Tuesday Poster Session
Category: Small Intestine
P6232 - Nerve Matters: A Case of Duodenal Ganglioneuroma
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Samuel Cheong, DO
University of Arizona College of Medicine
Tucson, AZ
Presenting Author(s)
Brandon Witten, MD1, Samuel Cheong, DO1, Natasha Khona, DO1, Mohamad Omar Diab, MD2, Gebran Abboud, MD1, Achyut Bhattacharyya, MD1, Hemanth Gavini, MD3
1Banner - University of Arizona Tucson, Tucson, AZ; 2Canyon Vista Medical Center, Sierra Vista, AZ; 3George Washington University School of Medicine and Health Sciences, Washington, DC
Introduction: Duodenal ganglioneuromas are a rare, benign neoplasm. Involvement in the duodenum has been described in the literature, mainly affecting pediatric patients. Incidence in adults is exceedingly sparse with only a few case reports describing this phenomenon. This case report highlights the clinical presentation, diagnostic process, and management of a patient with duodenal ganglioneuroma.
Case Description/
Methods: 60-year-old female with a history of ovarian cancer presented to our institution for interventional GI evaluation after a hyperattenuating lesion was discovered on CT abdomen/pelvis. Prior EGD performed at an outside facility investigating this area showed a subepithelial nodule in the second part of the duodenum near the ampulla. Biopsies of the surface mucosa in that area had showed benign duodenal mucosa along with findings suggestive of peptic duodenitis. Due to the subepithelial nature of the lesion, endoscopic ultrasound(EUS) was performed which showed a 13mm hypoechoic lesion within the submucosal layer. A fine needle biopsy(FNB) was performed and pathology demonstrated neuroectodermal derived neoplasm likely representing a ganglioneuroma versus a low-grade neuroendocrine tumor. After a multidisciplinary discussion at the tumor board, the decision was made to perform endoscopic resection of this lesion. The lesion was resected enbloc with endoscopic mucosal resection(EMR). Pathology showed mature ganglion cells within a wavy stroma of spindle cells that was strongly positive for chromogranin, S100, synaptophysin and CD163 consistent with a ganglioneuroma with margins free of tumor. Patient was recommended to undergo yearly EGD/EUS for surveillance.
Discussion: Duodenal ganglioneuroma is an exceedingly rare entity, with approximately five cases reported in adults to date. Our presentation was consistent with how these have typically manifested in previously reported cases, as slow growing, benign and incidentally found lesions. While the exact etiology remains unclear, these tumors have been associated with genetic syndromes such as multiple endocrine neoplasia (MEN) type 2 and neurofibromatosis. However, sporadic cases, like the one presented here, are more common.
This case highlights the importance of considering duodenal ganglioneuroma in the differential diagnosis of subepithelial gastrointestinal tumors. While rare, these benign tumors are treatable with endoscopic mucosal/submucosal resection, leading to excellent outcomes.
