Tuesday Poster Session
Category: Stomach and Spleen
P6380 - Gastric Ischemia
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- SN
Stephany Nguyen, MD
LSU Health New Orleans School of Medicine
New Orleans, LA
Presenting Author(s)
Stephany Nguyen, MD, Daniel Holmes, MD
LSU Health New Orleans School of Medicine, New Orleans, LA
Introduction: Gastric ischemia is uncommon due to the vast vascular supply of the stomach. Risk factors for gastric ischemia include atherosclerosis, vasculitis, gastric volvulus, DIC, shock, and post-surgical complication. This case aims to increase the index of suspicion for gastric ischemia, which has an overall poor prognosis.
Case Description/
Methods: A 73-year-old male with a history of hypertension and diabetes presented with severe abdominal pain and emesis for one day. He had an episode of bright red blood per rectum at the outside hospital. He was hypotensive and hypothermic with a WBC 21.1, hemoglobin 11.2, and lactic acid 20. He was intubated due to declining GCS. He required initiation of two pressors and broad-spectrum antibiotics. Initial nasogastric tube output was notably dark, and he was started on IV pantoprazole twice daily as well. CTA abdomen was concerning for active hemorrhage in his stomach. Emergent EGD showed a subjectively ischemic greater curvature of the stomach with congested, hemorrhagic, pale, and friable mucosa. Surgical intervention was deferred given patient was an overall poor surgical candidate.
Discussion: Endoscopic findings that are suggestive of gastric ischemia vary based on etiology and whether it’s acute or chronic. Findings may include pale mucosa, congested mucosa, hemorrhagic mucosa, ulcerations, or necrosis. In a case series of fifteen patients, the most common location was the greater curvature of the stomach. Management of gastric ischemia involves nasogastric tube decompression (ischemia can be exacerbated by gastric distension), initiation of a proton pump inhibitor, and interventional radiology or surgery consultation depending on the etiology. Unfortunately, the prognosis of gastric ischemia remains poor despite these measures.

Figure: Figure 1: Initial non-contrast CT AP with normal appearance of the stomach.
Figure 2: CTA AP one day later with active intraluminal contrast extravasation pooling within the depending gastric fundus.
