Tuesday Poster Session
Category: Liver
P6148 - A Severe Case of Drug-Induced Hypersensitivity Syndrome (DIHS) Presenting as Acute Liver Failure Requiring Urgent Liver Transplantation
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mina Awadallah, MD, MSc
University of Utah
Salt Lake City, UT
Presenting Author(s)
Mina Awadallah, MD, MSc1, Joshua Kirkpatrick, MD2, David Jonason, MD1, Christina Necessary, 3, Gillian Hale, MD, MPH1
1University of Utah, Salt Lake City, UT; 2West Virginia University School of Medicine, Morgantown, WV; 3University of Utah School of Medicine, Salt Lake City, UT
Introduction: Drug-Induced Hypersensitivity Syndrome (DIHS), formerly known as Drug Reaction with Eosinophilia and Systemic Symptoms, is a rare but life-threatening condition characterized by delayed-onset systemic inflammation, eosinophilia, and multiorgan involvement. Fulminant liver failure is the leading cause of mortality. We present a case of DIHS leading to acute liver failure and urgent liver transplantation.
Case Description/
Methods: A 65-year-old male with no prior liver disease presented with three weeks of painless jaundice, fatigue, and arthralgias. He had recently started herbal supplements containing multiple botanicals, including ginseng and ashwagandha. He was recently initiated aripiprazole and oral diclofenac 3 week prior.
Initial labs showed AST 2687, ALT 1810, total bilirubin 14.8, INR 1.5 and renal failure. CT scan showed a normal-appearing liver and multifocal lymphadenopathy. Infectious and toxicology screens were negative. Autoimmune serologies showed an abnormal ANA, antimitochondrial antibody IgG, and F-actin IgG raising suspicion for AIH or drug-induced liver injury (DILI).
Liver biopsy revealed a severe active hepatitis with bridging necrosis and marked plasma cell inflammation. Stains for infectious etiologies were negative. On hospital day four, the patient developed worsening INR, acute encephalopathy, and a diffuse morbilliform rash. Liver transplant evaluation was initiated. On hospital day five, new-onset eosinophilia and a RegiSCAR score of 6 raised strong suspicion for DIHS.