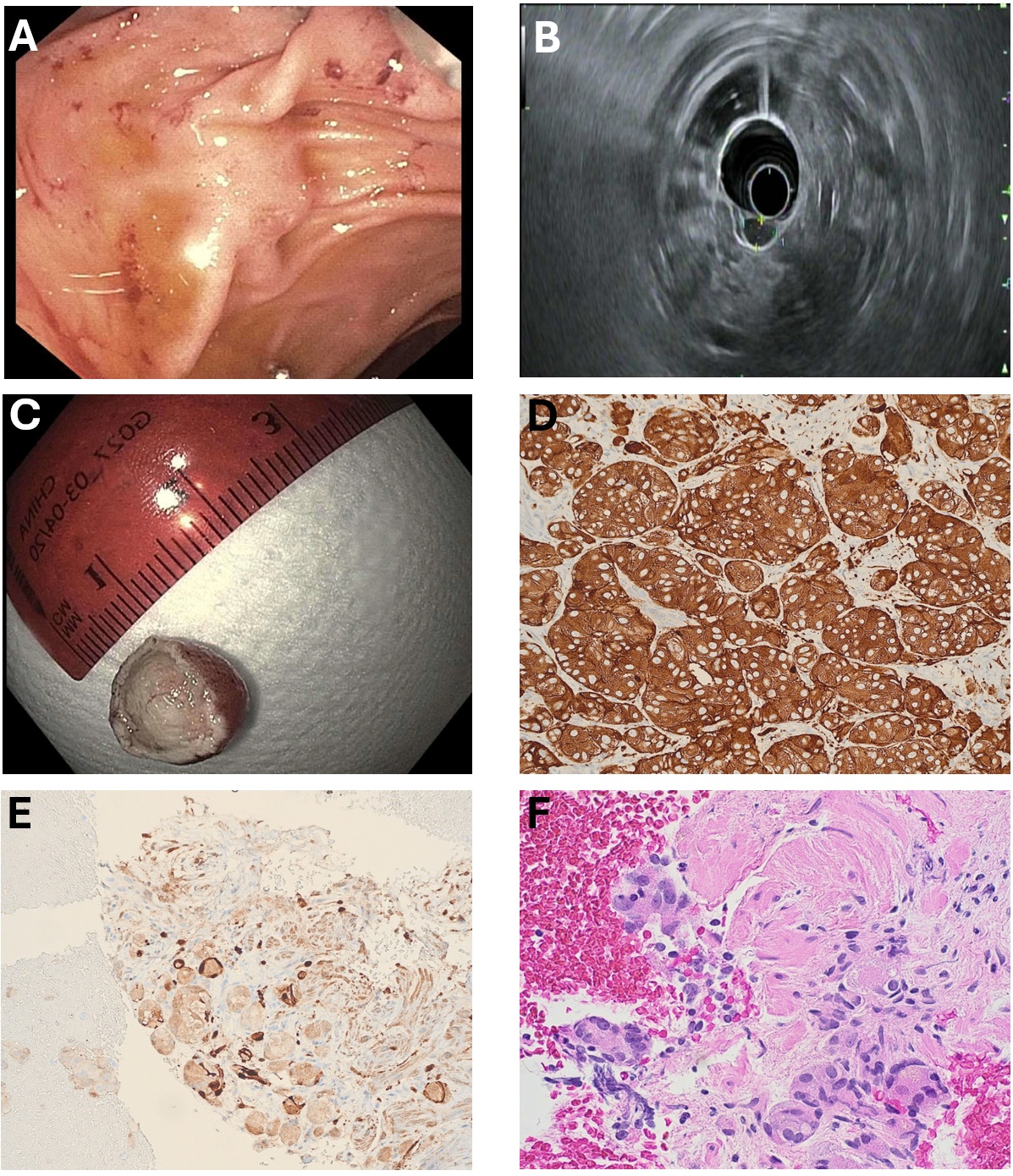
Figure: A: Endoscopic view of duodenal nodule located near the ampulla
B: Endoscopic ultrasound view of duodenal nodule showing extent of spread into the mucosa
C: En bloc resected EMR duodenal nodule
D: Synaptophysin immunohistochemical stain is positive in the neoplastic cells (H&E x400)
E: S100 immunohistochemical stain is positive in the ganglion cells and stroma consistent with ganglioneuroma (S100 x400)
F: H&E cell block from fine needle aspiration showing large ganglion cells with a background of bland spindle cells and wavy fibrillary stroma (H&E x400)
Disclosures:
Brandon Witten indicated no relevant financial relationships.
Samuel Cheong indicated no relevant financial relationships.
Natasha Khona indicated no relevant financial relationships.
Mohamad Omar Diab indicated no relevant financial relationships.
Gebran Abboud indicated no relevant financial relationships.
Achyut Bhattacharyya indicated no relevant financial relationships.
Hemanth Gavini indicated no relevant financial relationships.
