Tuesday Poster Session
Category: Liver
P6152 - Primary Hepatic Squamous Cell Carcinoma: Diagnostic Dilemmas and Therapeutic Strategies in a Rare Liver Malignancy
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mhd Kutaiba Albuni, MD (he/him/his)
Department of Internal Medicine, TriHealth Inc., Cincinnati
Cincinnati, OH
Presenting Author(s)
Mhd Kutaiba Albuni, MD1, Bisher Sawaf, MD2, Yusuf Omar Hallak, MD3, Muhamad Hijazi, MD4, Halime Kartal, MD5, Ankitha Vanaparti, MD4, Fayaz Khan, MD4, Shahem Abbarh, MD6, Amine Rakab, MD7
1Department of Internal Medicine, TriHealth Inc., Cincinnati, Cincinnati, OH; 2University of Toledo Medical Center, Toledo, OH; 3The University of Toledo, Toledo, OH; 4TriHealth, Cincinnati, OH; 5International School of medicine, Istanbul Medipol University, Istanbul, Istanbul, Turkey; 6Georgetown University MedStar Health, Baltimore, WA; 7Division of Medical Education, Weill Cornell Medicine, Doha, Ad Dawhah, Qatar
Introduction: Primary squamous cell carcinoma (SCC) of the liver is extremely rare, with few cases reported. It is often associated with hepatic cysts or hepatolithiasis, and unlike hepatocellular carcinoma, lacks specific markers or imaging features. Diagnosis requires histopathology and exclusion of metastasis. No standardized treatment exists; options include surgery, chemotherapy, and immunotherapy, but prognosis is poor. This study presents a case of Liver primary SCC in a 64-year-old woman, including imaging and genetic findings.
Case Description/
Methods: A 64-year-old woman with CAD s/p CABG, CKD, and tobacco use presented with RUQ pain, fever, and 50-pound weight loss. CT imaging revealed a large hepatic lesion and a smaller satellite lesion. Labs showed leukocytosis but normal liver enzymes and tumor markers (AFP, CEA). A liver biopsy confirmed squamous cell carcinoma (SCC). Immunohistochemistry ruled out metastases from other primaries. PET scan showed an 8 cm liver mass; endoscopies were negative. Genomic testing showed PD-L1 positivity without targetable mutations. Given poor functional status, she was not a candidate for chemotherapy. Palliative immunotherapy was initiated, but she eventually succumbed to the disease within four months of presentation.
Discussion: Primary hepatic squamous cell carcinoma (SCC) is an exceptionally rare malignancy with unclear pathogenesis. Proposed mechanisms include chronic bile duct inflammation, hepatic cysts, and squamous metaplasia secondary to prolonged irritation. Most patients, like ours, lack typical risk factors such as viral hepatitis or cirrhosis. Symptoms are nonspecific—commonly RUQ pain, jaundice, and weight loss—often mimicking liver abscess, as in our case. Tumor markers such as AFP, CEA, and CA 19-9 are typically normal, and liver enzymes may also be within the normal range. Diagnosis relies on histopathology and immunohistochemistry, with positive staining for p40, p63, and CKs, and exclusion of other primary SCC sites through imaging and endoscopy. CT imaging usually shows a heterogeneous liver mass without characteristic features. PD-L1 expression may guide immunotherapy, as reported in some cases. However, in our case there were no targetable mutations. Because diagnosis is one of exclusion and no standard treatment exists, a multidisciplinary approach is essential. Prognosis remains poor, with limited survival even with intervention.
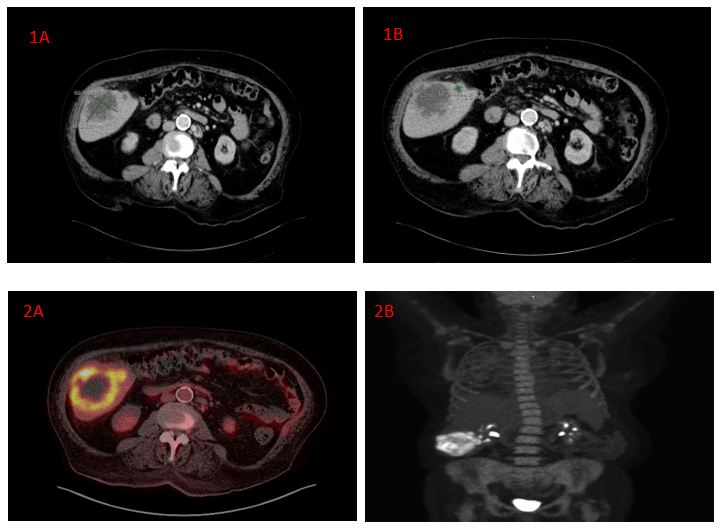
Figure: Figure 1a: A contrast-enhanced computed tomography (CT) scan of the abdomen revealed a dominant lesion in the right hepatic lobe measuring approximately 6.6 cm.