Figure 3: CTA AP demonstrating interval development of intraperitoneal free fluid and colonic distension.
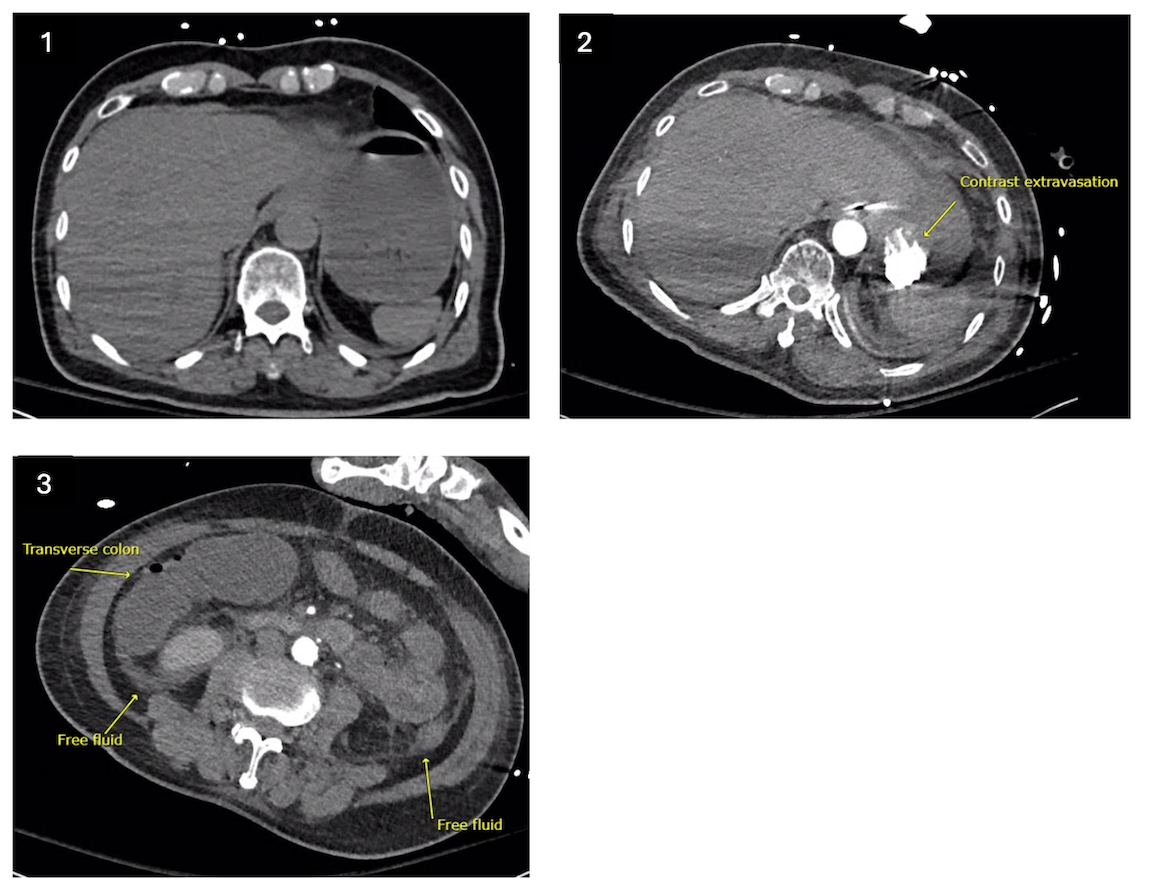
Figure: Figure 4: EGD revealing friable mucosa and hematin in the stomach.
Disclosures:
Stephany Nguyen indicated no relevant financial relationships.
Daniel Holmes indicated no relevant financial relationships.
Stephany Nguyen, MD, Daniel Holmes, MD. P6380 - Gastric Ischemia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
LSU Health New Orleans School of Medicine, New Orleans, LA
Introduction: Gastric ischemia is uncommon due to the vast vascular supply of the stomach. Risk factors for gastric ischemia include atherosclerosis, vasculitis, gastric volvulus, DIC, shock, and post-surgical complication. This case aims to increase the index of suspicion for gastric ischemia, which has an overall poor prognosis.
Case Description/
Methods: A 73-year-old male with a history of hypertension and diabetes presented with severe abdominal pain and emesis for one day. He had an episode of bright red blood per rectum at the outside hospital. He was hypotensive and hypothermic with a WBC 21.1, hemoglobin 11.2, and lactic acid 20. He was intubated due to declining GCS. He required initiation of two pressors and broad-spectrum antibiotics. Initial nasogastric tube output was notably dark, and he was started on IV pantoprazole twice daily as well. CTA abdomen was concerning for active hemorrhage in his stomach. Emergent EGD showed a subjectively ischemic greater curvature of the stomach with congested, hemorrhagic, pale, and friable mucosa. Surgical intervention was deferred given patient was an overall poor surgical candidate.
Discussion: Endoscopic findings that are suggestive of gastric ischemia vary based on etiology and whether it’s acute or chronic. Findings may include pale mucosa, congested mucosa, hemorrhagic mucosa, ulcerations, or necrosis. In a case series of fifteen patients, the most common location was the greater curvature of the stomach. Management of gastric ischemia involves nasogastric tube decompression (ischemia can be exacerbated by gastric distension), initiation of a proton pump inhibitor, and interventional radiology or surgery consultation depending on the etiology. Unfortunately, the prognosis of gastric ischemia remains poor despite these measures.

Figure: Figure 1: Initial non-contrast CT AP with normal appearance of the stomach.