Due to rapid liver failure, he underwent urgent liver transplantation on hospital day eight and improved postoperatively. The liver explant showed features of extensive necrosis and parenchymal loss, consistent with acute liver failure.
Discussion: This case highlights the diagnostic challenge of differentiating DIHS from AIH and DILI, particularly in the absence of early eosinophilia. It underscores the importance of considering not only commonly recognized hepatotoxic medications but also potential triggers of DIHS.
DIHS should be considered in patients with progressive liver injury, even without eosinophilia. Diagnosis relies on clinical features and RegiSCAR criteria, which include fever, rash, lymphadenopathy, internal organ involvement, and hematologic abnormalities. While eosinophilia is a hallmark feature, it may be absent initially in up to 31% of cases. This case emphasizes the need for early recognition of DIHS and the potential for severe outcomes requiring liver transplantation.
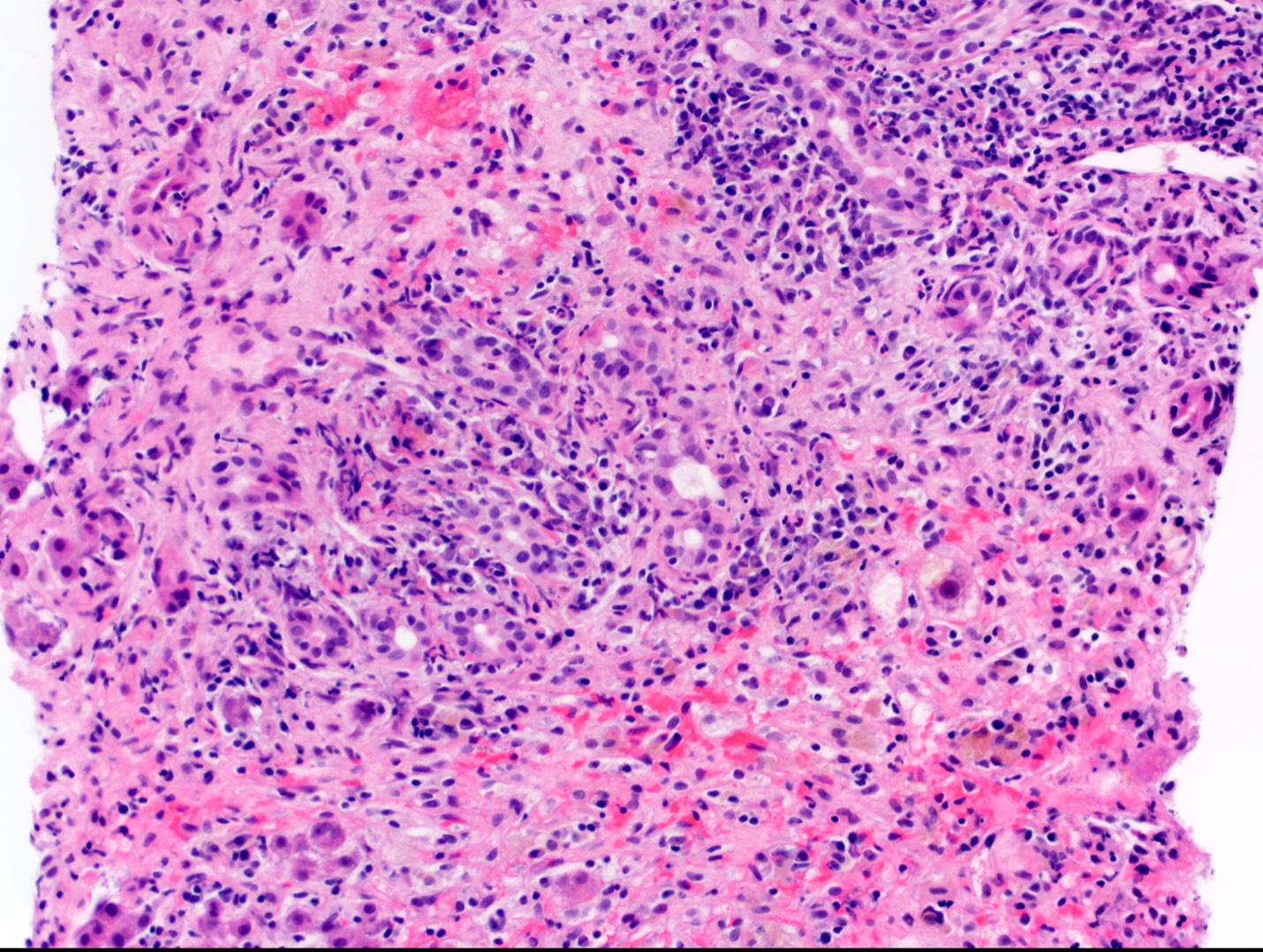
Figure: Liver core needle biopsy demonstrating portal inflammation with bridging necrosis extending along the interface with the lobular parenchyma (H+E stain, 20X).
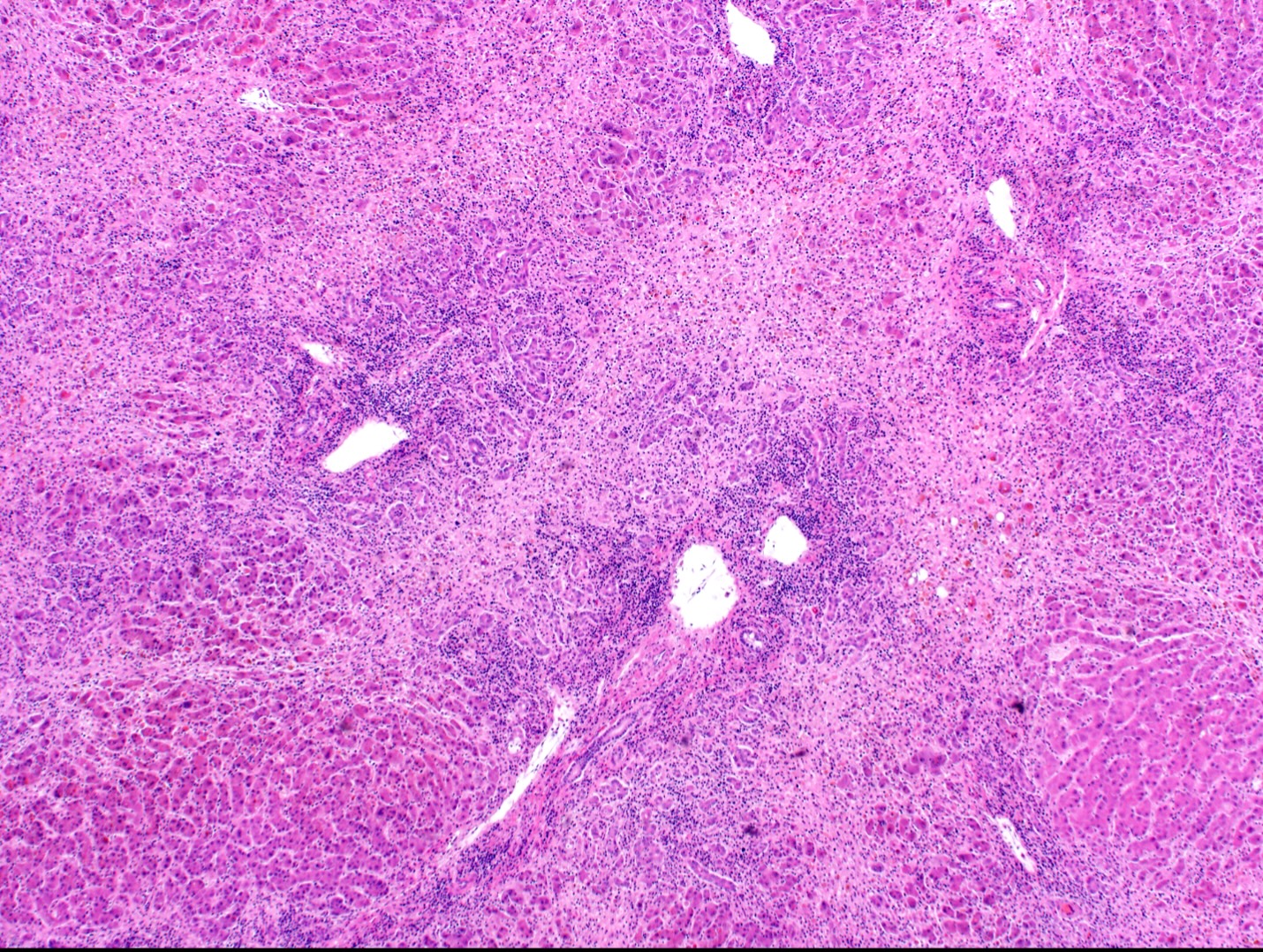
Figure: Liver explant, demonstrating extensive inflammation and nodularity imparted by extensive bridging necrosis (H+E stain, 4X)
Disclosures:
Mina Awadallah indicated no relevant financial relationships.
Joshua Kirkpatrick indicated no relevant financial relationships.
David Jonason indicated no relevant financial relationships.
Christina Necessary indicated no relevant financial relationships.
Gillian Hale indicated no relevant financial relationships.
Mina Awadallah, MD, MSc1, Joshua Kirkpatrick, MD2, David Jonason, MD1, Christina Necessary, 3, Gillian Hale, MD, MPH1. P6148 - A Severe Case of Drug-Induced Hypersensitivity Syndrome (DIHS) Presenting as Acute Liver Failure Requiring Urgent Liver Transplantation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Utah, Salt Lake City, UT; 2West Virginia University School of Medicine, Morgantown, WV; 3University of Utah School of Medicine, Salt Lake City, UT
