Tuesday Poster Session
Category: Liver
P6149 - Two Sides of the Same Coin: Contrasting Presentations and Outcomes of Hepatitis E Virus Infection in a Transplant Recipient and an Immunocompetent Host
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mina Awadallah, MD, MSc
University of Utah
Salt Lake City, UT
Presenting Author(s)
Mina Awadallah, MD, MSc1, Avneet Singh, DO2, Gillian Hale, MD, MPH1, Mariana Moreno-Prats, MD1, John Erikson Yap, MD, MBA, FACG3, Juan F. Gallegos-Orozco, MD, FACG3
1University of Utah, Salt Lake City, UT; 2Cooper University Health Care, Camden, NJ; 3University of Utah Health, Salt Lake City, UT
Introduction: Hepatitis E virus (HEV) is a non-enveloped RNA virus known to cause self-limited hepatitis in immunocompetent individuals but may lead to chronic infection in immunocompromised hosts. In rare cases, HEV can cause acute liver failure (ALF). We present two contrasting cases that illustrate the clinical spectrum of HEV infection and underscore the importance of early recognition and tailored management.
Case Description/
Methods: Case 1 – Acute Liver Failure in an Immunocompetent Host:
A 67-year-old man with diabetes and coronary artery disease presented with jaundice and hepatic encephalopathy. Labs revealed AST 9,813 U/L, ALT 7,057 U/L, bilirubin 16.8 mg/dL, INR 3.5, and ammonia 109 µmol/L. HEV IgM, IgG, and RNA (4.56 million IU/mL) were positive. Liver biopsy showed severe hepatitis with bridging necrosis. Despite ICU-level care, he deteriorated rapidly and died five days later. Autopsy confirmed fulminant hepatic necrosis due to HEV.
Case 2 – Chronic HEV in a Liver Transplant Recipient:
A 47-year-old man with NASH cirrhosis underwent liver transplantation. Three months later, he developed elevated liver enzymes (AST 133 U/L, ALT 573 U/L). Biopsies showed mild hepatitis without rejection. HEV RNA was positive (5.5 million IU/mL). He was treated with ribavirin 400 mg BID and adjustments in immunosuppression. After 12 weeks, liver enzymes normalized, and HEV RNA became undetectable. He remained well 3 months post-treatment.
