Tuesday Poster Session
Category: Liver
P6137 - From Transplant Candidate to Recovery: A Case of Severe Acetaminophen Overdose With Multisystem Involvement
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Rachael Hagen, DO (she/her/hers)
University of Connecticut Health
Farmington, CT
Presenting Author(s)
Rachael Hagen, DO1, Bianca Thakkar, DO1, Minh Thu T.. Nguyen, MD2, Elizabeth Richardon, DO3
1University of Connecticut Health, Farmington, CT; 2University of Connecticut, Farmington, CT; 3Hartford Hospital, Hartford, CT
Introduction: Acetaminophen is among the most widely used analgesics. While safe at therapeutic doses, both intentional and unintentional overdose remain the leading causes of acute liver failure in the United States. Renal failure is also common, whereas involvement of other organ systems is rare. We present a case of acetaminophen toxicity with thrombocytopenia and cardiac inflammation, followed by full recovery.
Case Description/
Methods: A 32-year-old male was admitted for intentional ingestion of 30 acetaminophen tablets. He consumed 10 beers weekly. Laboratory findings revealed an elevated acetaminophen level (70 mg/L), low platelet count (3,000/μL), creatinine of 0.7 mg/dL, alanine and aspartate aminotransferase of 10,706 and >14,000 U/L, elevated ammonia (93 μmol/L), INR of 6.4, and a Model of End-Stage Liver Disease (MELD) score of 41. Continuous N-acetylcysteine (NAC) therapy was initiated. Abdominal ultrasound showed hepatomegaly with fatty infiltration, also seen on computed tomography (Fig. 1). The patient’s mentation remained intact. Hematology attributed the thrombocytopenia to acetaminophen toxicity.
Two days later, he developed chest pain and elevated troponins (peak 1,300 ng/L), accompanied by inferolateral ST elevations (Fig. 2). Echocardiogram was unremarkable. Cardiac catheterization was deferred, as the findings were consistent with myopericarditis from liver dysfunction. Although initially evaluated for liver transplantation, his clinical status and laboratory values improved significantly. He was discharged home on hospital day 13 with psychiatric follow-up.
Discussion: Drug-induced thrombocytopenia is rare but has been reported in cases of acetaminophen overdose, likely due to a direct toxicity to platelets or megakaryocytes. In this case, the temporal association with rapid recovery supported acetaminophen as the underlying cause. Blood product transfusion is typically reserved for active bleeding rather than correction of coagulopathy alone. Similarly, the ST elevations were attributed to myopericarditis secondary to hepatic injury, as acetaminophen is not directly cardiotoxic but may trigger hypersensitivity or allergic responses.
In acetaminophen toxicity, monitoring ammonia is critical due to the risk of cerebral edema. Although the patient met King’s College Criteria for transplantation, conservative management with continued NAC use led to substantial improvement. This case underscores the potential for recovery despite severe hematologic, cardiac, and renal abnormalities.
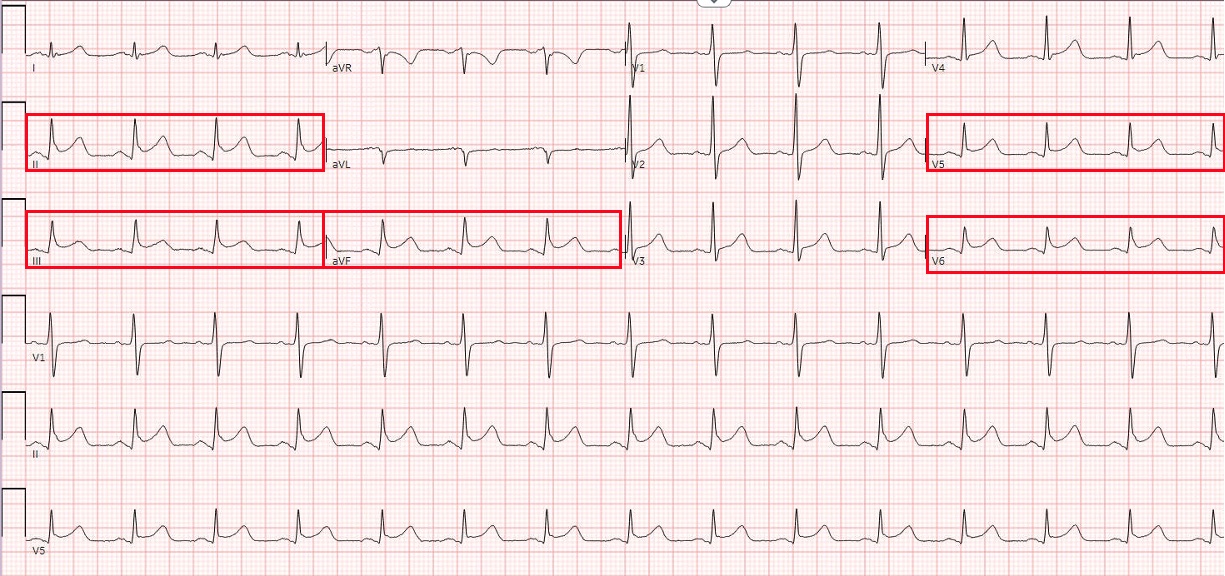
Figure: Figure 1. Abdominal ultrasound demonstrated hepatic steatosis.

Figure: Figure 2. EKG showed ST elevations in inferolateral leads, likely due to myopericarditis secondary to liver injury.
Disclosures:
Rachael Hagen indicated no relevant financial relationships.
Bianca Thakkar indicated no relevant financial relationships.
Minh Thu Nguyen indicated no relevant financial relationships.
Elizabeth Richardon indicated no relevant financial relationships.
