Tuesday Poster Session
Category: Small Intestine
P6229 - Vagal Nerve Stimulation-Induced Gastrointestinal Dysmotility and Megaduodenum: A Case of Intractable Nausea and Vomiting Resolved by Device Deactivation
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

John Pueringer, DO
University of Illinois College of Medicine
Chicago, IL
Presenting Author(s)
John Pueringer, DO, Jasson Barrios, , Krsna Kothari, MD, Anne Polick, MD
University of Illinois College of Medicine, Chicago, IL
Introduction: Vagal nerve stimulation (VNS) is an established treatment for refractory epilepsy. Common side effects include cough, hoarseness, voice alteration, and paresthesia [1]. Less commonly, nausea and vomiting may occur [2]. Though generally well-tolerated, VSN-related gastrointestinal (GI) effects can be underrecognized, particularly in patients with complex medical histories [3]. To our knowledge, this is the first case report of an adult with intractable nausea and vomiting, attributed to VNS-induced GI dysmotility and megaduodenum, necessitating device deactivation for recovery.
Case Description/
Methods:
A 25-year-old woman with epilepsy due to polymicrogyria (VNS placed 10 years prior), duodenal atresia requiring multiple surgeries (most recently duodenojejunostomy), and megaduodenum presented with severe nausea, vomiting, fatigue, weakness, and poor oral intake. BMI was 13.5. Vitals showed tachycardia (141 bpm), hypotension (97/55 mmHg), tachypnea (32 bpm), and O₂ sat of 88%. Labs showed lactic acidosis (7.0 mmol/L), leukocytosis ( >23,000/μL), elevated creatinine (1.33 mg/dL from 0.66), and metabolic acidosis (pH 7.18, HCO₃ 16).
She was treated empirically for intra-abdominal infection and admitted to the ICU for presumed hypovolemic vs. septic shock, which resolved with fluids and vasopressors. Abdominal CT revealed megaduodenum with proximal jejunal dilation (Figure 1). Extensive workup (including EGD and enteroscopy) found no structural cause. EGD suctioned 2300 cc of retained fluid, improving her pain. She was started on TPN.
Given persistent symptoms, her VNS was deactivated, followed by 48-hour EEG monitoring. Post-deactivation, her nausea and vomiting resolved, oral intake improved, and no seizures occurred. She was discharged with neurology follow-up and a plan for gradual VNS reprogramming. At 6-month follow-up, she remained asymptomatic with a 16-lb weight gain.
Discussion: Deactivation of the VNS led to resolution of the patient’s nausea and vomiting, highlighting the importance of considering VNS-related GI side effects. This case illustrates the need to recognize systemic effects of VNS and the role of cognitive bias in diagnostics. Her complex anatomy initially led clinicians to suspect a structural issue. The device was deactivated on hospital day 17, with symptom improvement. In hindsight, earlier evaluation of the VNS might have avoided prior interventions. Her response offers a framework for managing similar cases with tailored VNS reprogramming.
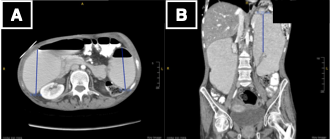
Figure: Figure 1: CT imaging showing A) axial view with markedly dilated descending portion of the duodenum measuring up to 8.9 cm in diameter and proximal jejunum dilated to 8.2 cm, and B) coronal view with descending portion of the duodenum measuring up to 11.
Disclosures:
John Pueringer indicated no relevant financial relationships.
Jasson Barrios indicated no relevant financial relationships.
Krsna Kothari indicated no relevant financial relationships.
Anne Polick indicated no relevant financial relationships.
John Pueringer, DO, Jasson Barrios, , Krsna Kothari, MD, Anne Polick, MD. P6229 - Vagal Nerve Stimulation-Induced Gastrointestinal Dysmotility and Megaduodenum: A Case of Intractable Nausea and Vomiting Resolved by Device Deactivation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Illinois College of Medicine, Chicago, IL
Introduction: Vagal nerve stimulation (VNS) is an established treatment for refractory epilepsy. Common side effects include cough, hoarseness, voice alteration, and paresthesia [1]. Less commonly, nausea and vomiting may occur [2]. Though generally well-tolerated, VSN-related gastrointestinal (GI) effects can be underrecognized, particularly in patients with complex medical histories [3]. To our knowledge, this is the first case report of an adult with intractable nausea and vomiting, attributed to VNS-induced GI dysmotility and megaduodenum, necessitating device deactivation for recovery.
Case Description/
Methods:
A 25-year-old woman with epilepsy due to polymicrogyria (VNS placed 10 years prior), duodenal atresia requiring multiple surgeries (most recently duodenojejunostomy), and megaduodenum presented with severe nausea, vomiting, fatigue, weakness, and poor oral intake. BMI was 13.5. Vitals showed tachycardia (141 bpm), hypotension (97/55 mmHg), tachypnea (32 bpm), and O₂ sat of 88%. Labs showed lactic acidosis (7.0 mmol/L), leukocytosis ( >23,000/μL), elevated creatinine (1.33 mg/dL from 0.66), and metabolic acidosis (pH 7.18, HCO₃ 16).
She was treated empirically for intra-abdominal infection and admitted to the ICU for presumed hypovolemic vs. septic shock, which resolved with fluids and vasopressors. Abdominal CT revealed megaduodenum with proximal jejunal dilation (Figure 1). Extensive workup (including EGD and enteroscopy) found no structural cause. EGD suctioned 2300 cc of retained fluid, improving her pain. She was started on TPN.
Given persistent symptoms, her VNS was deactivated, followed by 48-hour EEG monitoring. Post-deactivation, her nausea and vomiting resolved, oral intake improved, and no seizures occurred. She was discharged with neurology follow-up and a plan for gradual VNS reprogramming. At 6-month follow-up, she remained asymptomatic with a 16-lb weight gain.
Discussion: Deactivation of the VNS led to resolution of the patient’s nausea and vomiting, highlighting the importance of considering VNS-related GI side effects. This case illustrates the need to recognize systemic effects of VNS and the role of cognitive bias in diagnostics. Her complex anatomy initially led clinicians to suspect a structural issue. The device was deactivated on hospital day 17, with symptom improvement. In hindsight, earlier evaluation of the VNS might have avoided prior interventions. Her response offers a framework for managing similar cases with tailored VNS reprogramming.
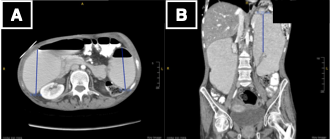
Figure: Figure 1: CT imaging showing A) axial view with markedly dilated descending portion of the duodenum measuring up to 8.9 cm in diameter and proximal jejunum dilated to 8.2 cm, and B) coronal view with descending portion of the duodenum measuring up to 11.
Disclosures:
John Pueringer indicated no relevant financial relationships.
Jasson Barrios indicated no relevant financial relationships.
Krsna Kothari indicated no relevant financial relationships.
Anne Polick indicated no relevant financial relationships.
John Pueringer, DO, Jasson Barrios, , Krsna Kothari, MD, Anne Polick, MD. P6229 - Vagal Nerve Stimulation-Induced Gastrointestinal Dysmotility and Megaduodenum: A Case of Intractable Nausea and Vomiting Resolved by Device Deactivation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