Figure1b: A contrast-enhanced computed tomography (CT) scan of the abdomen revealed a dominant lesion in the right hepatic lobe with a smaller adjacent satellite lesion measuring 1.4 cm.
Figure 2a: Positron emission tomography (PET) imaging demonstrated an 8 cm hepatic lesion with intense peripheral fluorodeoxyglucose (FDG) uptake and heterogeneous intralesional activity.
Figure 2b: Positron emission tomography (PET) imaging demonstrated new bilateral pulmonary infiltrates consistent with an inflammatory process were also observed.
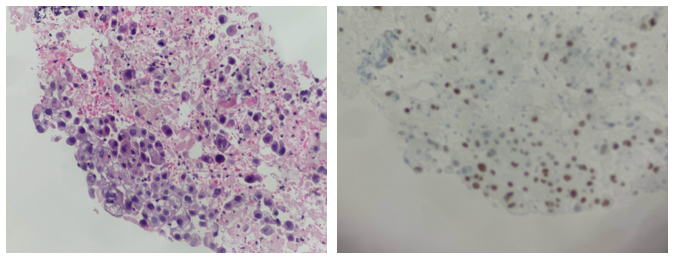
Figure: Histopathological analysis of the liver tissue revealed squamous cell carcinoma. Immunohistochemical staining was positive for pan-keratin, CAM 5.2, p40, and p63, confirming squamous differentiation. Markers for hepatocellular origin (hepatocyte-specific antigen [HSA], glypican-3), breast and urothelial carcinoma (GATA3), colorectal and intestinal tumors (SATB2, CDX2), pulmonary adenocarcinoma (TTF-1), PAX8, estrogen receptors, and melanoma (SOX10) were all negative. Immunoperoxidase staining for p53 showed only rare positive nuclei.
Disclosures:
Mhd Kutaiba Albuni indicated no relevant financial relationships.
Bisher Sawaf indicated no relevant financial relationships.
Yusuf Omar Hallak indicated no relevant financial relationships.
Muhamad Hijazi indicated no relevant financial relationships.
Halime Kartal indicated no relevant financial relationships.
Ankitha Vanaparti indicated no relevant financial relationships.
Fayaz Khan indicated no relevant financial relationships.
Shahem Abbarh indicated no relevant financial relationships.
Amine Rakab indicated no relevant financial relationships.
Mhd Kutaiba Albuni, MD1, Bisher Sawaf, MD2, Yusuf Omar Hallak, MD3, Muhamad Hijazi, MD4, Halime Kartal, MD5, Ankitha Vanaparti, MD4, Fayaz Khan, MD4, Shahem Abbarh, MD6, Amine Rakab, MD7. P6152 - Primary Hepatic Squamous Cell Carcinoma: Diagnostic Dilemmas and Therapeutic Strategies in a Rare Liver Malignancy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Department of Internal Medicine, TriHealth Inc., Cincinnati, Cincinnati, OH; 2University of Toledo Medical Center, Toledo, OH; 3The University of Toledo, Toledo, OH; 4TriHealth, Cincinnati, OH; 5International School of medicine, Istanbul Medipol University, Istanbul, Istanbul, Turkey; 6Georgetown University MedStar Health, Baltimore, WA; 7Division of Medical Education, Weill Cornell Medicine, Doha, Ad Dawhah, Qatar
Introduction: Primary squamous cell carcinoma (SCC) of the liver is extremely rare, with few cases reported. It is often associated with hepatic cysts or hepatolithiasis, and unlike hepatocellular carcinoma, lacks specific markers or imaging features. Diagnosis requires histopathology and exclusion of metastasis. No standardized treatment exists; options include surgery, chemotherapy, and immunotherapy, but prognosis is poor. This study presents a case of Liver primary SCC in a 64-year-old woman, including imaging and genetic findings.
Case Description/
Methods: A 64-year-old woman with CAD s/p CABG, CKD, and tobacco use presented with RUQ pain, fever, and 50-pound weight loss. CT imaging revealed a large hepatic lesion and a smaller satellite lesion. Labs showed leukocytosis but normal liver enzymes and tumor markers (AFP, CEA). A liver biopsy confirmed squamous cell carcinoma (SCC). Immunohistochemistry ruled out metastases from other primaries. PET scan showed an 8 cm liver mass; endoscopies were negative. Genomic testing showed PD-L1 positivity without targetable mutations. Given poor functional status, she was not a candidate for chemotherapy. Palliative immunotherapy was initiated, but she eventually succumbed to the disease within four months of presentation.