Rachael Hagen, DO1, Bianca Thakkar, DO1, Minh Thu T.. Nguyen, MD2, Elizabeth Richardon, DO3. P6137 - From Transplant Candidate to Recovery: A Case of Severe Acetaminophen Overdose With Multisystem Involvement, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Connecticut Health, Farmington, CT; 2University of Connecticut, Farmington, CT; 3Hartford Hospital, Hartford, CT
Introduction: Acetaminophen is among the most widely used analgesics. While safe at therapeutic doses, both intentional and unintentional overdose remain the leading causes of acute liver failure in the United States. Renal failure is also common, whereas involvement of other organ systems is rare. We present a case of acetaminophen toxicity with thrombocytopenia and cardiac inflammation, followed by full recovery.
Case Description/
Methods: A 32-year-old male was admitted for intentional ingestion of 30 acetaminophen tablets. He consumed 10 beers weekly. Laboratory findings revealed an elevated acetaminophen level (70 mg/L), low platelet count (3,000/μL), creatinine of 0.7 mg/dL, alanine and aspartate aminotransferase of 10,706 and >14,000 U/L, elevated ammonia (93 μmol/L), INR of 6.4, and a Model of End-Stage Liver Disease (MELD) score of 41. Continuous N-acetylcysteine (NAC) therapy was initiated. Abdominal ultrasound showed hepatomegaly with fatty infiltration, also seen on computed tomography (Fig. 1). The patient’s mentation remained intact. Hematology attributed the thrombocytopenia to acetaminophen toxicity.
Two days later, he developed chest pain and elevated troponins (peak 1,300 ng/L), accompanied by inferolateral ST elevations (Fig. 2). Echocardiogram was unremarkable. Cardiac catheterization was deferred, as the findings were consistent with myopericarditis from liver dysfunction. Although initially evaluated for liver transplantation, his clinical status and laboratory values improved significantly. He was discharged home on hospital day 13 with psychiatric follow-up.
Discussion: Drug-induced thrombocytopenia is rare but has been reported in cases of acetaminophen overdose, likely due to a direct toxicity to platelets or megakaryocytes. In this case, the temporal association with rapid recovery supported acetaminophen as the underlying cause. Blood product transfusion is typically reserved for active bleeding rather than correction of coagulopathy alone. Similarly, the ST elevations were attributed to myopericarditis secondary to hepatic injury, as acetaminophen is not directly cardiotoxic but may trigger hypersensitivity or allergic responses.
In acetaminophen toxicity, monitoring ammonia is critical due to the risk of cerebral edema. Although the patient met King’s College Criteria for transplantation, conservative management with continued NAC use led to substantial improvement. This case underscores the potential for recovery despite severe hematologic, cardiac, and renal abnormalities.
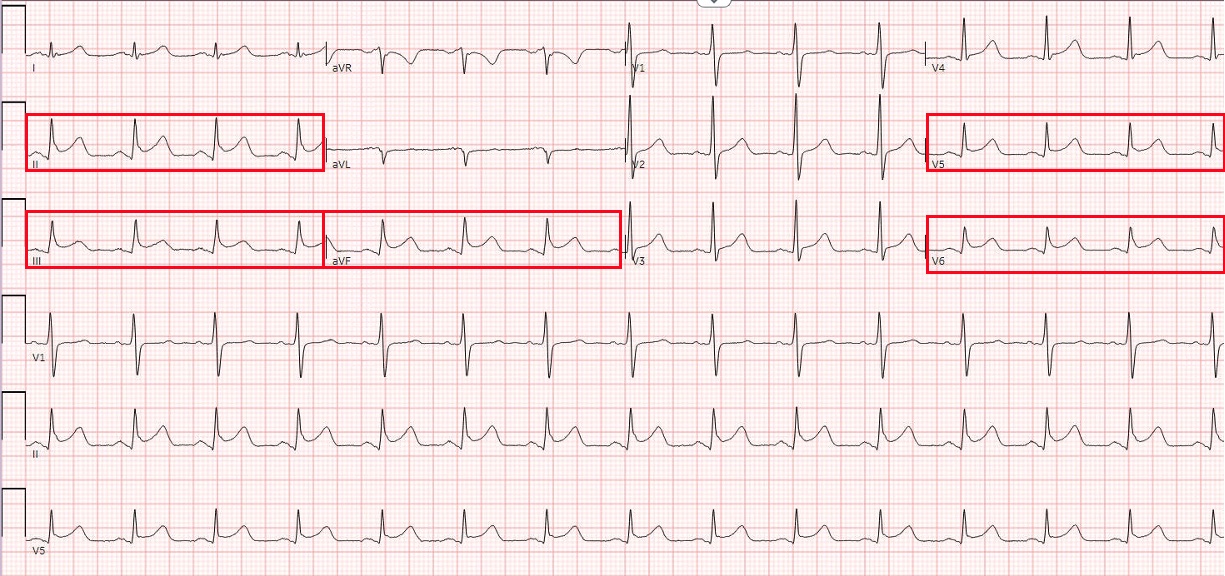
Figure: Figure 1. Abdominal ultrasound demonstrated hepatic steatosis.

Figure: Figure 2. EKG showed ST elevations in inferolateral leads, likely due to myopericarditis secondary to liver injury.
Disclosures:
Rachael Hagen indicated no relevant financial relationships.
Bianca Thakkar indicated no relevant financial relationships.
Minh Thu Nguyen indicated no relevant financial relationships.
Elizabeth Richardon indicated no relevant financial relationships.
Rachael Hagen, DO1, Bianca Thakkar, DO1, Minh Thu T.. Nguyen, MD2, Elizabeth Richardon, DO3. P6137 - From Transplant Candidate to Recovery: A Case of Severe Acetaminophen Overdose With Multisystem Involvement, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
