Tuesday Poster Session
Category: Liver
P6138 - When the Floodgates Open: A Case of Spontaneous Umbilical Hernia Rupture in Cirrhosis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Rachael Hagen, DO (she/her/hers)
University of Connecticut Health
Farmington, CT
Presenting Author(s)
Rachael Hagen, DO1, Bianca Thakkar, DO1, Minh Thu T.. Nguyen, MD2
1University of Connecticut Health, Farmington, CT; 2University of Connecticut, Farmington, CT
Introduction: Flood syndrome refers to the spontaneous rupture of an umbilical hernia with leakage of ascitic fluid—a rare and serious complication of decompensated cirrhosis. It carries a mortality and morbidity rate of up to 30%. Management is particularly challenging, as surgical options are often limited by the high operative risk associated with cirrhosis and ascites. However, the resulting open abdominal wall defect poses a significant risk for infection and spontaneous bacterial peritonitis (SBP). We present a case of Flood syndrome managed conservatively.
Case Description/
Methods: A 50-year-old male with decompensated metabolic dysfunction-associated steatohepatitis (MASH) cirrhosis presented with large-volume ascites after missing his weekly paracentesis for one month. His Model for End-Stage Liver Disease (MELD) score was 29. During hospitalization, progressive ascites led to umbilical hernia distension and eventual rupture, resulting in persistent drainage of ascitic fluid. Fluid studies were consistent with cirrhosis. Abdominal and pelvic imaging revealed large-volume ascites with umbilical cellulitis and no discrete fluid collection in the umbilicus (Fig. 1). He remained on antibiotics for peritonitis prophylaxis.
He underwent superficial closure of the umbilical defect, with no further surgical intervention performed. Transjugular intrahepatic portosystemic shunt (TIPS) was not recommended due to a high MELD score, which increased procedural risk. He was not a candidate for liver transplantation due to elevated body mass index and chronic portal venous thrombosis. One-week after closure, no further leakage was noted. He resumed weekly paracentesis but remained intolerant of diuretic therapy.
Discussion: Umbilical herniation occurs in 20% of patients with cirrhosis, but rupture is rare and often preceded by skin necrosis. Management involves TIPS, surgical herniorrhaphy, or wound closure, with drains as temporary measures. In this case, a pigtail catheter was avoided due to infection risk. According to the American Gastroenterological Association, hernia repair is not advised in cirrhotic patients with ascites unless bowel incarceration or strangulation is present. Ascites control remains the cornerstone of management. If rupture occurs, conservative management is preferred, with elective repair in select cases. This case highlights the need for an individualized, multidisciplinary approach to managing Flood syndrome.
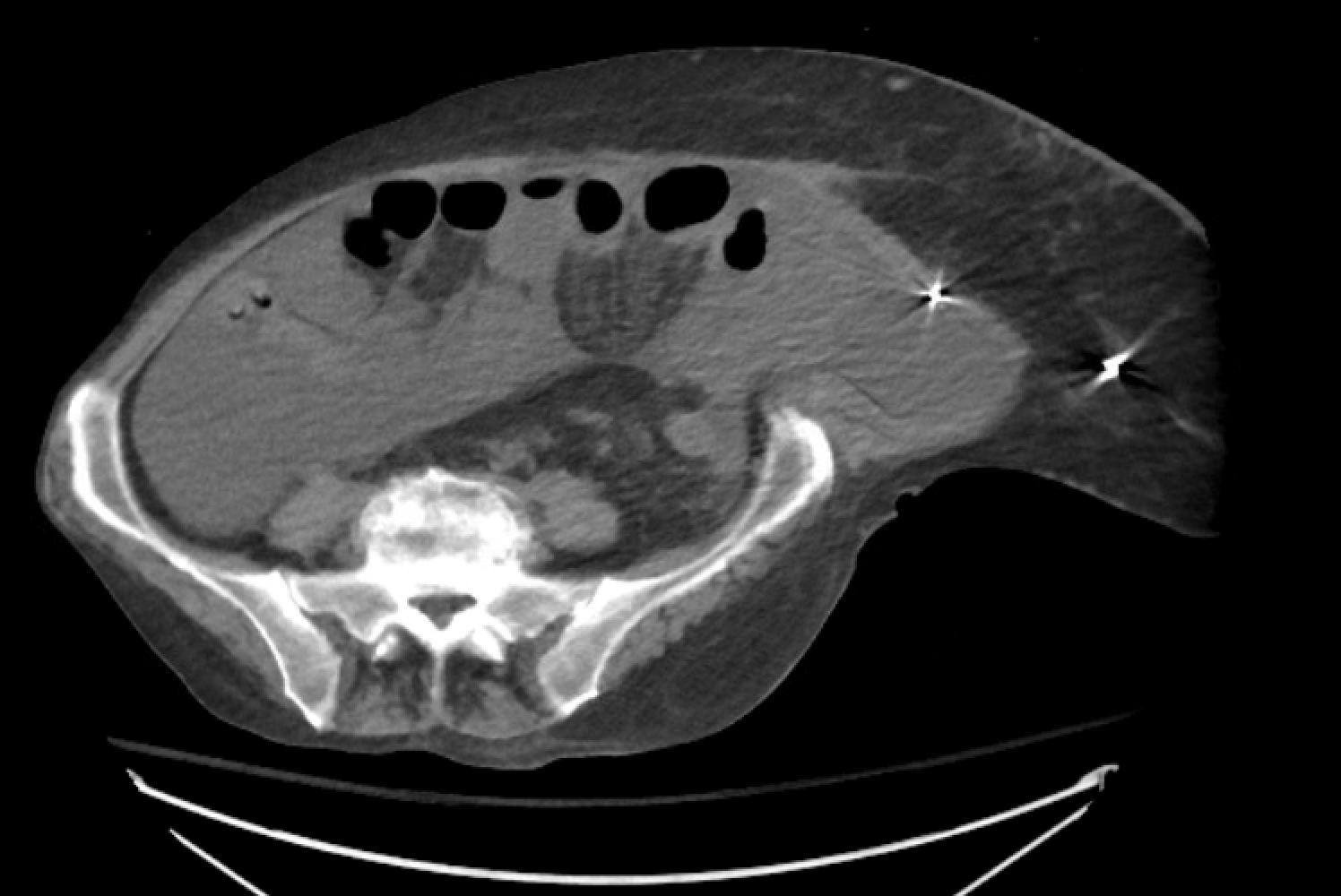