Brandon Witten, MD1, Samuel Cheong, DO1, Natasha Khona, DO1, Mohamad Omar Diab, MD2, Gebran Abboud, MD1, Achyut Bhattacharyya, MD1, Hemanth Gavini, MD3. P6232 - Nerve Matters: A Case of Duodenal Ganglioneuroma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Banner - University of Arizona Tucson, Tucson, AZ; 2Canyon Vista Medical Center, Sierra Vista, AZ; 3George Washington University School of Medicine and Health Sciences, Washington, DC
Introduction: Duodenal ganglioneuromas are a rare, benign neoplasm. Involvement in the duodenum has been described in the literature, mainly affecting pediatric patients. Incidence in adults is exceedingly sparse with only a few case reports describing this phenomenon. This case report highlights the clinical presentation, diagnostic process, and management of a patient with duodenal ganglioneuroma.
Case Description/
Methods: 60-year-old female with a history of ovarian cancer presented to our institution for interventional GI evaluation after a hyperattenuating lesion was discovered on CT abdomen/pelvis. Prior EGD performed at an outside facility investigating this area showed a subepithelial nodule in the second part of the duodenum near the ampulla. Biopsies of the surface mucosa in that area had showed benign duodenal mucosa along with findings suggestive of peptic duodenitis. Due to the subepithelial nature of the lesion, endoscopic ultrasound(EUS) was performed which showed a 13mm hypoechoic lesion within the submucosal layer. A fine needle biopsy(FNB) was performed and pathology demonstrated neuroectodermal derived neoplasm likely representing a ganglioneuroma versus a low-grade neuroendocrine tumor. After a multidisciplinary discussion at the tumor board, the decision was made to perform endoscopic resection of this lesion. The lesion was resected enbloc with endoscopic mucosal resection(EMR). Pathology showed mature ganglion cells within a wavy stroma of spindle cells that was strongly positive for chromogranin, S100, synaptophysin and CD163 consistent with a ganglioneuroma with margins free of tumor. Patient was recommended to undergo yearly EGD/EUS for surveillance.
