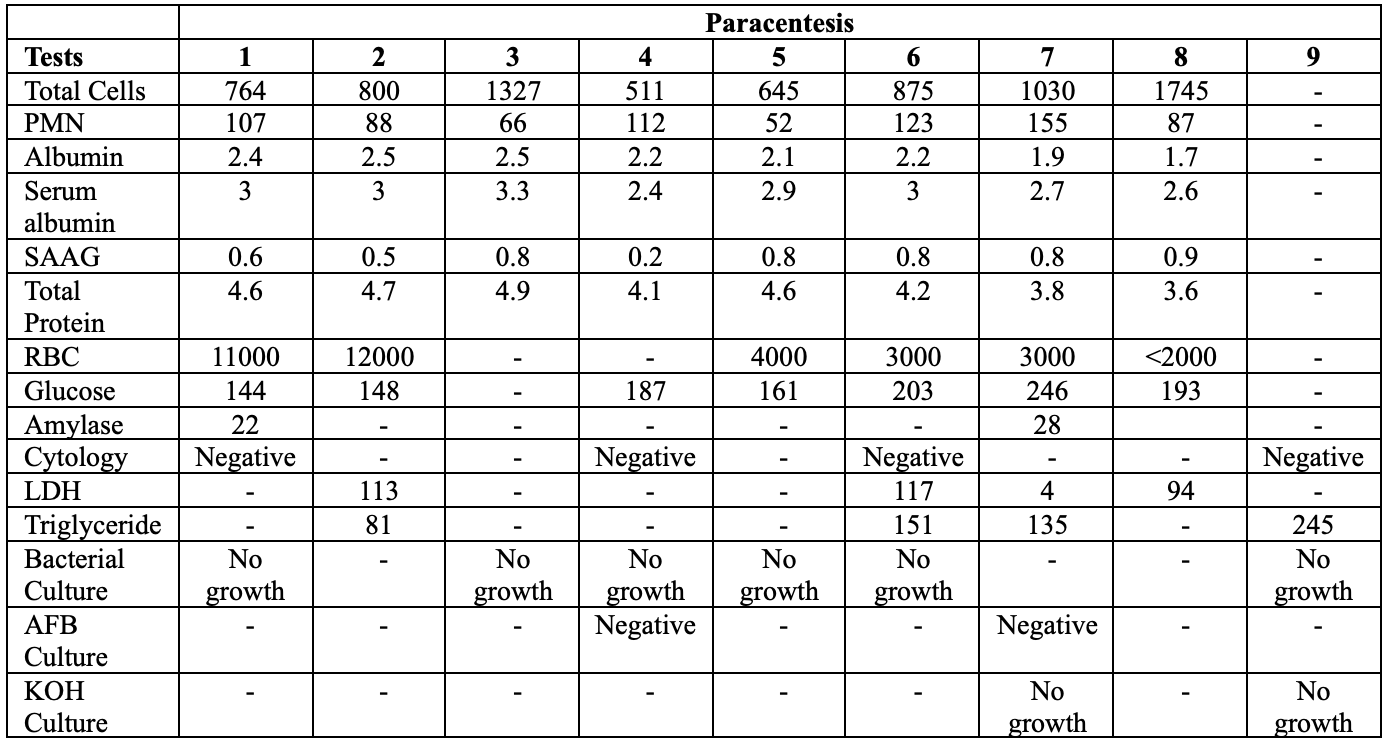
Figure: Table 1. Timeline of Ascitic Fluid Evaluation and Key Results
Disclosures:
Kaushik Puranam indicated no relevant financial relationships.
Darshan Kothari indicated no relevant financial relationships.
Michael Dore indicated no relevant financial relationships.
Kaushik Puranam, MD1, Darshan Kothari, MD2, Michael Dore, MD1. P6153 - When the Gradient Fails: Unexplained Recurrent Low SAAG Ascites, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