Discussion: These cases highlight the divergent outcomes of HEV based on host immune status. The immunocompetent patient developed fulminant hepatitis and died, despite having a similar viral load to the transplant recipient who recovered with antiviral therapy. In immunocompromised patients, HEV may present subtly but progress to chronicity. Early HEV testing should be considered in patients with unexplained hepatitis, particularly those with recent transplantation or systemic stress. Prompt diagnosis and appropriate therapy can significantly alter outcomes.
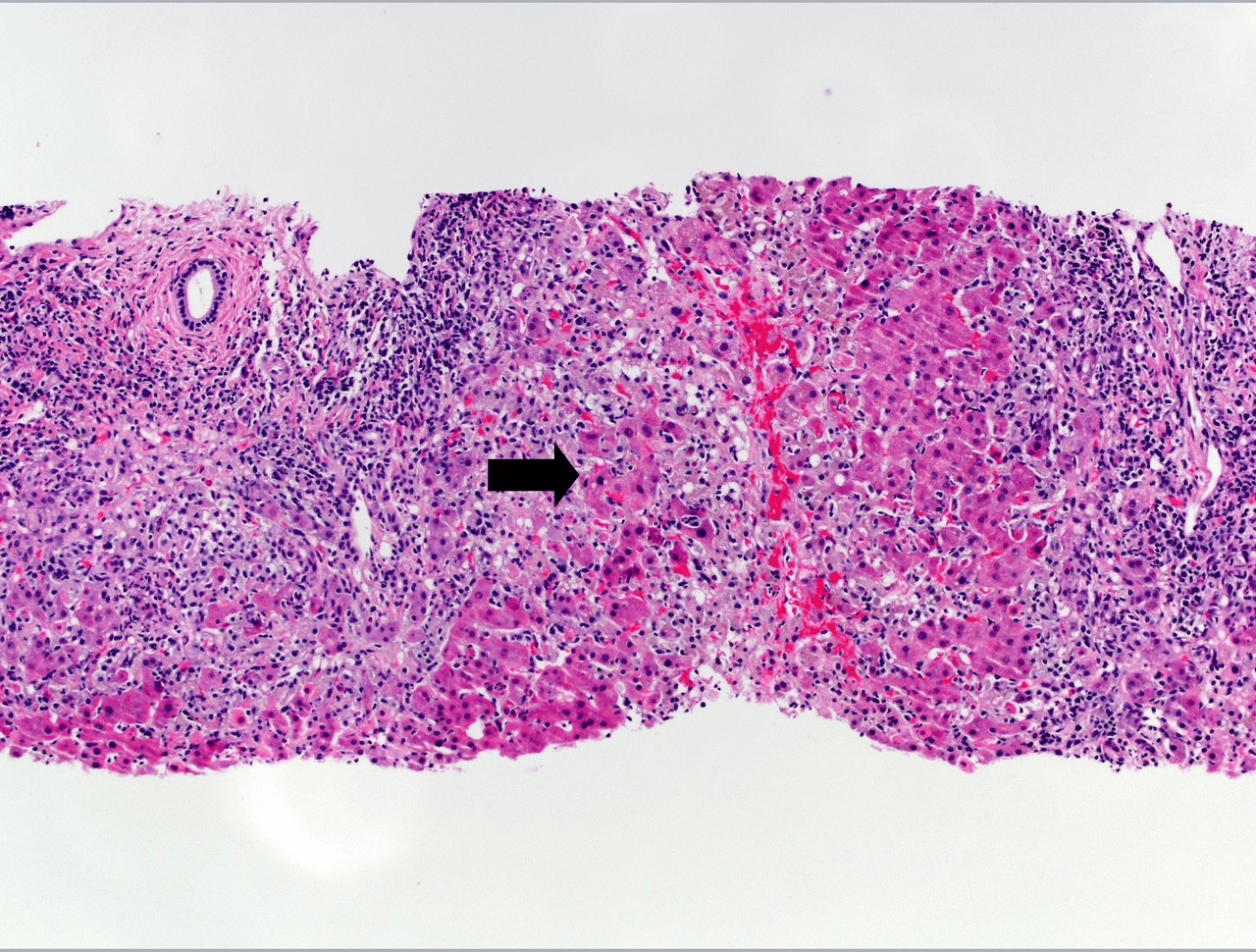
Figure: HEV in post transplant liver biopsy
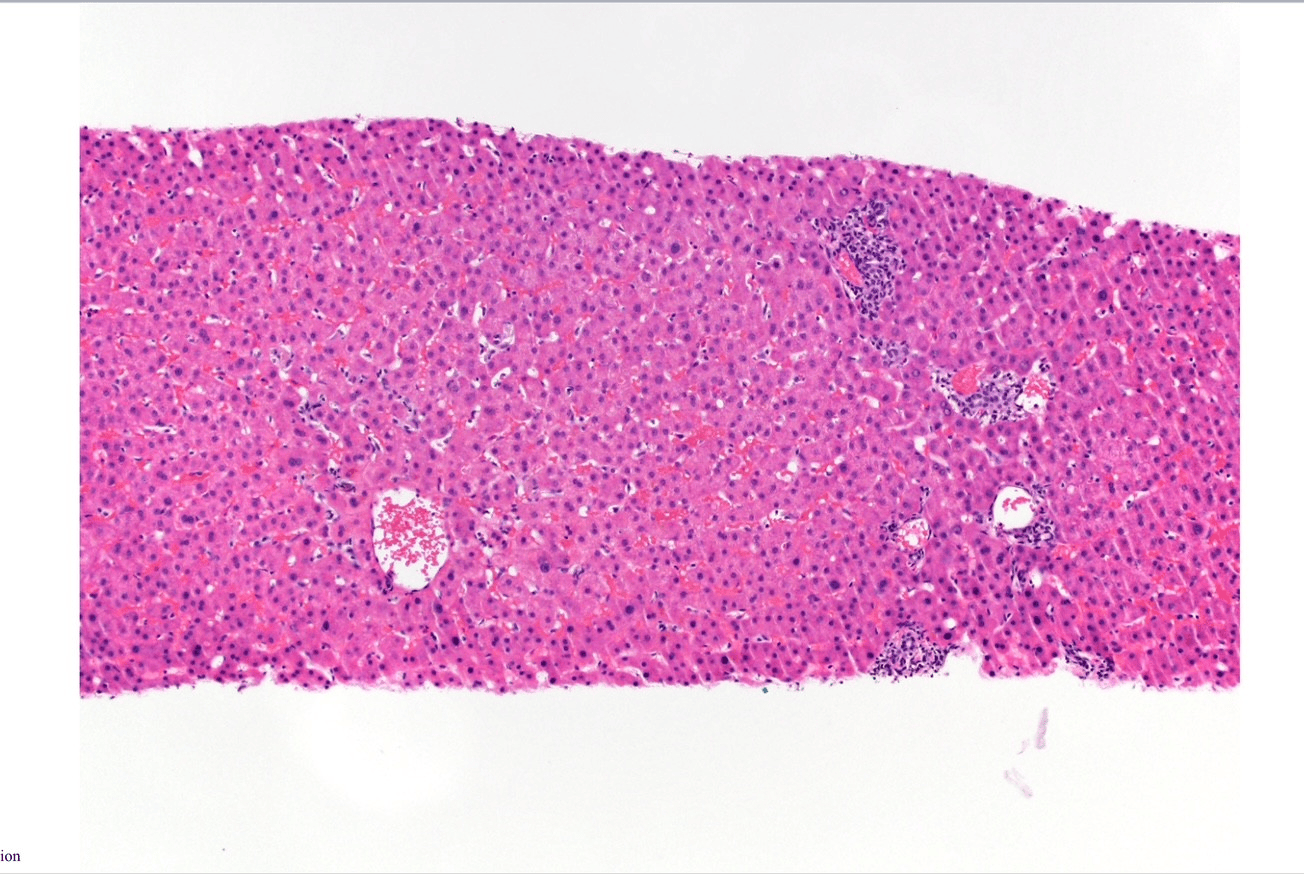
Figure: HEV in fulminant liver failure liver biopsy
Disclosures:
Mina Awadallah indicated no relevant financial relationships.
Avneet Singh indicated no relevant financial relationships.
Gillian Hale indicated no relevant financial relationships.
Mariana Moreno-Prats indicated no relevant financial relationships.
John Erikson Yap: Phathom Pharmaceutical – Speakers Bureau. Steris – Consultant.
Juan Gallegos-Orozco: Gilead – Grant/Research Support. Hanmi – Grant/Research Support. Intercept – Grant/Research Support. Mirum – Grant/Research Support.
Mina Awadallah, MD, MSc1, Avneet Singh, DO2, Gillian Hale, MD, MPH1, Mariana Moreno-Prats, MD1, John Erikson Yap, MD, MBA, FACG3, Juan F. Gallegos-Orozco, MD, FACG3. P6149 - Two Sides of the Same Coin: Contrasting Presentations and Outcomes of Hepatitis E Virus Infection in a Transplant Recipient and an Immunocompetent Host, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Utah, Salt Lake City, UT; 2Cooper University Health Care, Camden, NJ; 3University of Utah Health, Salt Lake City, UT