Introduction: Drug-Induced Hypersensitivity Syndrome (DIHS), formerly known as Drug Reaction with Eosinophilia and Systemic Symptoms, is a rare but life-threatening condition characterized by delayed-onset systemic inflammation, eosinophilia, and multiorgan involvement. Fulminant liver failure is the leading cause of mortality. We present a case of DIHS leading to acute liver failure and urgent liver transplantation.
Case Description/
Methods: A 65-year-old male with no prior liver disease presented with three weeks of painless jaundice, fatigue, and arthralgias. He had recently started herbal supplements containing multiple botanicals, including ginseng and ashwagandha. He was recently initiated aripiprazole and oral diclofenac 3 week prior.
Initial labs showed AST 2687, ALT 1810, total bilirubin 14.8, INR 1.5 and renal failure. CT scan showed a normal-appearing liver and multifocal lymphadenopathy. Infectious and toxicology screens were negative. Autoimmune serologies showed an abnormal ANA, antimitochondrial antibody IgG, and F-actin IgG raising suspicion for AIH or drug-induced liver injury (DILI).
Liver biopsy revealed a severe active hepatitis with bridging necrosis and marked plasma cell inflammation. Stains for infectious etiologies were negative. On hospital day four, the patient developed worsening INR, acute encephalopathy, and a diffuse morbilliform rash. Liver transplant evaluation was initiated. On hospital day five, new-onset eosinophilia and a RegiSCAR score of 6 raised strong suspicion for DIHS.
Due to rapid liver failure, he underwent urgent liver transplantation on hospital day eight and improved postoperatively. The liver explant showed features of extensive necrosis and parenchymal loss, consistent with acute liver failure.
Discussion: This case highlights the diagnostic challenge of differentiating DIHS from AIH and DILI, particularly in the absence of early eosinophilia. It underscores the importance of considering not only commonly recognized hepatotoxic medications but also potential triggers of DIHS.