Figure: Figure 1. A CT scan of the abdomen and pelvis revealed large-volume ascites with umbilical cellulitis and no discrete fluid collection in the umbilicus.
Disclosures:
Rachael Hagen indicated no relevant financial relationships.
Bianca Thakkar indicated no relevant financial relationships.
Minh Thu Nguyen indicated no relevant financial relationships.
Rachael Hagen, DO1, Bianca Thakkar, DO1, Minh Thu T.. Nguyen, MD2. P6138 - When the Floodgates Open: A Case of Spontaneous Umbilical Hernia Rupture in Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Connecticut Health, Farmington, CT; 2University of Connecticut, Farmington, CT
Introduction: Flood syndrome refers to the spontaneous rupture of an umbilical hernia with leakage of ascitic fluid—a rare and serious complication of decompensated cirrhosis. It carries a mortality and morbidity rate of up to 30%. Management is particularly challenging, as surgical options are often limited by the high operative risk associated with cirrhosis and ascites. However, the resulting open abdominal wall defect poses a significant risk for infection and spontaneous bacterial peritonitis (SBP). We present a case of Flood syndrome managed conservatively.
Case Description/
Methods: A 50-year-old male with decompensated metabolic dysfunction-associated steatohepatitis (MASH) cirrhosis presented with large-volume ascites after missing his weekly paracentesis for one month. His Model for End-Stage Liver Disease (MELD) score was 29. During hospitalization, progressive ascites led to umbilical hernia distension and eventual rupture, resulting in persistent drainage of ascitic fluid. Fluid studies were consistent with cirrhosis. Abdominal and pelvic imaging revealed large-volume ascites with umbilical cellulitis and no discrete fluid collection in the umbilicus (Fig. 1). He remained on antibiotics for peritonitis prophylaxis.
He underwent superficial closure of the umbilical defect, with no further surgical intervention performed. Transjugular intrahepatic portosystemic shunt (TIPS) was not recommended due to a high MELD score, which increased procedural risk. He was not a candidate for liver transplantation due to elevated body mass index and chronic portal venous thrombosis. One-week after closure, no further leakage was noted. He resumed weekly paracentesis but remained intolerant of diuretic therapy.
Discussion: Umbilical herniation occurs in 20% of patients with cirrhosis, but rupture is rare and often preceded by skin necrosis. Management involves TIPS, surgical herniorrhaphy, or wound closure, with drains as temporary measures. In this case, a pigtail catheter was avoided due to infection risk. According to the American Gastroenterological Association, hernia repair is not advised in cirrhotic patients with ascites unless bowel incarceration or strangulation is present. Ascites control remains the cornerstone of management. If rupture occurs, conservative management is preferred, with elective repair in select cases. This case highlights the need for an individualized, multidisciplinary approach to managing Flood syndrome.