Discussion: Primary hepatic squamous cell carcinoma (SCC) is an exceptionally rare malignancy with unclear pathogenesis. Proposed mechanisms include chronic bile duct inflammation, hepatic cysts, and squamous metaplasia secondary to prolonged irritation. Most patients, like ours, lack typical risk factors such as viral hepatitis or cirrhosis. Symptoms are nonspecific—commonly RUQ pain, jaundice, and weight loss—often mimicking liver abscess, as in our case. Tumor markers such as AFP, CEA, and CA 19-9 are typically normal, and liver enzymes may also be within the normal range. Diagnosis relies on histopathology and immunohistochemistry, with positive staining for p40, p63, and CKs, and exclusion of other primary SCC sites through imaging and endoscopy. CT imaging usually shows a heterogeneous liver mass without characteristic features. PD-L1 expression may guide immunotherapy, as reported in some cases. However, in our case there were no targetable mutations. Because diagnosis is one of exclusion and no standard treatment exists, a multidisciplinary approach is essential. Prognosis remains poor, with limited survival even with intervention.
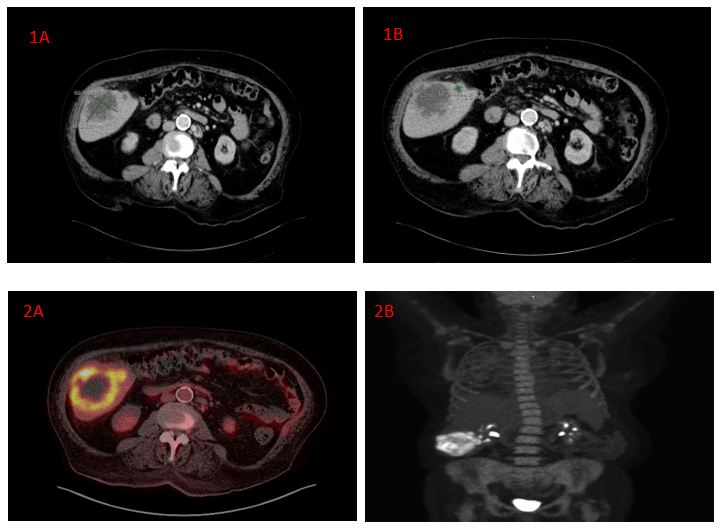
Figure: Figure 1a: A contrast-enhanced computed tomography (CT) scan of the abdomen revealed a dominant lesion in the right hepatic lobe measuring approximately 6.6 cm.
Figure1b: A contrast-enhanced computed tomography (CT) scan of the abdomen revealed a dominant lesion in the right hepatic lobe with a smaller adjacent satellite lesion measuring 1.4 cm.
Figure 2a: Positron emission tomography (PET) imaging demonstrated an 8 cm hepatic lesion with intense peripheral fluorodeoxyglucose (FDG) uptake and heterogeneous intralesional activity.
Figure 2b: Positron emission tomography (PET) imaging demonstrated new bilateral pulmonary infiltrates consistent with an inflammatory process were also observed.
Figure: Histopathological analysis of the liver tissue revealed squamous cell carcinoma. Immunohistochemical staining was positive for pan-keratin, CAM 5.2, p40, and p63, confirming squamous differentiation. Markers for hepatocellular origin (hepatocyte-specific antigen [HSA], glypican-3), breast and urothelial carcinoma (GATA3), colorectal and intestinal tumors (SATB2, CDX2), pulmonary adenocarcinoma (TTF-1), PAX8, estrogen receptors, and melanoma (SOX10) were all negative. Immunoperoxidase staining for p53 showed only rare positive nuclei.
Disclosures:
Mhd Kutaiba Albuni indicated no relevant financial relationships.
Bisher Sawaf indicated no relevant financial relationships.
Yusuf Omar Hallak indicated no relevant financial relationships.
Muhamad Hijazi indicated no relevant financial relationships.
Halime Kartal indicated no relevant financial relationships.
Ankitha Vanaparti indicated no relevant financial relationships.
Fayaz Khan indicated no relevant financial relationships.
Shahem Abbarh indicated no relevant financial relationships.
Amine Rakab indicated no relevant financial relationships.
Mhd Kutaiba Albuni, MD1, Bisher Sawaf, MD2, Yusuf Omar Hallak, MD3, Muhamad Hijazi, MD4, Halime Kartal, MD5, Ankitha Vanaparti, MD4, Fayaz Khan, MD4, Shahem Abbarh, MD6, Amine Rakab, MD7. P6152 - Primary Hepatic Squamous Cell Carcinoma: Diagnostic Dilemmas and Therapeutic Strategies in a Rare Liver Malignancy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