Introduction: Hepatitis E virus (HEV) is a non-enveloped RNA virus known to cause self-limited hepatitis in immunocompetent individuals but may lead to chronic infection in immunocompromised hosts. In rare cases, HEV can cause acute liver failure (ALF). We present two contrasting cases that illustrate the clinical spectrum of HEV infection and underscore the importance of early recognition and tailored management.
Case Description/
Methods: Case 1 – Acute Liver Failure in an Immunocompetent Host:
A 67-year-old man with diabetes and coronary artery disease presented with jaundice and hepatic encephalopathy. Labs revealed AST 9,813 U/L, ALT 7,057 U/L, bilirubin 16.8 mg/dL, INR 3.5, and ammonia 109 µmol/L. HEV IgM, IgG, and RNA (4.56 million IU/mL) were positive. Liver biopsy showed severe hepatitis with bridging necrosis. Despite ICU-level care, he deteriorated rapidly and died five days later. Autopsy confirmed fulminant hepatic necrosis due to HEV.
Case 2 – Chronic HEV in a Liver Transplant Recipient:
A 47-year-old man with NASH cirrhosis underwent liver transplantation. Three months later, he developed elevated liver enzymes (AST 133 U/L, ALT 573 U/L). Biopsies showed mild hepatitis without rejection. HEV RNA was positive (5.5 million IU/mL). He was treated with ribavirin 400 mg BID and adjustments in immunosuppression. After 12 weeks, liver enzymes normalized, and HEV RNA became undetectable. He remained well 3 months post-treatment.
Discussion: These cases highlight the divergent outcomes of HEV based on host immune status. The immunocompetent patient developed fulminant hepatitis and died, despite having a similar viral load to the transplant recipient who recovered with antiviral therapy. In immunocompromised patients, HEV may present subtly but progress to chronicity. Early HEV testing should be considered in patients with unexplained hepatitis, particularly those with recent transplantation or systemic stress. Prompt diagnosis and appropriate therapy can significantly alter outcomes.