DIHS should be considered in patients with progressive liver injury, even without eosinophilia. Diagnosis relies on clinical features and RegiSCAR criteria, which include fever, rash, lymphadenopathy, internal organ involvement, and hematologic abnormalities. While eosinophilia is a hallmark feature, it may be absent initially in up to 31% of cases. This case emphasizes the need for early recognition of DIHS and the potential for severe outcomes requiring liver transplantation.
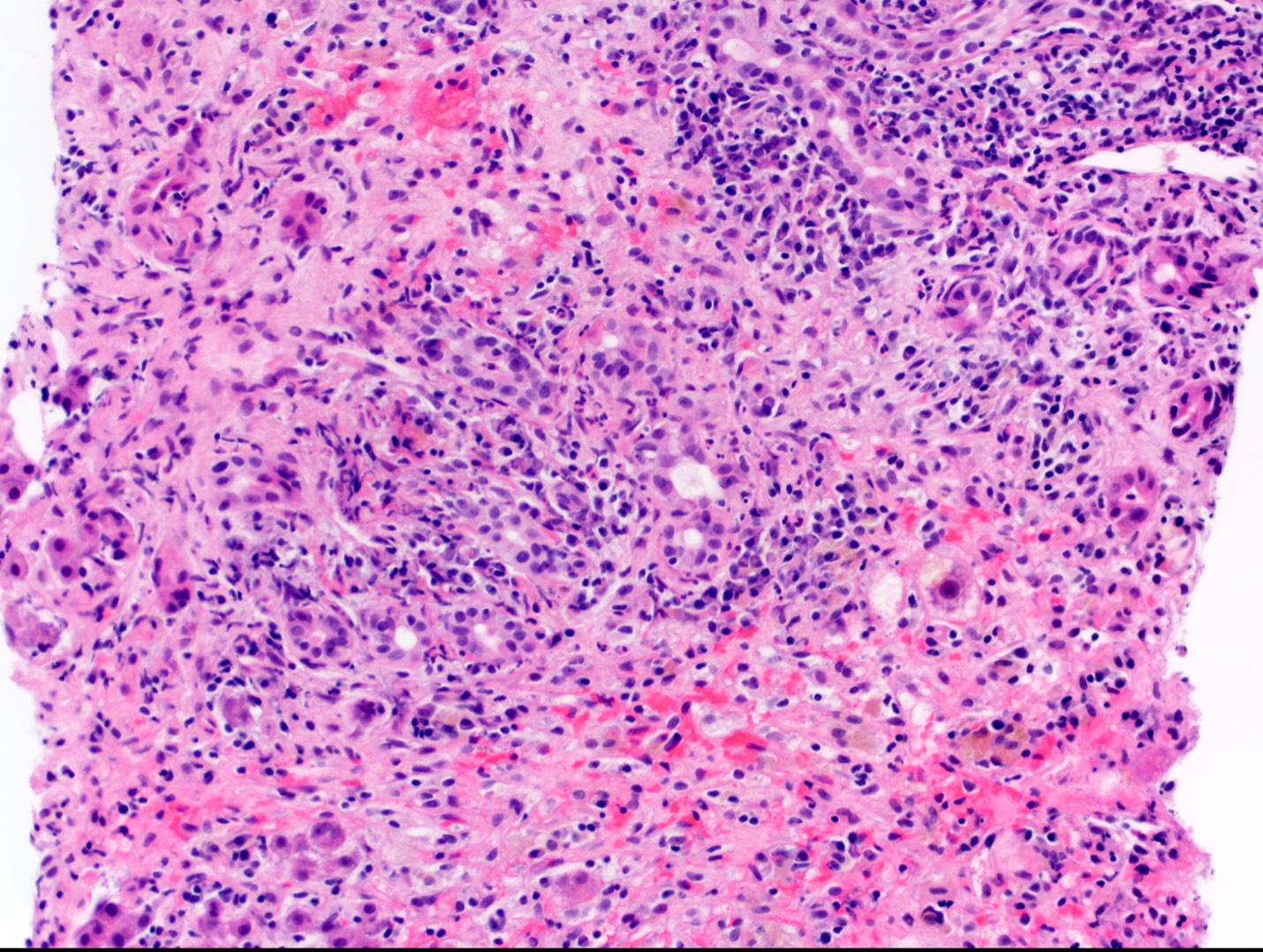
Figure: Liver core needle biopsy demonstrating portal inflammation with bridging necrosis extending along the interface with the lobular parenchyma (H+E stain, 20X).