Discussion: Duodenal ganglioneuroma is an exceedingly rare entity, with approximately five cases reported in adults to date. Our presentation was consistent with how these have typically manifested in previously reported cases, as slow growing, benign and incidentally found lesions. While the exact etiology remains unclear, these tumors have been associated with genetic syndromes such as multiple endocrine neoplasia (MEN) type 2 and neurofibromatosis. However, sporadic cases, like the one presented here, are more common.
This case highlights the importance of considering duodenal ganglioneuroma in the differential diagnosis of subepithelial gastrointestinal tumors. While rare, these benign tumors are treatable with endoscopic mucosal/submucosal resection, leading to excellent outcomes.
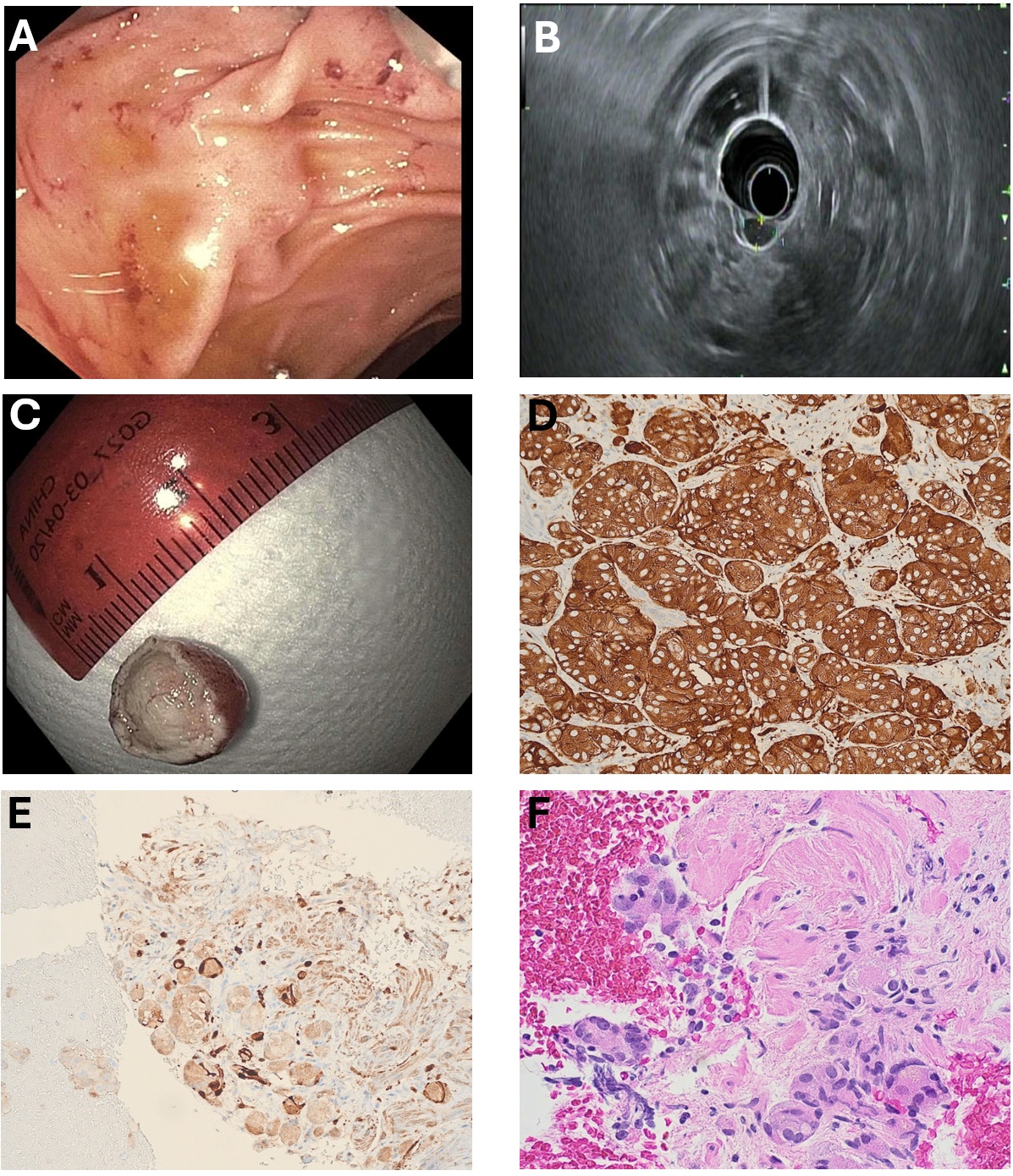
Figure: A: Endoscopic view of duodenal nodule located near the ampulla
B: Endoscopic ultrasound view of duodenal nodule showing extent of spread into the mucosa
C: En bloc resected EMR duodenal nodule
D: Synaptophysin immunohistochemical stain is positive in the neoplastic cells (H&E x400)
E: S100 immunohistochemical stain is positive in the ganglion cells and stroma consistent with ganglioneuroma (S100 x400)
F: H&E cell block from fine needle aspiration showing large ganglion cells with a background of bland spindle cells and wavy fibrillary stroma (H&E x400)
Disclosures:
Brandon Witten indicated no relevant financial relationships.
Samuel Cheong indicated no relevant financial relationships.
Natasha Khona indicated no relevant financial relationships.
Mohamad Omar Diab indicated no relevant financial relationships.
Gebran Abboud indicated no relevant financial relationships.
Achyut Bhattacharyya indicated no relevant financial relationships.
Hemanth Gavini indicated no relevant financial relationships.
Brandon Witten, MD1, Samuel Cheong, DO1, Natasha Khona, DO1, Mohamad Omar Diab, MD2, Gebran Abboud, MD1, Achyut Bhattacharyya, MD1, Hemanth Gavini, MD3. P6232 - Nerve Matters: A Case of Duodenal Ganglioneuroma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