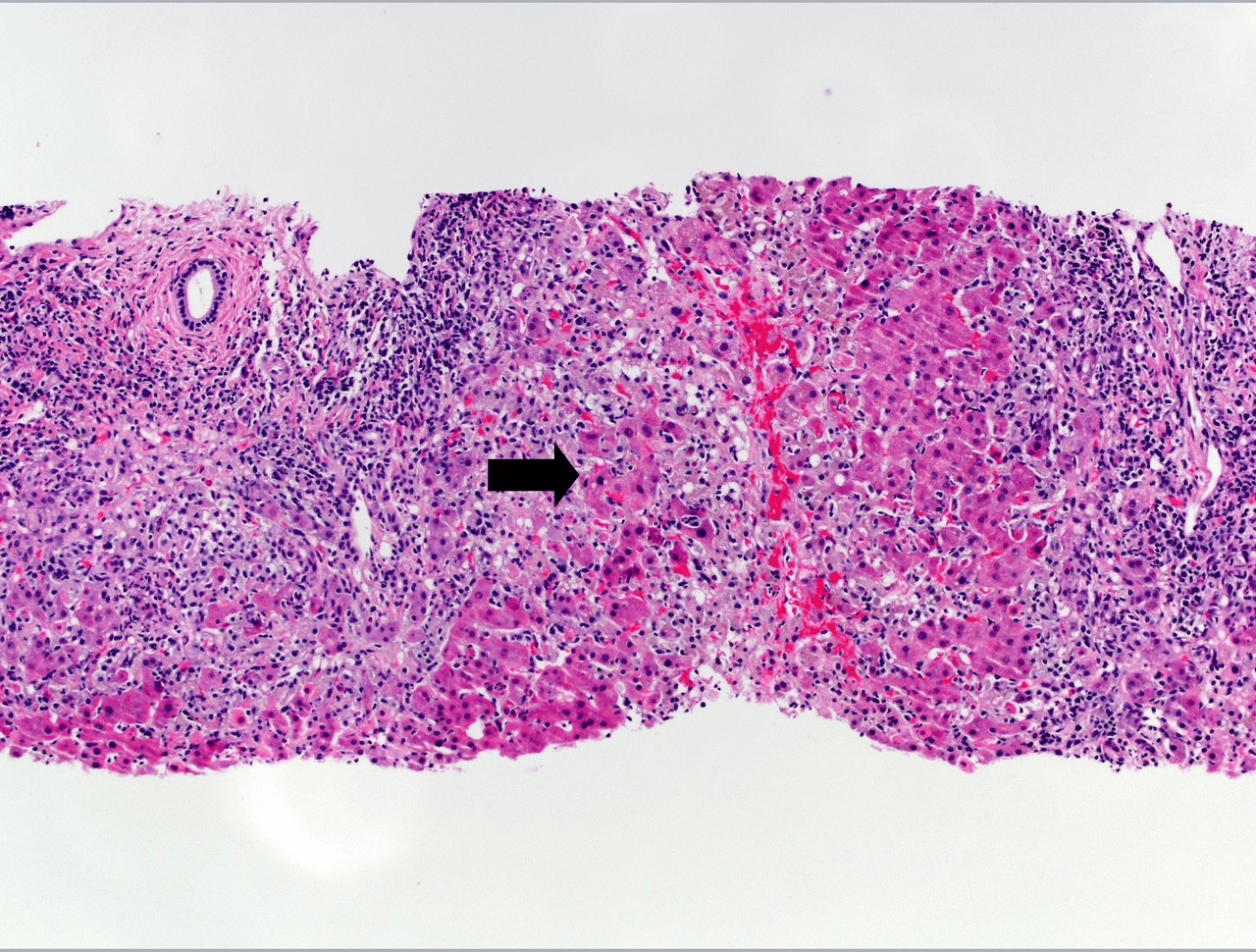
Figure: HEV in post transplant liver biopsy
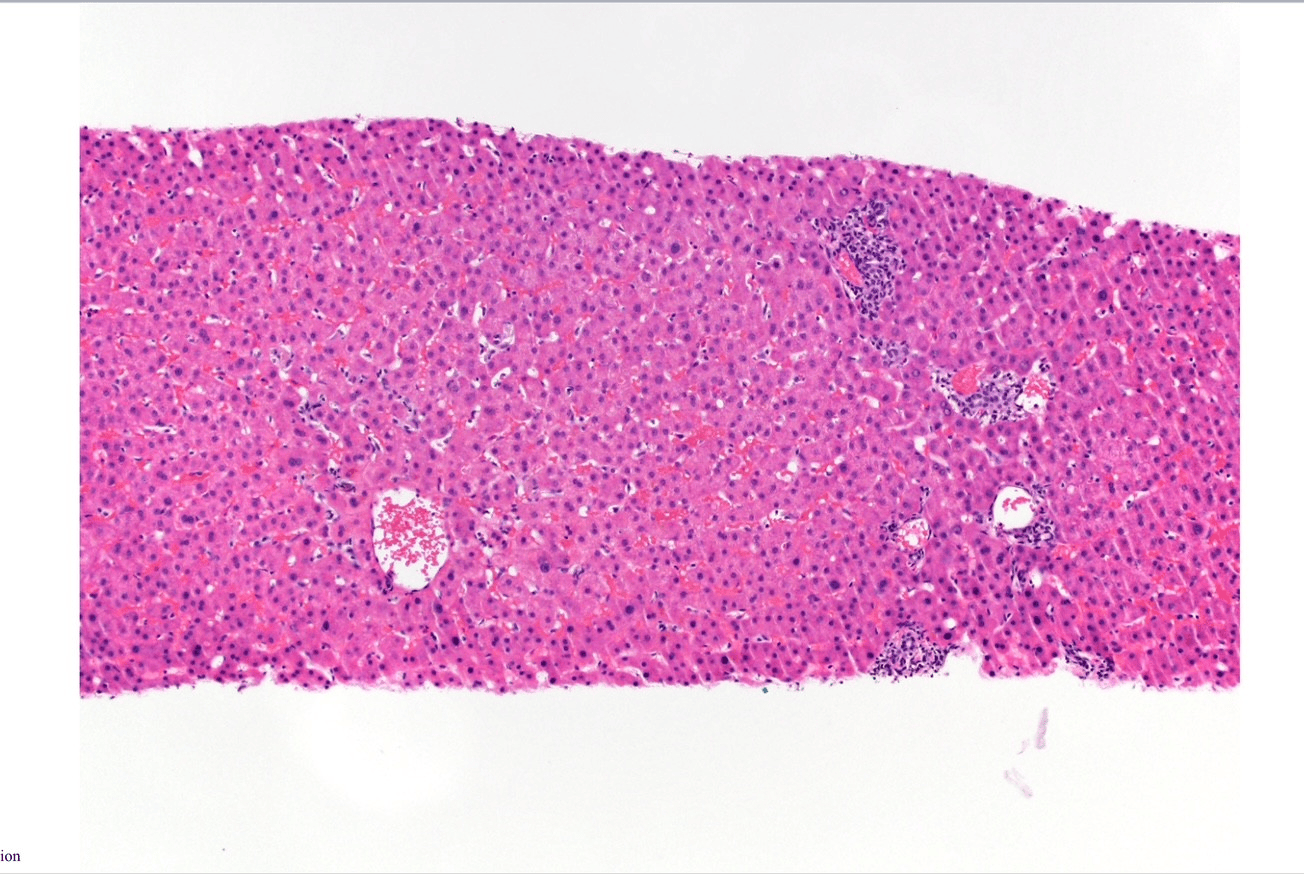
Figure: HEV in fulminant liver failure liver biopsy
Disclosures:
Mina Awadallah indicated no relevant financial relationships.
Avneet Singh indicated no relevant financial relationships.
Gillian Hale indicated no relevant financial relationships.
Mariana Moreno-Prats indicated no relevant financial relationships.
John Erikson Yap: Phathom Pharmaceutical – Speakers Bureau. Steris – Consultant.
Juan Gallegos-Orozco: Gilead – Grant/Research Support. Hanmi – Grant/Research Support. Intercept – Grant/Research Support. Mirum – Grant/Research Support.
Mina Awadallah, MD, MSc1, Avneet Singh, DO2, Gillian Hale, MD, MPH1, Mariana Moreno-Prats, MD1, John Erikson Yap, MD, MBA, FACG3, Juan F. Gallegos-Orozco, MD, FACG3. P6149 - Two Sides of the Same Coin: Contrasting Presentations and Outcomes of Hepatitis E Virus Infection in a Transplant Recipient and an Immunocompetent Host, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