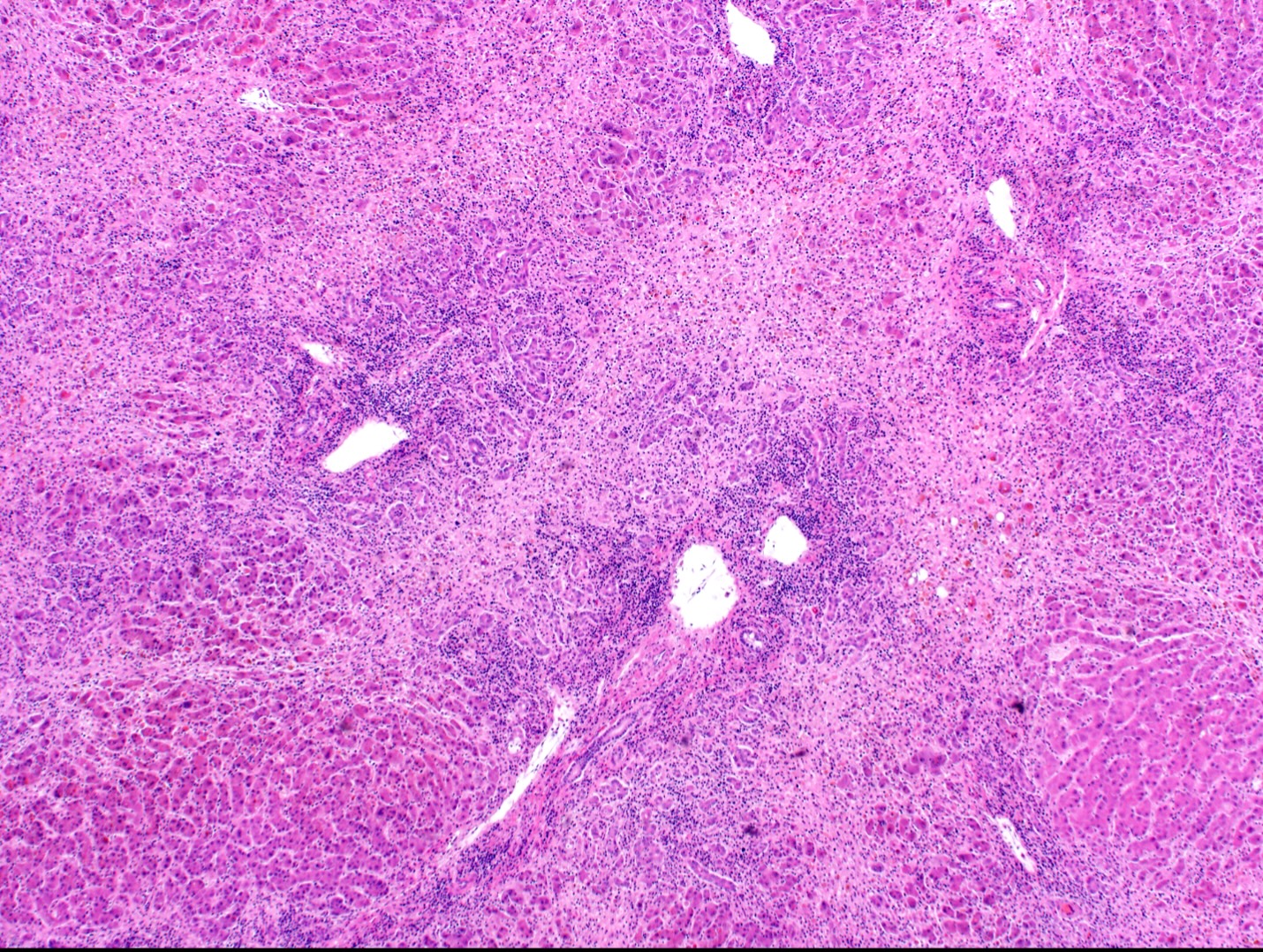
Figure: Liver explant, demonstrating extensive inflammation and nodularity imparted by extensive bridging necrosis (H+E stain, 4X)
Disclosures:
Mina Awadallah indicated no relevant financial relationships.
Joshua Kirkpatrick indicated no relevant financial relationships.
David Jonason indicated no relevant financial relationships.
Christina Necessary indicated no relevant financial relationships.
Gillian Hale indicated no relevant financial relationships.
Mina Awadallah, MD, MSc1, Joshua Kirkpatrick, MD2, David Jonason, MD1, Christina Necessary, 3, Gillian Hale, MD, MPH1. P6148 - A Severe Case of Drug-Induced Hypersensitivity Syndrome (DIHS) Presenting as Acute Liver Failure Requiring Urgent Liver Transplantation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