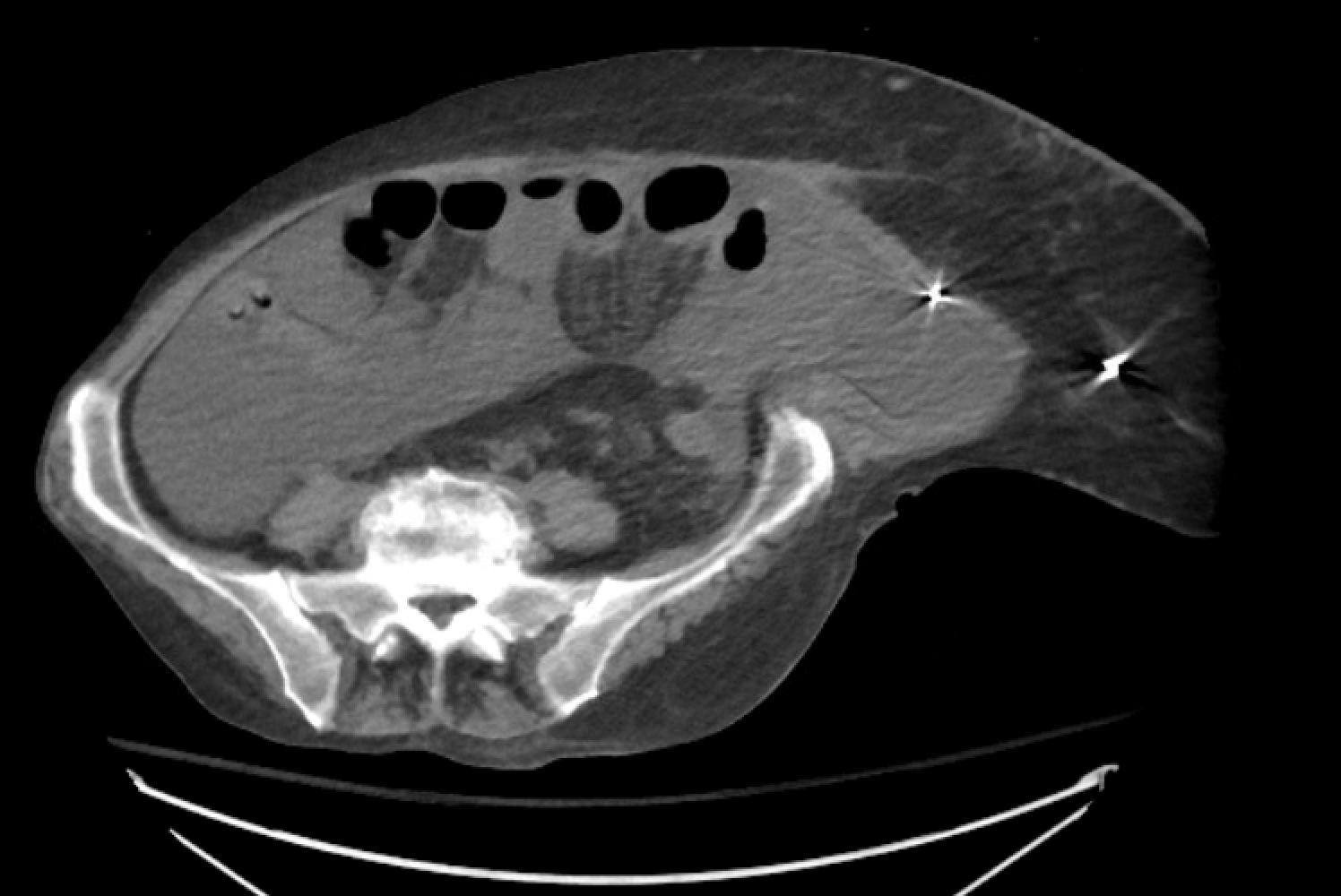
Figure: Figure 1. A CT scan of the abdomen and pelvis revealed large-volume ascites with umbilical cellulitis and no discrete fluid collection in the umbilicus.
Disclosures:
Rachael Hagen indicated no relevant financial relationships.
Bianca Thakkar indicated no relevant financial relationships.
Minh Thu Nguyen indicated no relevant financial relationships.
Rachael Hagen, DO1, Bianca Thakkar, DO1, Minh Thu T.. Nguyen, MD2. P6138 - When the Floodgates Open: A Case of Spontaneous Umbilical Hernia Rupture in Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