Figure 2: CTA AP one day later with active intraluminal contrast extravasation pooling within the depending gastric fundus.
Figure 3: CTA AP demonstrating interval development of intraperitoneal free fluid and colonic distension.
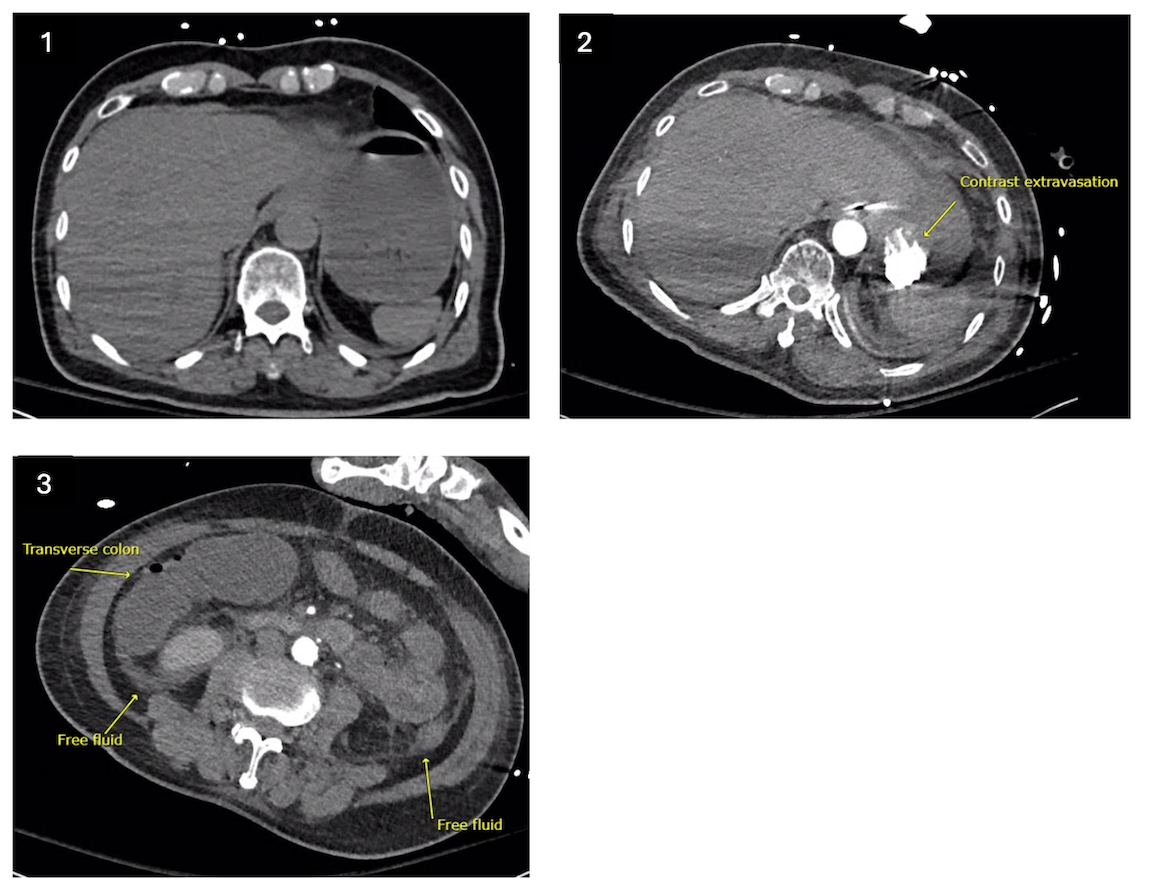
Figure: Figure 4: EGD revealing friable mucosa and hematin in the stomach.
Disclosures:
Stephany Nguyen indicated no relevant financial relationships.
Daniel Holmes indicated no relevant financial relationships.
Stephany Nguyen, MD, Daniel Holmes, MD. P6380 - Gastric Ischemia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
